Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista colombiana de Gastroenterología
Print version ISSN 0120-9957
Rev Col Gastroenterol vol.35 no.3 Bogotá July/Sept. 2020 Epub Mar 01, 2021
https://doi.org/10.22516/25007440.431
Original article
Budd-Chiari Syndrome: Etiology, management, and outcomes in a study of 35 patients at the Hospital Pablo Tobón Uribe
1Grupo de Gastrohepatología y Facultad de Medicina, Universidad de Antioquia; Medellín, Colombia
2Grupo de Gastrohepatología y Facultad de Medicina. Universidad de Antioquia, Hospital Pablo Tobón Uribe; Medellín, Colombia
Budd-Chiari syndrome (BCS) is a rare disorder characterized by the obstruction of the veins of the liver. Both its presentation and therapeutic management are heterogenous. The following is a retrospective study of patients diagnosed with BCS treated by the hepatology service at the Hospital Pablo Tobón Uribe. The results of the categorical variables are expressed as proportions and the continuous variables as means and ranges. The average age of onset of this disease was 37.7 years and it was not predominant in neither sex. The most common symptoms were abdominal pain (91.4%), ascites (71.4%) and hepatomegaly (60%). Out of 35 patients, 11 (31.4%) had primary hypercoagulability, 7 (20%) had some myeloproliferative disorder, 6 (17.1%) had extrahepatic malignancies —3 with mechanical compression and 3 due to associated hypercoagulability—, and 1 case had a membranous obstruction of the inferior vena cava. 32 patients (91.4%) received anticoagulation as first-line therapy and only 4 were taken to surgery: 2 to angioplasty, 1 to transjugular intrahepatic portosystemic shunt (TIPS) and 1 to orthotopic liver transplantation (OLT). On the other hand, 17 (48.5%) individuals underwent invasive procedures as a second-line therapy, of which 8 (22.8%) underwent angioplasty and stenting, 5 (14.29%) underwent TIPS and 4 needed OLT. The 6 patients who were taken to TIPS did not need liver transplants. Budd-Chiari syndrome remains a rare condition affecting the health of young men and women alike, with a heterogeneous clinical presentation but, in most cases, with a clear trigger where thrombophilic and myeloproliferative disorders predominate. The use of invasive therapeutic measures, especially the early selection of patients who may benefit from TIPS, has changed the natural course and prognosis of this group of patients.
Keywords: Budd-Chiari Syndrome; Hepatic Vein Thrombosis; Thrombosis
El síndrome de Budd-Chiari (Budd-Chiari syndrome, BCS) es una entidad rara, definida por la obstrucción del flujo venoso del hígado y corresponde a una condición heterogénea tanto en presentación como en manejo terapéutico. A continuación, presentamos un estudio retrospectivo de pacientes con diagnóstico de BCS, atendidos por el grupo de hepatología del el Hospital Pablo Tobón Uribe. Los resultados se expresan como proporciones en las variables categóricas y como medias y rangos para las variables continuas. La edad promedio de presentación fue de 37,7 años y no hubo preponderancia por el género. Los principales síntomas fueron dolor abdominal (91,4 %), ascitis (71,4 %) y hepatomegalia (60 %). Asimismo, 11 pacientes (31,4 %) presentaron hipercoagulabilidad primaria, mientras que en 7 (20 %) se encontró algún síndrome mieloproliferativo. Además, 6 (17,1 %) tenían neoplasias extrahepáticas: 3 con compresión mecánica y 3 por hipercoagulabilidad asociada; solo en 1 caso se documentaron membranas en la vena cava inferior. Y en 5 casos no fue posible determinar la causa de trombosis. De igual forma, 32 pacientes (91,4 %) recibieron anticoagulación como primer manejo; solo 4 sujetos fueron remitidos a procedimientos: 2 a angioplastia, 1 a derivación portosistémica intrahepática transyugular (Transjugular Intrahepatic Portosystemic Shunt, TIPS) y 1 a trasplante ortotópico hepático (TOH). Luego de ello, 17 (48,5 %) recibieron procedimientos invasivos como segunda línea: 8 (22,8 %) se condujeron a angioplastia y endoprótesis (stent), 5 (14,29 %) a TIPS y 4 necesitaron TOH. Así, los 6 pacientes que se llevaron a TIPS no necesitaron trasplante hepático. El BCS continúa siendo una condición poco frecuente que afecta la salud de personas jóvenes, tanto hombres como mujeres, con una presentación clínica heterogénea. Sin embargo, en la mayoría de los casos ocurre por una causa desencadenante clara, entre las cuales predominan las trombofilias y los síndromes mieloproliferativos. El uso de medidas terapéuticas invasivas, especialmente de la selección temprana de los enfermos que se benefician de TIPS, ha cambiado la historia natural y el pronóstico de este grupo de pacientes.
