Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista colombiana de Gastroenterología
Print version ISSN 0120-9957
Rev Col Gastroenterol vol.35 no.3 Bogotá July/Sept. 2020 Epub Mar 01, 2021
https://doi.org/10.22516/25007440.598
Original article
Restarting care-related activities in the context of COVID-19: Prioritization, protocols, and procedures. Experience of a gastroenterology outpatient unit in Bogotá, Colombia
1Especialista en Medicina Interna, Gastroenterología y Endoscopia Digestiva, Pontificia Universidad Javeriana. Directora médica de Emdiagnóstica S.A.S.; Bogotá, Colombia
2Especialista en Anestesiología y Reanimación, Universidad Nacional de Colombia. Profesor ocasional, Universidad Nacional de Colombia. Anestesiólogo de Emdiagnóstica S.A.S.; Bogotá, Colombia
3Especialista en Medicina Interna, Gastroenterología y Endoscopia Digestiva, Universidad Nacional de Colombia. Gastroenterólogo de Emdiagnóstica S.A.S.; Bogotá, Colombia
4Abogado, Universidad Externado de Colombia. Magíster en Responsabilidad Civil, Universidad Externado de Colombia. Especialista en Economía, Pontificia Universidad Javeriana. Gerente de Core Abogados, grupo asesor de Emdiagnóstica S.A.S.; Bogotá, Colombia
The Colombian Government ordered a mandatory nationwide quarantine in March 2020 due to the spread of the SARS-CoV-2 virus. Since then, outpatient endoscopy units were closed and only urgent procedures were performed in the hospital setting, resulting in a repression of sensitive, priority and elective outpatient endoscopic procedures. The rate of spread of the virus was contained and it did not progress exponentially as in other countries; in the meantime, gastroenterology services were provided in the form of teleconsultation. The mitigation measures and the containment of the virus allowed the Mayor’s Office of Bogotá and the National Government to issue notices with recommendations for the provision of some regulated outpatient services in May 2020, thus creating a window of opportunity to care for patients with sensitive diseases. Under this legal and epidemiological framework, the provision of digestive endoscopy services was restarted at EMDIAGNOSTICA S.A.S. This study presents the strategies for scheduling and performing endoscopic procedures in an outpatient gastroenterology unit during COVID-19 pandemia in Colombia and describes a system for prioritizing procedures according to medical criteria, ranging from care by teleconsultation and/ or an application of a telephone survey and the use of a medically necessary, time-sensitive (MENTS) scale adapted for digestive endoscopy. It also describes changes in infrastructure, methodology implemented for protection of human talent and patients, and post procedure follow-up for feedback, safety and satisfaction degree evaluation in care.
Keywords: SARS-CoV-2; COVID-19; Endoscopy; Quality; Safety; Sedation
La infección por el virus SARS-CoV-2 en Colombia condujo a que el Gobierno decretara una cuarentena total obligatoria en marzo de 2020. En dicho momento, las unidades de endoscopia ambulatoria permanecieron cerradas y solo se efectuaron procedimientos urgentes en el ámbito hospitalario. Esto ocasionó un represamiento de procedimientos endoscópicos sensibles al tiempo, prioritarios y electivos, de realización ambulatoria. La velocidad de propagación del virus se ha contenido, lográndose detener la progresión exponencial observada inicialmente. En dicho contexto, la atención de gastroenterología se ha continuado en la modalidad de teleconsulta. En mayo de este mismo año, el comportamiento de contención epidemiológica permitió que la Alcaldía de Bogotá y el Gobierno nacional emitieran circulares con las recomendaciones para la prestación de algunos servicios ambulatorios reglamentados, y así dar oportunidad de atención a pacientes con enfermedades sensibles al tiempo. Dentro de este marco legal y epidemiológico, se reinició la prestación de servicios de endoscopia digestiva en Emdiagnóstica S.A.S. Por tanto, presentamos aquí las estrategias para la programación y la realización de procedimientos endoscópicos en una unidad ambulatoria de gastroenterología, durante la pandemia por COVID-19 (Coronavirus disease 2019) en Colombia. También se describe un sistema de priorización de procedimientos de acuerdo con el criterio médico, que va desde la atención por teleconsulta o la aplicación de una encuesta telefónica hasta la utilización de una escala MeNTS (Medically Necessary Time-Sensitive) adaptada para endoscopia digestiva. Además, se relatan las adecuaciones en la planta física, la metodología implementada para la protección del talento humano y de los pacientes y el seguimiento posterior a la realización de los procedimientos para retroalimentación, seguridad y evaluación de satisfacción.
