Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista colombiana de Gastroenterología
Print version ISSN 0120-9957On-line version ISSN 2500-7440
Rev. colomb. Gastroenterol. vol.35 no.2 Bogotá Apr./June 2020
https://doi.org/10.22516/25007440.559
Letter
Evidence of gastrointestinal disturbances in COVID-19: manifestations and theories in pathophysiology
1 Médico. Investigador, Centro de Investigaciones Biomédicas; Cartagena, Colombia
2 Médico interno. Universidad de Cartagena; Turbaco, Colombia
3 Médico. Hospital Naval; Cartagena, Colombia
4 Médico. Investigador, Centro de Diagnóstico Cardiológico; Arjona, Colombia
5 Médico. Unidad Integral del San Jorge; Sahagún (Córdoba), Colombia
6 Médico PhD en Hepatología y Gastroenterología. Centro médico Gastropack; Cartagena. Colombia
SARS-CoV-2, a new virus, emerged in December 2019 in Wuhan, China. It belongs to the coronavirus family and has produced an outbreak of acute respiratory infection, the main clinical presentations of which range from mild respiratory symptoms to severe pneumonia and sepsis. Due to its rapid spread around the world, and the fact that it causes thousands of deaths, the World Health Organization (WHO) has classified it as a pandemic. 1
Studies of SARS-CoV and MERS-CoV, whose infection peaks occurred in 2003 and 2012, have demonstrated that these viruses can potentially invade the human digestive system. 2 MERS-CoV uses dipeptidyl peptidase-4 receptors in the intestinal epithelium for cellular infection which causes inflammation and degradation of this epithelium. 2
On the other hand, SARS-CoV uses angiotensin converting enzyme II (ACEII) as the receptor for entry into cells and infection of the body. This mechanism has been same proposed for SARS-CoV-2 as well. 2 This hypothesis may be strengthened by the results of Zhang et al. whose genetic analysis has identified the expression of ACE II in various areas of the digestive tract including the esophagus, stomach, ileum and colon. 1,3.
The ileum and the colon are the places in which greatest expression of ACE II occurs, surpassing even its expression in the lungs. The main effects occur in absorbent enterocytes. When invaded by SARS CoV-2, they produce alterations in absorption and other mechanisms that lead to diarrhea. 1,3
In addition, transmembrane protease serine 2, an important enzyme widely expressed at these sites in the gastrointestinal tract, 3,4 facilitates infection by proteolytic cleavage of ACE2 receptor which promotes viral uptake, and cleavage of coronavirus spike glycoproteins which activates the glycoprotein for host cell entry. Thus, after the virus enters the cell its RNA begins to replicate which produces new virions which are released into the gastrointestinal tract. This theory has been confirmed by detection of SARS-CoV-2 RNA in stool samples up to 5 weeks after the results of respiratory samples are negative. This suggests that the fecal-oral route is a potential transmission mechanism. 5,6
It has also been documented that viral infections including with SARS-CoV are related to greater permeability of lipopolysaccharides and migration of intestinal bacteria which alters the lung-intestine axis. This could be immunologically involved in respiratory and digestive effects given the alteration of the microbiota of these systems. This theory may be applicable to SARS-CoV-2 because of its similarities to SARS-CoV. 1,3,7.