Palabras clave: Síndrome de Budd-Chiari; trombosis de la vena hepática; trombosis
Introduction
Budd-Chiari syndrome (BCS) is a rare condition caused by the obstruction of the venous flow of the liver. This obstruction may occur anywhere from the hepatic veins to the inferior vena cava. The incidence of this condition is estimated at 1 case per 2.5 million people per year worldwide 1.
Although this syndrome presents with the classical triad of ascites, abdominal pain, and hepatomegaly, in clinical practice it is evident that it is a heterogeneous condition regarding its presentation and treatment. Patients may have thrombosis associated with primary thrombophilia or a mechanical phenomenon that triggers the obstruction and, in many cases, multiple precipitating factors. Possible treatment choices include anticoagulation and diuretics or invasive radiology procedures, such as thrombolysis, angioplasty or transjugular intrahepatic portosystemic shunt (TIPS), and surgery in the case of portosystemic shunt or liver transplantation 2.
Knowledge about this group of patients is based on small case series, and, in recent years, attempts have been made to standardize diagnostic criteria, prognostic indicators and step-by-step therapeutic modalities based on the possibilities of success 3.
The following is a series of retrospective cases that describe the clinical, biochemical, and imaging features, as well as the treatment plan and outcomes of patients of all ages diagnosed with BCS and treated at the Hospital Pablo Tobón Uribe.
Materials and methods
This is a retrospective cohort study conducted on a population of patients diagnosed with BCS and treated by the hepatology group of the Hospital Pablo Tobón Uribe in Medellín, Colombia, between January 2010 and November 2018.
BCS was defined as the occlusion of the hepatic venous outflow, for any reason, which can occur in the hepatic veins, the inferior vena cava, or both. Such occlusion may be confirmed using imaging tests (Doppler ultrasound, computed tomography, contrast magnetic resonance imaging, or venography).
Patients with microvascular coronary disease (sinusoidal obstruction syndrome), heart failure, or with a previous history of liver transplantation were excluded. In all patients, general demographic variables, comorbidities, etiology of liver disease, form of presentation, severity according to the MELD (model for end-stage liver disease) score and the Rotterdam score, were analyzed, as well as laboratory characteristics, imaging variables, treatment provided, complications and overall survival.
Results are expressed as continuous variables, described as medians and interquartile ranges (IQR), and categorical variables are presented as absolute numbers and percentages.
Results
During the study period, 35 patients met the inclusion criteria. Distribution by sex was very similar: 18 male patients (51.43 %) and 17 female patients (48.57 %). The average age was 39 years (20-46 years) (Table 1).