Palabras clave: SARS-CoV-2; COVID-19; endoscopia; calidad; seguridad; sedación
Introduction
The Coronavirus Disease 2019 (COVID-19), declared a pandemic by the World Health Organization (WHO) on March 11, 2020 1, substantially changed the way how health care services are delivered to the community and by health care workers. In Colombia, a compulsory lockdown was decreed in March 2020, with the aim of delaying the peak of infections, allowing the hospital network to make the necessary adaptations so as not to collapse 2,3. Isolation protocols were established on March 6 4 after the first case was reported in the country, and they have been adjusted to allow the movement of people and return to work activities, but always considering the security of citizens as a priority 5,6.
However, government guidelines specifically restricted the provision of some non-essential medical services 2,3. Specifically, services provided to diagnose time-sensitive conditions (i.e., in which the time of diagnosis or the start of treatment have a direct impact on prognosis) had to comply with the lockdown and the preventive isolation measures established by the Government while proposing options to continue performing diagnostic procedures that are essential for the prognosis of some diseases without posing a greater risk to health.
Considering that gastrointestinal endoscopies are (or may be) aerosol generating procedures, strategies were developed to reduce the risk of transmission while being performed. After being closed for 7 weeks, the outpatient units were able to restart their services without knowing if they would be suspended again. Consequently, it was necessary to define how to restart these activities and who would undergo these procedures in endoscopy units.
In our unit, once the problem was identified, a strategy began to be planned to deal with the situation. Thus, a multidisciplinary group was created (gastroenterologists, anesthesiologists, lawyers, nurses, and financial advisors) who, through online meetings, established a protocol with recommendations to reactivate the provision of services based on the prioritization scheme described below.
Methodology
Before reopening the unit, a non-systematic search was conducted in the medical literature (Medline-Pubmed, Scielo, Embase, and Google-Scholar) on protocols, clinical practice guidelines, and reports in countries that had already experienced this situation. Moreover, we participated in several virtual conferences and reviewed the decrees issued by government agencies 2,3. It was possible to learn about the measures that had been adopted in this regard worldwide, reproduce the actions that proved to be effective, and modify or adapt those that could be improved.
Multiple international scientific organizations 7-16 designed and socialized guidelines that were reviewed and adapted to our context, since their application had to be adjusted to the needs of an outpatient endoscopy unit that does not provide emergency services. All these contingency measures were planned in accordance with the behavior of COVID-19 in Bogotá.
Legal framework
The Ministry of Health adopted the action plan for the provision of health care services during the pandemic containment and mitigation phases through Resolution 536 of 2020, and, based on it, care plans were structured in the context of the crisis. Thus, in April and May, guidelines were issued for the gradual reopening of services during the health emergency mitigation and control phases. Emphasis was placed on outpatient surgery, surgery with low-risk intensive care unit (ICU) requirement, short hospital stay surgeries, and non-deferrable surgeries.
In update made on June, recommendations regarding outpatient services, surgery, and diagnostic support procedures were eliminated, stating that “care services may be provided, and undifferentiated procedures may be performed in such a way as to guarantee the protection and safety of users and the human talent associated with the provision of such care services.”