In general, patients with the 2019 coronavirus disease (Coronavirus Disease 2019, COVID-19) often develop a fever and respiratory tract involvement. 8,9 However, gastrointestinal symptoms including s diarrhea, anorexia, nausea, vomiting, abdominal pain and even gastrointestinal bleeding have been reported in infected patients. 10-12
A retrospective study by Luo et al. that included 1,141 patients from January 1 to February 20, 2020 found that 16% (183) of these patients had gastrointestinal symptoms including loss of appetite (180), nausea (134), vomiting (119) and diarrhea (68) as their main symptoms. 9
This is consistent with a retrospective clinical study and case review by Tian et al. which found that loss of appetite was the most common gastrointestinal symptom in adults but that vomiting was the most common in the pediatric population. However, when both groups were analyzed together, diarrhea stood out as the main finding. 8
Similarly, a study by Guan et al. conducted from December 11, 2019 to January 29, 2020 and including a cohort of 1,099 patients from 552 hospitals in 31 provinces and municipalities in China tried to characterize the first patients diagnosed at the beginning of the COVID-19 outbreak. They documented nausea and vomiting as the main gastrointestinal manifestations. 13
Another study by Lu et al., conducted between January 28 and February 26, identified 171 pediatric patients under the age of 16 who tested positive for the virus. Fifteen suffered from diarrhea while 11 suffered from vomiting. 14
Notably, gastrointestinal symptoms have also been reported in pregnant women. A study by Chen et al. found that of 112 patients diagnosed with COVID-19, eight developed diarrhea. 15
Zhang et al. found that diarrhea and vomiting appeared approximately 5 days after presentation of the first symptoms of COVID-19 in adult patients and persisted for 4 days on average. 16 Other gastrointestinal manifestations also reported by Zhang et al. in another study include abdominal pain in eight of the 139 patients analyzed. 17
Although each of these symptoms may seem harmless, a retrospective observational study of 52 critically ill patients by Yang et al. has shown that 6% developed digestive tract bleeding raising the question of whether the infection caused the bleeding or if it worsened underlying conditions. 18 This is also related to the observation of another of hemoptysis in 5% of COVID-19 patients. 10
In addition to gastrointestinal tract disorders, evidence suggests that the liver may also be affected although but this be due to concomitant factors such as antiviral agents and pre-existing conditions. Short term results have been inconclusive and long term evaluations have yet to conclude. 19
The literature reports growing numbers of unusual and asymptomatic presentations of COVID-19. This provides better information for detection of possible cases. Gastrointestinal symptoms vary among populations, and extrapulmonary manifestations may appear before the characteristic respiratory symptoms associated with this infection.
Yang et al. reported the case of a 62-year-old male patient with a history of hypertension, diabetes, and hyperlipidemia who was admitted to the hospital with a clinical picture of diarrhea and fever before respiratory symptoms developed. This patient’s presentation was atypical presentation for this disease. 20
Similarly, the only respiratory symptom of a 53-year-old male patient with a history of epilepsy and a clinical picture of fever, malaise, and swelling was a dry cough despite the presence of a ground glass pattern in the lower part of the lobe of the left lung. 21
Nevertheless, gastrointestinal symptoms can appear throughout the course of this disease, even after respiratory symptoms appear. An example is the case of a patient who consulted for unquantified fever and four days of coughing who later developed nausea, vomiting, diarrhea, and abdominal discomfort. 22
Patients may also develop alterations of both the respiratory and gastrointestinal systems, as reported by Azwar et al. They documented the case of a patient who consulted for chest and epigastric pain as well as respiratory distress, nausea and vomiting. 23 This may cast doubt about which factors specifically influence the effects on each system.
In summary, it is speculated that the gastrointestinal system is another that is organ directly affected by SARS-CoV-2. Health care professionals should consider a diagnosis atypical presentation of COVID-19 when extrapulmonary symptoms occur. Furthermore, evidence of viral RNA in the feces of apparently recovered patients can guide the creation of protocols for managing biological residues of these patients in order to avoid possible fecal-oral contagion.