Table 1 Clinical features
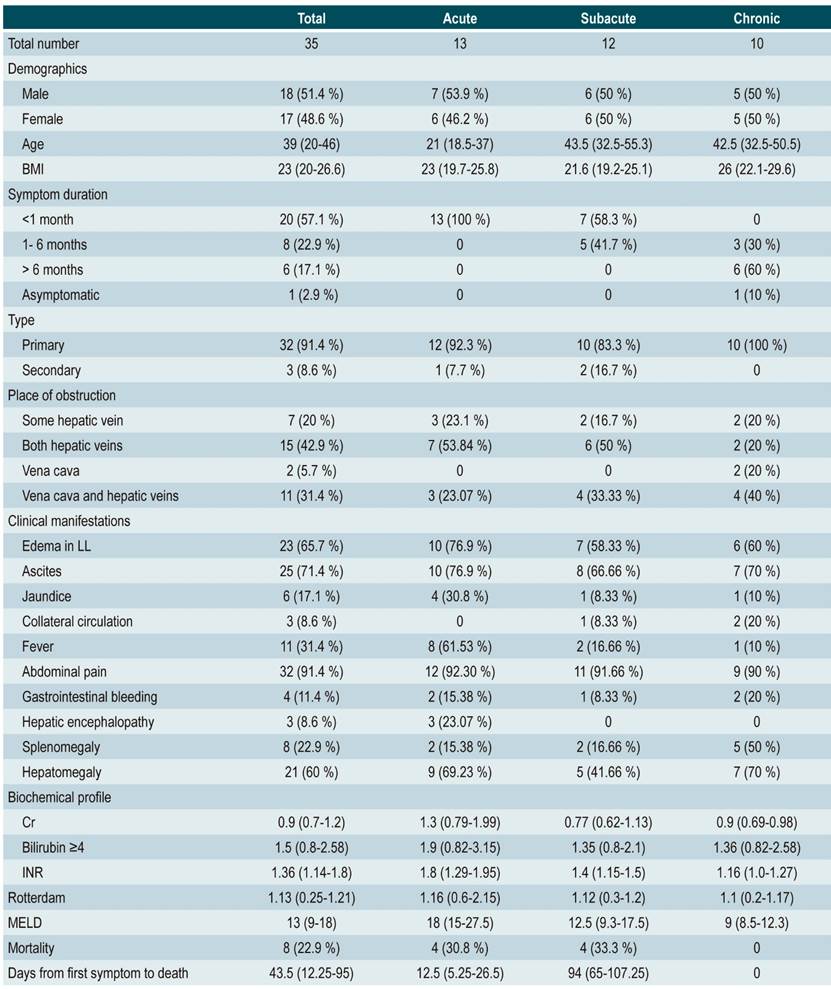
BMI: Body mass index; LL: Lower limbs; INR: International Normalized Ratio; Cr: Creatinine; MELD: Model for End-stage Liver Disease
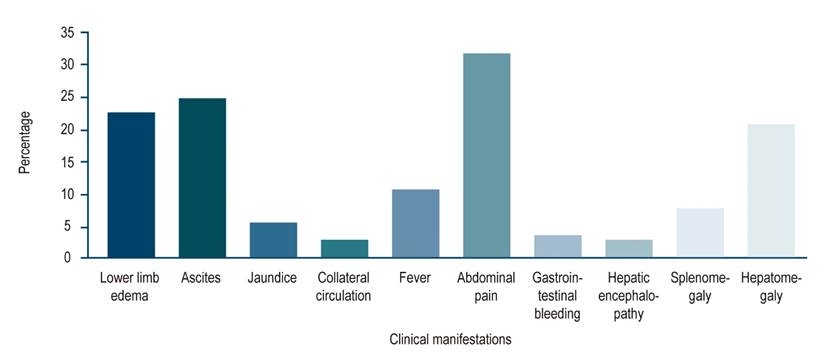
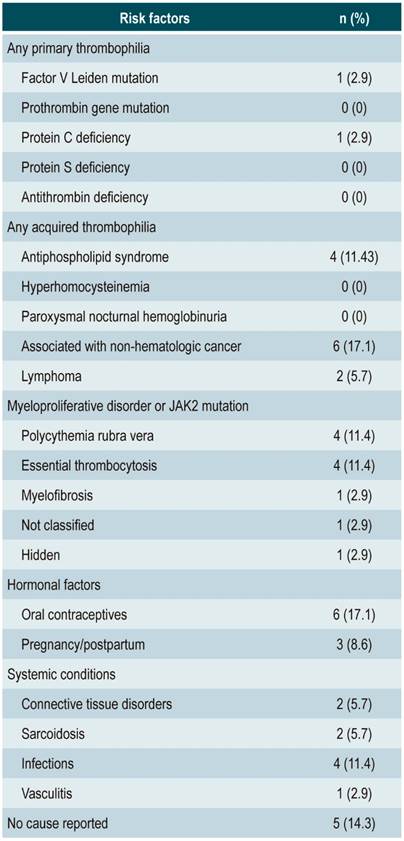
Some of the risk factors found prior to the onset of the condition included 7 patients (20%) with some type of neoplasm; 6 (17%) with a history of oral contraceptive use; 4 (11,4%) with a history of primary hypercoagulability; 2 pregnant women or in their post-partum period; 2 with a history of sarcoidosis; and 2 cases of local or systemic infection. In 12 cases (34.29 %) no risk factor was reported. It should be noted that 4 patients (11,4 %) presented with more than 1 associated risk factor (Table 2). Regarding the clinical presentation and the 3 symptoms classically reported in BCS semiology, 32 patients (91 %) had abdominal pain, 25 (71 %) ascites, and 21 (60 %) hepatomegaly (Figure 1).
