Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista colombiana de Gastroenterología
Print version ISSN 0120-9957On-line version ISSN 2500-7440
Rev. colomb. Gastroenterol. vol.35 no.2 Bogotá Apr./June 2020
https://doi.org/10.22516/25007440.366
Case report
Actinic colitis of cecal location. Number of cases
1 Departamento de Patología y Laboratorios, Fundación Santa Fe de Bogotá. Bogotá D. C., Colombia
2 Departamento de Patología y Laboratorios, Fundación Santa Fe de Bogotá. Facultad de Medicina, Universidad de los Andes. Bogotá D. C., Colombia
By definition, actinic colitis includes inflammatory changes of the colorectal mucosa secondary to radiation therapy of nearby tissue. The most frequent location is the rectum, and the most common indication for radiation therapy is a pelvic region neoplasm in the rectum, prostate or cervix. It is estimated that up to half of patients receiving pelvic radiation go on to develop associated gastrointestinal symptoms.
We present two patients with sacroiliac and pelvic bone metastases secondary to prostate adenocarcinoma who received radiation in the lumbosacral and pelvic region. Both patients developed bloody stools soon after radiation therapy. Colonoscopy showed erythema and ulceration, and histopathology found a pattern of ischemic colitis with nucleus and cytomegalovirus infection, fibrous stroma with reactive changes and abundant inflammatory infiltration of neutrophils. These findings are characteristic of acute actinic colitis, but the cecal location has not been reported frequently. Nevertheless, the pelvic location of the cecum and the terminal ileum puts these anatomical segments at risk from the direct impact of radiation therapy. In the acute phase, this condition, is self-limiting and usually resolves with support measures. It is essential that the personnel involved in the management of these patients be aware of this entity and its possible differential diagnoses.
Keywords: Colitis; radiotherapy; gastrointestinal bleeding
Por definición, la colitis actínica incluye cambios inflamatorios de la mucosa colorrectal secundarios a radioterapia en cercanía a la región tratada. La localización más frecuente es el recto y la indicación más común de radioterapia corresponde a neoplasias de la región pélvica incluidos el recto, la próstata y el cérvix. Se estima que hasta la mitad de los pacientes que reciben radiación pélvica llega a desarrollar síntomas gastrointestinales asociados. Se presentan dos pacientes con metástasis óseas sacroilíacas y pélvicas secundarias a adenocarcinoma de próstata que recibieron radiación en la región lumbosacra y pélvica, ambos pacientes presentaron episodios de deposiciones con sangre que iniciaron tempranamente posterior a la radioterapia. La colonoscopia mostró eritema y ulceración. En el estudio histopatológico se observó un patrón de colitis isquémica, con núcleo y citomegalia, estroma fibroso con cambios reactivos y abundante infiltrado inflamatorio neutrofílico. Estos hallazgos son característicos de la colitis actínica aguda; sin embargo, la localización cecal no ha sido frecuentemente reportada. Aunque al ser el ciego y el íleon terminal móviles de localización pélvica, se convierten en un factor de riesgo para que estos segmentos anatómicos sean susceptibles al impacto directo de la radioterapia. Esta condición, en la fase aguda, es autolimitada y se suele resolver con medidas de soporte. Es indispensable que el personal involucrado en el manejo de estos pacientes conozca esta entidad y los posibles diagnósticos diferenciales.
Palabras clave: Colitis; radioterapia; hemorragia gastrointestinal
Introduction
Radiation colitis corresponds to inflammatory changes of the colonic mucosa secondary to radiation therapy in the vicinity. 1 This common pathology occurs in up to 50% of patients who receive radiation treatment for abdominal and pelvic malignancies. Usually, patients with cancer of the prostate, cervix and rectum are the most affected, and the regions that are usually involved are the sigmoid colon and the rectum. 2,3 Radiation colitis can be acute or chronic depending on the time of appearance of the lesion with respect to exposure. The acute phase appears within six months of the start of radiation therapy and usually manifests clinically with diarrhea, tenesmus and bleeding. The chronic phase occurs six months after exposure and presents with diarrhea, pain, obstruction, fistulas, and bleeding. Diagnosis conventionally involves colonoscopy and medical history. 3 Colitis due to localized radiation therapy in the cecum is uncommon, and there had been no cases reported in the literature. We present two cases of cecal radiation colitis in patients who were irradiated due to pelvic bone metastases from prostate adenocarcinoma.