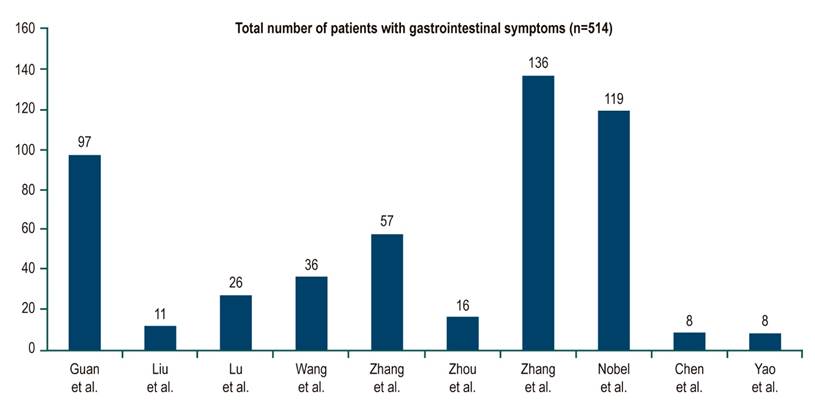
Table 1 and Figure 1 provide details regarding studies of gastrointestinal manifestations in patients with COVID-19. 13,14,24-28
Referencias
1. Musa S. Hepatic and gastrointestinal involvement in coronavirus disease 2019 (COVID-19): What do we know till now? Arab J Gastroenterol. 2020;21(1):3‐8. http://doi.org/10.1016/j.ajg.2020.03.002 [ Links ]
2. Yeo C, Kaushal S, Yeo D. Enteric involvement of coronaviruses: is faecal-oral transmission of SARS-CoV-2 possible? Lancet Gastroenterol Hepatol. 2020;5(4):335‐337. http://doi.org/10.1016/S2468-1253(20)30048-0 [ Links ]
3. Zhang H, Kang Z, Gong H, Xu D, Wang J, Li Z, Li Z, Cui X, Xiao J, Zhan J, Meng T, Zhou W, Liu J, Xu H. Digestive system is a potential route of COVID-19: an analysis of single-cell coexpression pattern of key proteins in viral entry process. Gut. 2020;69(6):1010‐1018. http://doi.org/10.1136/gutjnl-2020-320953 [ Links ]
4. Hoffmann M, Kleine-Weber H, Schroeder S, Krüger N, Herrler T, Erichsen S, Schiergens T, Herrler G, Wu NH, Nitsche A, Müller MA, Drosten C, Pöhlmann S. SARS-CoV-2 Cell Entry Depends on ACE2 and TMPRSS2 and Is Blocked by a Clinically Proven Protease Inhibitor. Cell. 2020;181(2):271‐280.e8. http://doi.org/10.1016/j.cell.2020.02.052 [ Links ]
5. Wu Y, Guo C, Tang L, Hong Z, Zhou J, Dong X, Yin H, Xiao Q, Tang Y, Qu X, Kuang L, Fang X, Mishra N, Lu J, Shan H, Jiang G, Huang X. Prolonged presence of SARS-CoV-2 viral RNA in faecal samples. Lancet Gastroenterol Hepatol . 2020;5(5):434‐435. http://doi.org/10.1016/S2468-1253(20)30083-2 [ Links ]
6. Xiao F, Tang M, Zheng X, Liu Y, Li X, Shan H. Evidence for Gastrointestinal Infection of SARS-CoV-2. Gastroenterology. 2020;158(6):1831‐1833.e3. http:/doi.org/10.1053/j.gastro.2020.02.055 [ Links ]
7. He Y, Wen Q, Yao F, Xu D, Huang Y, Wang J. Gut -lung axis: The microbial contributions and clinical implications. Crit Rev Microbiol. 2017;43(1):81‐95. http://doi.org/10.1080/1040841X.2016.1176988 [ Links ]
8. Tian Y, Rong L, Nian W, He Y. Review article: gastrointestinal features in COVID-19 and the possibility of faecal transmission. Aliment Pharmacol Ther. 2020;51(9):843‐851. http://doi.org/10.1111/apt.15731 [ Links ]
9. Luo S, Zhang X, Xu H. Don’t Overlook Digestive Symptoms in Patients With 2019 Novel Coronavirus Disease (COVID-19). Clin Gastroenterol Hepatol. 2020;18(7):1636‐1637. http://doi.org/10.1016/j.cgh.2020.03.043 [ Links ]
10. Liang W, Feng Z, Rao S, Xiao C, Xue X, Lin Z, Zhang Q, Qi W. Diarrhoea may be underestimated: a missing link in 2019 novel coronavirus. Gut . 2020;69(6):1141-1143. http://doi.org/10.1136/gutjnl-2020-320832 [ Links ]