Only 13 patients (37.14 %) had acute BCS, of which 3 developed criteria for acute liver failure. The remaining cases were subacute or chronic BCS (Table 1). Regarding the causes reported after the onset of BSC, 11 patients (31.4 %) had primary hypercoagulability, while 7 (20 %) had some type of myeloproliferative disorder. Furthermore, 6 patients (17,1 %) had extrahepatic neoplasms, 3 presented with mechanical compression of the supra-hepatic veins, and 3 presented with associated hypercoagulability. Membranous obstruction of the inferior vena cava was reported in only 1 case.
Moreover, BCS was found to be secondary to active infection (septic thrombosis) in 1 (2.8 %) of the patients, while 4 (11.42 %) of them were classified under other conditions such as hypereosinophilic syndrome (n = 1), BCS secondary to catheter-related thrombosis (n = 1), and hepatic sarcoidosis (n = 2). In the remaining 5 cases (14.28 %), no trigger cause was reported (Table 2). Overall, 32 cases (91. %) were classified as primary cases associated with thrombosis, while only 3 (8.5 %) were secondary to extrinsic mechanical obstruction.
On the other hand, in 15 patients (42,86 %) thrombotic involvement of the 3 suprahepatic veins was reported, and in 11 cases (31,4 %) thrombosis occurred in both the suprahepatic veins and the inferior vena cava. Furthermore, in 7 cases (20 %) there was isolated involvement of some of the suprahepatic veins. In 2 (5.7 %) there was an exclusive involvement of the inferior vena cava (Table 1).
Regarding the treatment plan, 32 patients (91.4 %) received anticoagulant therapy with full treatment doses. About invasive treatment to improve blood flow through the liver, only 5 were initially treated with invasive procedures: 2 with angioplasty and stenting, 1 with TIPS, and one case of orthotopic liver transplant (OLT) (Figure 2).
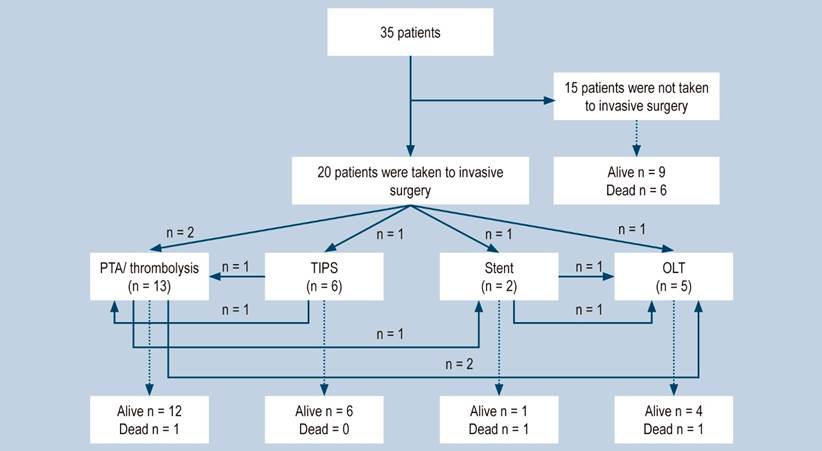
Figure 2 Treatment flowchart. Initially, 1 patient was referred to angioplasty and then received thrombolysis. PTA: percutaneous transluminal angioplasty; TIPS: transjugular intrahepatic portosystemic shunt; OLT: orthotopic liver transplant.