Likewise, the Ministry of Health stated that the actions to be followed and the possibility of reactivating the provision of health care services depended on the analysis, in each territory, of factors such as the trend of new cases, the availability of human resources and personal protection equipment (PPE), the use of the installed capacity, and the behavior in the provision of the service. Therefore, the implementation of any reactivation plan must necessarily go through the assessment of the conditions in the territories and the guidelines provided in this regard by the competent authority.
The Health Department of Bogotá issued Notice 029 of April 29, 2020, and Notice 036 of May 12, 2020, which contained recommendations for the operational organization of outpatient services in the context of the COVID-19 pandemic emergency. In said notices, it was concluded that the provision of the health care services in the framework of the health emergency is associated with a dynamism conditioned by the evolution of the pandemic at the territorial level and that, as circumstances evolve, these guidelines will be modified. This process requires constant updating and coordination among the actors involved.
Operational phase
Preparation of administrative and assistance personnel
Individual risk factors were estimated when classifying administrative and healthcare personnel available for on-site care during the pandemic. In addition, the staff was divided into two groups, so that endoscopy services could be provided rotating the staff every two weeks. Agreements and online workshops were made for the adaptation, use and disposal of PPE. Also, PPE necessary to guarantee at least 4 months of operation was acquired.
Furthermore, some documents and procedures necessary to ensure compliance and safe health care services delivery for patients, staff, and the community were adapted, modified, and created (Table 1). Finally, it was agreed that, at the beginning of each day, all staff would make a statement of their health status and risk of COVID-19 (Table 2). All patients would be considered suspected cases and, consequently, protective measures would be the same in all cases.
Table 1 Documents adapted, modified, or created to reactivate activities during the COVID-19 pandemic*
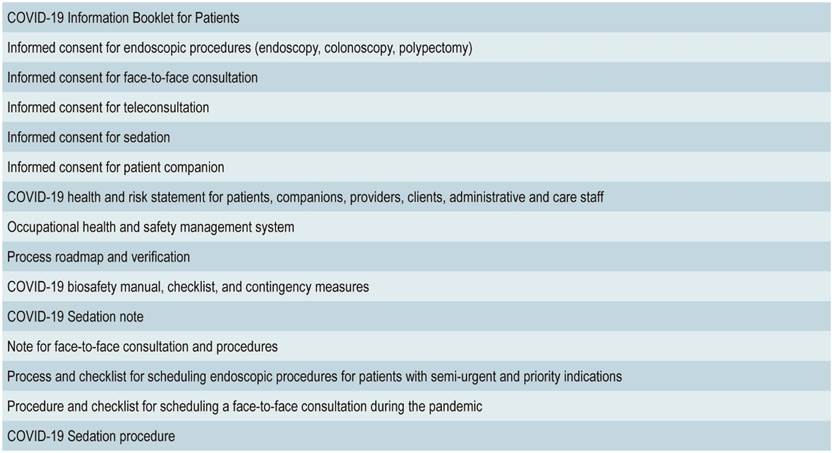
*List of institutional documents from Emdiagnóstica S.A.S., which were adapted, modified, or edited to fit the COVID-19 pandemic scenario. It details the information provided to patients, informed consent forms, organizational documents related to safety and occupational health, protocols created to guide medical care provision, the form with the basic information recorded in the gastroenterology and anesthesiology clinical records, checklists, and roadmaps. COVID-19: Coronavirus Disease 2019
Table 2 Statement of health status and risk of COVID-19*
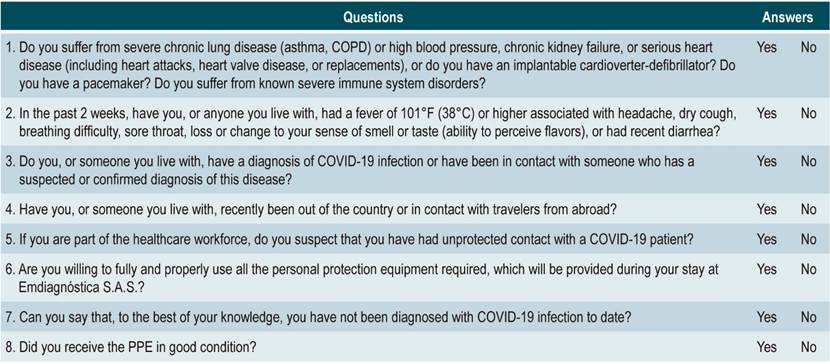
*Form delivered daily, at the beginning of the day, to all the Emdiagnóstica S.A.S. staff to confirm their current state of health and to estimate the risk of COVID-19. Its completion is mandatory. Once the questionnaire has been completed in its entirety, the employee’s body temperature has been taken, the risk of COVID-19 has been confirmed to be low, and the health condition is found to be optimal, the employee is authorized to enter the unit facilities. All forms are stored in the physical archive of Emdiagnóstica S.A.S. COVID-19: Coronavirus Disease 2019; COPD: chronic obstructive pulmonary disease; PPE: personal protective equipment.