11. Gu J, Han B, Wang J. COVID-19: Gastrointestinal Manifestations and Potential Fecal-Oral Transmission. Gastroenterology . 2020;158(6):1518‐1519. http://doi.org/10.1053/j.gastro.2020.02.054 [ Links ]
12. Pan L, Mu M, Yang P, Sun Y, Wang R, Yan J, Li P, Hu B, Wang J, Hu C, Jin Y, Niu X, Ping R, Du Y, Li T, Xu G, Hu Q, Tu L. Clinical Characteristics of COVID-19 Patients With Digestive Symptoms in Hubei, China: A Descriptive, Cross-Sectional, Multicenter Study. Am J Gastroenterol. 2020;115(5):766-773. http://doi.org/ 10.14309/ajg.0000000000000620 [ Links ]
13. Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, Liu L, Shan H, Lei CL, Hui DS, Du B, Li LJ, Zeng G, Yuen KY, Chen RC, Tang CL, Wang T, Chen PY, Xiang J, Li SY, Wang JL, Liang ZJ, Peng YX, Wei L, Liu Y, Hu YH, Peng P, Wang JM, Liu JY, Chen Z, Li G, Zheng ZJ, Qiu SQ, Luo J, Ye CJ, Zhu SY, Zhong NS; China Medical Treatment Expert Group for Covid-19. Clinical Characteristics of Coronavirus Disease 2019 in China. N Engl J Med. 2020;382(18):1708-1720. http://doi.org/10.1056/NEJMoa2002032 [ Links ]
14. Lu X, Zhang L, Du H, Zhang J, Qu J, Zhang W, Wang Y, Bao S, Li Y, Wu C, Liu H, Liu D, Shao J, Peng X, Yang Y, Liu Z, Xiang Y, Zhang F, Silva RM, Pinkerton KE, Shen K, Xiao H, Xu S, Wong GW; Chinese Pediatric Novel Coronavirus Study Team. SARS-CoV-2 Infection in Children. N Engl J Med . 2020;382(17):1663‐1665. http://doi.org/10.1056/NEJMc2005073 [ Links ]
15. Chen L, Li Q, Zheng D, Jiang H, Wei Y, Zou L, Feng L, Xiong G, Sun G, Wang H, Zhao Y, Qiao J. Clinical Characteristics of Pregnant Women with Covid-19 in Wuhan, China. N Engl J Med . 2020;NEJMc2009226. http://doi.org/10.1056/NEJMc2009226 [ Links ]
16. Zhang Y. Gastrointestinal tract symptoms in coronavirus disease 2019: Analysis of clinical symptoms in adult patients. medRxiv. 2020;127. https://doi.org/10.1101/2020.03.23.20040279 [ Links ]
17. Zhang JJ, Dong X, Cao YY, Yuan YD, Yang YB, Yan YQ, Akdis CA, Gao YD. Clinical characteristics of 140 patients infected with SARS-CoV-2 in Wuhan, China. Allergy. 2020;10.1111/all.14238. http://doi.org/10.1111/all.14238 [ Links ]
18. Yang X, Yu Y, Xu J, Shu H, Xia J, Liu H, Wu Y, Zhang L, Yu Z, Fang M, Yu T, Wang Y, Pan S, Zou X, Yuan S, Shang Y. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med. 2020;8(5):475-481. http://doi.org/10.1016/S2213-2600(20)30079-5 [ Links ]
19. Young BE, Ong SWX, Kalimuddin S, Low JG, Tan SY, Loh J, Ng OT, Marimuthu K, Ang LW, Mak TM, Lau SK, Anderson DE, Chan KS, Tan TY, Ng TY, Cui L, Said Z, Kurupatham L, Chen MI, Chan M, Vasoo S, Wang LF, Tan BH, Lin RTP, Lee VJM, Leo YS, Lye DC; Singapore 2019 Novel Coronavirus Outbreak Research Team. Epidemiologic Features and Clinical Course of Patients Infected With SARS-CoV-2 in Singapore. JAMA. 2020;323(15):1488-94. http://doi.org/10.1001/jama.2020.3204 [ Links ]