Regarding patients with clinical deterioration or no response to first-line therapy, 17 (485%) underwent invasive procedures, while 8 (22,8%) underwent angioplasty and stenting. In addition, 5 patients (149 %) required TIPS and 4 were taken to OLT (Figure 2). It should be noted that treatment alternatives were defined by the hepathology group and became more complex according to the success of recanalization and decompression. An important finding was that none of the 6 patients who underwent TIPS required liver transplantation.
About the survival of the patients treated by the hepatology service, 8 deaths (228 %) were reported, of which only 3 were directly associated with BCS. In the remaining scenarios, deaths were secondary to the progression of underlying conditions.
Discussion
This is one of the largest series of patients diagnosed with BCS published in our country. Firstly, it was possible to observe that this condition affects mainly young patients, since their average age was around the fourth decade of life, and that there is no sex predominance. These findings are comparable with those reported in other series 4. In Colombia, these characteristics had already been described in case reports 5.
It is worth noting that during medical training, BCS is conceived as an acute and severe condition. However, this type of presentation occurs in only one third of cases (34,29 %); most patients present with subacute or chronic BCS. In our case series study, the cardinal symptoms, as described in classical semiology 5, were abdominal pain (91 %), ascites (71.4 %) and hepatomegaly (60 %). These clinical signs are still valid for reaching a diagnosis.
Hepatic venous outflow tract obstruction occurs more frequently in the suprahepatic vein (42.8 %), although it can also occur simultaneously in the suprahepatic vein and the inferior vena cava (31.4 %). Isolated vein thrombosis (isolated inferior cava or hepatic vein alone) is less common, and most cases (91.4 %) generally are associated with primary causes of thrombosis; extrinsic obstructions were very rare 6.
As reported in previous case series, BCS is associated with primary or acquired thrombophilia and myeloproliferative disorders 6. In the present study, it was not possible to identify the cause of thrombosis in only 5 cases, and some patients had multiple etiologies. Nevertheless, since this is a retrospective study, it is not possible to assure that in all patients the protocol to search for thrombophilia used was the same or that laboratory samples were collected properly at the moment anticoagulation was started.
The most recent studies have proposed and proved, the most efficient treatment to change the prognosis of these patients is definitely one in which decompression and recanalization of the hepatic outflow tract is achieved 7. In our study, 20 patients underwent invasive procedures, which became more complex progressively according to their clinical and biochemical response. It should be noted that this intervention was not carried out based on the guidelines validated by the European Association for the Study of the Liver 8, but rather it was more a methodical clinical judgment exercise that was performed using the tools available at the time.
Since 2013, we have been stricter in including risk scores to predict therapeutic success and in assessing response earlier, so as not to delay the use of definitive invasive measures that improve prognosis 9. Still, the most important treatment finding is the outstanding result achieved in patients who were taken to TIPS. Despite the few cases, this result is consistent with what is described in current studies 8,10.
A large part of the treatment alternatives exposed here are not available at all levels of care in the Colombian health system, and most health centers will certainly only have anticoagulation, and even thrombolysis, available. However, it is evident, both in this case series and in larger reports conducted worldwide, that the successful treatment of patients with BCS currently depends on early interventions, as well as on the use of scores that can predict the success of therapies. Another relevant aspect is the selection of patients who, in advance, with the failure of conventional therapies is known. These patients require relieving liver congestion through TIPS or liver transplantation.
The limitations of this study include its retrospective nature and that only the experience of a single medical center is reported. Furthermore, the availability of diagnostic and therapeutic tests was not the same for all patients in the study period. Treatment plans were not standardized for anticoagulation and thrombolysis. Also, in the acute phase, most patients received low molecular weight heparins and conventional thrombolytics.
However, some conclusions can be drawn from the results of this series. BCS remains a rare condition, affecting the health of young people, both men and women, with a heterogeneous clinical presentation. In most cases, this condition occurs because there is a clear trigger, particularly thrombophilia and myeloproliferative disorders. The use of invasive therapeutic measures, especially the early selection of patients who may benefit from TIPS, has changed the natural history and prognosis of this group of patients.