Case 1
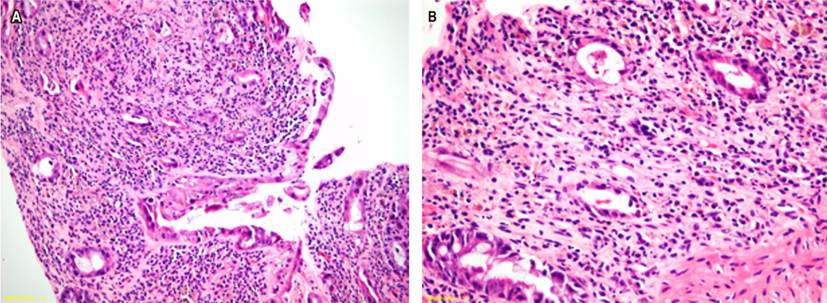
A 75-year-old patient with a history of prostatic adenocarcinoma consulted because of pain in his right hip. An abdominal computerized axial tomography (CT) scan revealed multiple osteoblastic lesions in the patient’s spine, pelvis, and secondary femur which were probably metastatic. Palliative radiation therapy (300 cGy per session) was indicated for the entire pelvic region including the femoral heads. At the end of 10 radiation therapy sessions, the patient presented bloody stools. A colonoscopy showed that the cecal mucosa had mild focal erythema without ulcers or other lesions. Biopsies were taken from this location. The histopathological study (Figure 1) showed a pattern of acute ischemic colitis with reactive changes, loss and miniaturization of glands, cytomegaly and nucleomegaly without alteration of the nucleus-cytoplasm relationship, paucicellular lamina propria with predominantly neutrophilic and superficial inflammatory infiltrate with incipient fibrosis, edema and areas with hemorrhaging without thrombi. Based on these findings, acute radiation colitis was diagnosed and the patient was treated with supportive measures. His subsequent evolution was satisfactory.
Case 2
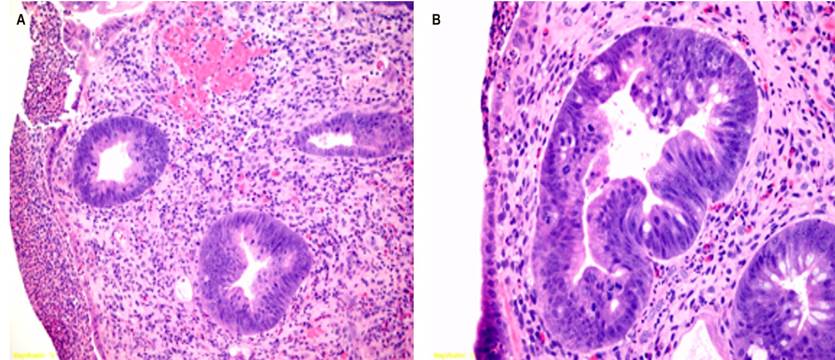
An 85-year-old patient with a diagnosis of metastatic prostate adenocarcinoma in the right lumbar and sacroiliac region consulted due to melena and hematochezia that had begun seven days after completing six radiation therapy treatment of the right lumbar and sacroiliac region (400 cGy per session). A colonoscopy showed that the cecal mucosa had multiple flat, fibrin-covered, ulcerations. A biopsy showed radiation colitis with more serious changes than in the previous case. There was marked architectural distortion, loss and miniaturization of crypts, formation of microabscesses, fibrous stroma with rich eosinophilic polymorphonuclear inflammatory infiltrate, fibroblasts, reactive endothelial cells and regenerative changes including cells with cytomegaly and nucleomegaly without significant alteration of the nucleus-cytoplasm relationship (Figure 2). Based on these findings, acute radiation colitis was diagnosed. The patient received support measures. His subsequent evolution was good.
Discussion
Ionizing radiation is a known cause of intestinal disease. 4 Walsh first reported intestinal damage induced by radiation therapy in 1897, just two years after the discovery of X-rays. 5 Despite advances in radiation therapy techniques, radiation colitis is common after radiation therapy in the pelvic region for gynecological, urological, and anorectal neoplasms. Up to 50% of these patients have reported symptoms. 3,6
Colonoscopy provides information that is essential for diagnosis of radiation colitis. Among the important findings are edema, erythema, friability, ulcers, and necrosis of the mucosa which depend on the degree of inflammation. 7 The first patient reported on here presented erythema in the mucosa while the second presented a higher degree of inflammation and ulcers. Biopsies are not usually necessary to make the diagnosis, but as in these two cases a biopsy may be needed to confirm an endoscopist’s suspicion or because of the patient’s medical history. In some cases biopsies can help exclude other causes of colitis. 3 Differential diagnoses include infections, inflammatory bowel disease, other causes of ischemic-pattern colitis, diverticular disease, and drug-associated colitis. 8
Histopathologically, the patterns of the acute and chronic phases correspond to those of acute and chronic ischemic colitis. In the acute phase, changes are more evident in the epithelium, with cytomegaly, nucleomegaly, pyknosis, karyorrhexis, and abundant mitotic activity with frequent atypical figures. These include miniaturization and loss of crypts, mucin loss with inflammatory infiltrate of the lamina propria with a predominance of neutrophil polymorphonuclear cells and plasma cells and formation of crypt abscesses. In contrast, alterations during the chronic phase are predominantly stromal and include hyalinized connective tissue occupying the lamina propria, reactive atypia in fibroblasts and endothelial cells, obliteration and hyalinization of blood vessels, and atrophy of the muscularis propria. 8
Our patients’ clinical histories, endoscopic findings, and histopathological findings made it possible to orient their diagnoses towards acute radiation colitis.