20. Yang X, Zhao J, Yan Q, Zhang S, Wang Y, Li Y. A case of COVID-19 patient with the diarrhea as initial symptom and literature review. Clin Res Hepatol Gastroenterol. 2020:S2210-7401(20)30085-1. http://doi.org/10.1016/j.clinre.2020.03.013 [ Links ]
21. Blanco-Colino R, Vilallonga R, Martín R, Petrola C, Armengol M. Suspected acute abdomen as an extrapulmonary manifestation of Covid-19 infection. Cir Esp. 2020;98(5):295-296. http://doi.org/10.1016/j.ciresp.2020.03.006 [ Links ]
22. Holshue ML, DeBolt C, Lindquist S, Lofy KH, Wiesman J, Bruce H, Spitters C, Ericson K, Wilkerson S, Tural A, Diaz G, Cohn A, Fox L, Patel A, Gerber SI, Kim L, Tong S, Lu X, Lindstrom S, Pallansch MA, Weldon WC, Biggs HM, Uyeki TM, Pillai SK; Washington State 2019-nCoV Case Investigation Team. First Case of 2019 Novel Coronavirus in the United States. N Engl J Med . 2020;382(10):929-936. http://doi.org/ 10.1056/NEJMoa2001191 [ Links ]
23. Azwar MK, Kirana F, Kurniawan A, Handayani S, Setiati S. Gastrointestinal Presentation in COVID-19 in Indonesia: A Case Report. Acta Med Indones. 2020;52(1):63-7. [ Links ]
24. Liu K, Fang YY, Deng Y, Liu W, Wang MF, Ma JP, Xiao W, Wang YN, Zhong MH, Li CH, Li GC, Liu HG. Clinical characteristics of novel coronavirus cases in tertiary hospitals in Hubei Province. Chin Med J (Engl). 2020;133(9):1025-1031. http://doi.org/10.1097/CM9.0000000000000744 [ Links ]
25. Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, Wang B, Xiang H, Cheng Z, Xiong Y, Zhao Y, Li Y, Wang X, Peng Z. Clinical Characteristics of 138 Hospitalized Patients With 2019 Novel Coronavirus-Infected Pneumonia in Wuhan, China. JAMA . 2020;323(11):1061-9. http://doi.org/10.1001/jama.2020.1585 [ Links ]
26. Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, Xiang J, Wang Y, Song B, Gu X, Guan L, Wei Y, Li H, Wu X, Xu J, Tu S, Zhang Y, Chen H, Cao B. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395(10229):1054-1062. http://doi.org/10.1016/S0140-6736(20)30566-3 [ Links ]
27. Nobel YR, Phipps M, Zucker J, Lebwohl B, Wang TC, Sobieszczyk ME, Freedberg DE. Gastrointestinal Symptoms and COVID-19: Case-Control Study from the United States. Gastroenterology . 2020:S0016-5085(20)30490-X. http://doi.org/10.1053/j.gastro.2020.04.017 [ Links ]
28. Yao Q, Wang P, Wang X, Qie G, Meng M, Tong X, Bai X, Ding M, Liu W, Liu K, Chu Y. A retrospective study of risk factors for severe acute respiratory syndrome coronavirus 2 infections in hospitalized adult patients. Pol Arch Intern Med. 2020;130(5):390-399. http://doi.org/10.20452/pamw.15312 [ Links ]
Received: May 05, 2020; Accepted: May 12, 2020











 text in
text in