REFERENCES
1. Valla DC. The diagnosis and management of the Budd-Chiari syndrome: consensus and controversies. Hepatology. 2003;38(4):793-803. http://doi.org/10.1053/jhep.2003.50415 [ Links ]
2. DeLeve LD, Valla DC, Garcia-Tsao G; American Association for the Study Liver Diseases. Vascular disorders of the liver. Hepatology. 2009;49(5):1729-1764. http://doi.org/10.1002/hep.22772 [ Links ]
3. Xue H, Li YC, Shakya P, Palikhe M, Jha RK. The role of intravascular intervention in the management of Budd-Chiari syndrome. Dig Dis Sci. 2010;55(9):2659-2663. http://doi.org/10.1007/s10620-009-1087-7 [ Links ]
4. Darwish Murad S, Plessier A, Hernandez-Guerra M, Fabris F, Eapen CE, Bahr MJ, Trebicka J, Morard I, Lasser L, Heller J, Hadengue A, Langlet P, Miranda H, Primignani M, Elias E, Leebeek FW, Rosendaal FR, Garcia-Pagan JC, Valla DC, Janssen HL; EN-Vie (European Network for Vascular Disorders of the Liver). Etiology, management, and outcome of the Budd-Chiari syndrome. Ann Intern Med. 2009;151(3):167-75. http://doi.org/10.7326/0003-4819-151-3-200908040-00004 [ Links ]
5. Ramírez AC, Correa S, Espinoza YP, Marín JI, Muñoz O, Santos O, Hoyos S, Guzmán C, Mena A, Restrepo JC. Síndrome de Budd Chiari: Reporte de tres casos y revisión de la literatura. Rev Col Gastroenterol. 2014;29(3):281-284. [ Links ]
6. Okuda H, Yamagata H, Obata H, Iwata H, Sasaki R, Imai F, Okudaira M, Ohbu M, Okuda K. Epidemiological and clinical features of Budd-Chiari syndrome in Japan. J Hepatol. 1995;22(1):1-9. http://doi.org/10.1016/0168-8278(95)80252-5 [ Links ]
7. Attwell A, Ludkowski M, Nash R, Kugelmas M. Treatment of Budd-Chiari syndrome in a Liver Transplant Unit, the role of transjugular intrahepatic porto-systemic shunt and liver transplantation. Aliment Pharmacol Ther. 2004;20(8):867-73. https://doi.org/10.1111/j.1365-2036.2004.02190.x [ Links ]
8. Seijo S, Plessier A, Hoekstra J, Dell’era A, Mandair D, Rifai K, Trebicka J, Morard I, Lasser L, Abraldes JG, Darwish Murad S, Heller J, Hadengue A, Primignani M, Elias E, Janssen HL, Valla DC, Garcia-Pagan JC; European Network for Vascular Disorders of the Liver. Good long-term outcome of Budd-Chiari syndrome with a step-wise management. Hepatology. 2013;57(5):1962-8. http://doi.org/10.1002/hep.26306 [ Links ]
9. Qi X, Ren W, Wang Y, Guo X, Fan D. Survival and prognostic indicators of Budd-Chiari syndrome: A systematic review of 79 studies. Expert Rev Gastroenterol Hepatol. 2015;9(6):865-875. https://doi.org/10.1586/17474124.2015.1024224 [ Links ]
10. García-Pagán JC, Heydtmann M, Raffa S, Plessier A, Murad S, Fabris F, Vizzini G, Gonzales Abraldes J, Olliff S, Nicolini A, Luca A, Primignani M, Janssen HL, Valla D, Elias E, Bosch J; Budd-Chiari Syndrome-Transjugular Intrahepatic Portosystemic Shunt Group. TIPS for Budd-Chiari syndrome: long-term results and prognostics factors in 124 patients. Gastroenterology. 2008;135(3):808-15. http://doi.org/10.1053/j.gastro.2008.05.051 [ Links ]
Citation: Muñoz-Maya O, Vergara-Cadavid JA, Cajiao-Castro L, Santos OM, Marín-Zuluaga JI, Restrepo-Gutiérrez JC. Budd-Chiari Syndrome: Etiology, management, and outcomes in a study of 35 patients at the Hospital Pablo Tobón Uribe. Rev Colomb Gastroenterol. 2020;35(3):280-286. https://doi.org/10.22516/25007440.431
Received: July 17, 2019; Accepted: October 03, 2019











 text in
text in