Even though radiation colitis is most frequently found in the rectum, the pelvic location of the cecum and the terminal ileum place these anatomical segments at risk of direct impact from radiation therapy. It is also important to highlight that the acute phase of the disease is usually self-limiting and resolves with support measures as observed in the two cases presented. 9 In contrast, management of the chronic phase is more complex due to progressive evolution of the disease that includes fibrosis, edema, endarteritis, obstruction, perforation and malignancy. Consequently, different treatments including hyperbaric oxygen, endoscopic cauterization and surgery may be required depending on the individual case. 10
Conclusion
Cecal radiation colitis is rare, and our cases are the first to be reported in this location. Both were associated with radiation directed at pelvic metastases. Personnel involved in the care of these patients should consider radiation therapy colitis as a differential diagnosis for patients who present gastrointestinal bleeding after radiation therapy for primary or metastatic neoplasms. Knowledge of this entity can lead to timely diagnosis which will help prevent complications and reduce short-term and long-term morbidity in these patients.
Referencias
1. Qadeer M, Vargo J. Approaches to the prevention and management of radiation colitis. Curr Gastroenterol Rep. 2008;10(5):507-13. https://doi.org/10.1007/s11894-008-0093-9 [ Links ]
2. Kennedy, G. Heise C. Radiation colitis and proctitis. Clin Colon Rectal Surg. 2007;20(1):64-72. https://doi.org/10.1055/s-2007-970202 [ Links ]
3. Sarin A, Safar B. Management of radiation proctitis. Gastroenterol Clin N Am. 2013;42(4):913-25. https://doi.org/10.1016/j.gtc.2013.08.004 [ Links ]
4. Leupin N, Curschmann J, Kranzbühler H, Maurer CA, Laissue JA, Mazzucchelli L. Acute radiation colitis in patients treated with short-term preoperative radiotherapy for rectal cancer. Am J Surg Pathol. 2002;26(4):498-504. https://doi.org/10.1097/00000478-200204000-00013 [ Links ]
5. Theis VS, Sripadam R, Ramani V, Lal S. Chronic radiation enteritis. Clin Oncol (R Coll Radiol). 2010;22(1):70-83. https://doi.org/10.1016/j.clon.2009.10.003 [ Links ]
6. Sinkó D, Baranyai Z, Nemeskéri C, Teknos D, Jósa V, Hegedus L, Mayer A. Symptoms, diagnosis and treatment of radiation-induced enteritis. Orv Hetil. 2010;151(36):1450-4. https://doi.org/10.1556/OH.2010.28939 [ Links ]
7. Kennedy GD, Heise CP. Radiation colitis and proctitis. Clin Colon Rectal Surg. 2007;20:64-72. https://doi.org/10.1055/s-2007-970202. [ Links ]
8. Mollà M, Biete A, Piqué J, Panés J. Lesiones intestinales de la radioterapia. Gastroenterol Hepatol. 2001;24(9):454-60. https://doi.org/10.1016/S0210-5705(01)79002-4 [ Links ]
9. Watanabe JM, Surawicz CM. Colitis: pseudomembranous, microscopic, and radiation. En: McNally Peter R. ed. GI/Liver Secrets Plus. 4th Edition, Elsevier; 2010. Chapter 50. p. 349-54. https://doi.org/10.1016/B978-0-323-06397-5.00050-2. [ Links ]
10. Kountouras J, Zavos C. Recent advances in the management of radiation colitis. World J Gastroenterol. 2008;14(48):7289-301. https://doi.org/10.3748/wjg.14.7289 [ Links ]
Received: February 12, 2019; Accepted: April 30, 2019











 text in
text in