Adaptation of the endoscopy unit facilities
Based on the studies by Repici et al. 17, Cennamo et al. 18 and the American Gastroenterological Association (AGA) 10, areas were demarcated according to the degree of exposure to droplets and aerosols, and the unit was equipped with a negative pressure air exchange system (15 cycles every hour) with high efficiency particulate air (HEPA) filters.
Patient selection and procedure scheduling
The provision of the teleconsultation service was established when the preventive lockdown was decreed; in this case, the Government guidelines regarding remote appointments were accepted. This service was used to prioritize the performance of endoscopic procedures. Patient scheduling in this phase was based on national and international recommendations on prioritization, according to the relevance of the study, the health condition of the patient, and the local behavior of the COVID-19 infection curve. Moreover, the recommendations of the Asian-Pacific Society for Digestive Endoscopy (A-PSDE) for an outpatient endoscopy unit 15 were adapted to the local context (Table 3), as well as the suggestions of the AGA 10 regarding the 8-week limit for performing time-sensitive procedures.
Table 3 Performance of endoscopic procedures during the COVID-19 pandemic*
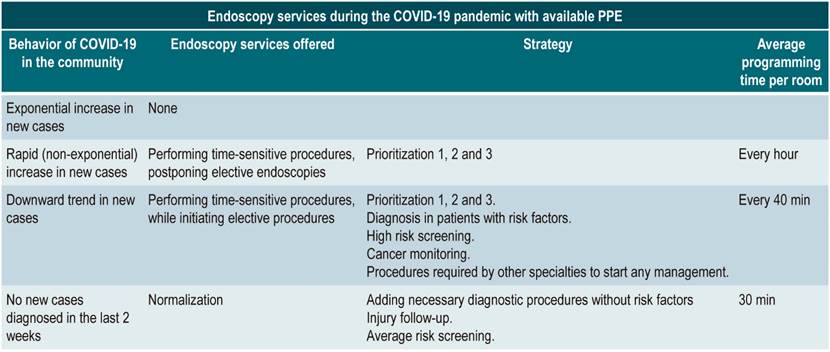
*Strategies used to define the scheduling and performance of endoscopic diagnostic procedures during the COVID-19 pandemic, with available PPE, and considering the behavior of the local epidemiological curve, based on the recommendations of the AGA 10 and the A-PSDE 15. COVID-19: Coronavirus Disease 2019; PPE: personal protective equipment.
Thus, the procedures were scheduled based on the criteria of the gastroenterologist, on the diagnostic probability of having cancer and the presence of alarming symptoms, and on the risk/benefit balance during the pandemic. Three groups were created: priority 1 (procedures that, according to the gastroenterologist, had to be performed within the following two weeks), priority 2 (to be performed within weeks 3 and 4) and priority 3 (to be performed between weeks 5 and 8) (Figure 1). All patients were given recommendations on alarm symptoms that required performing the procedure earlier.
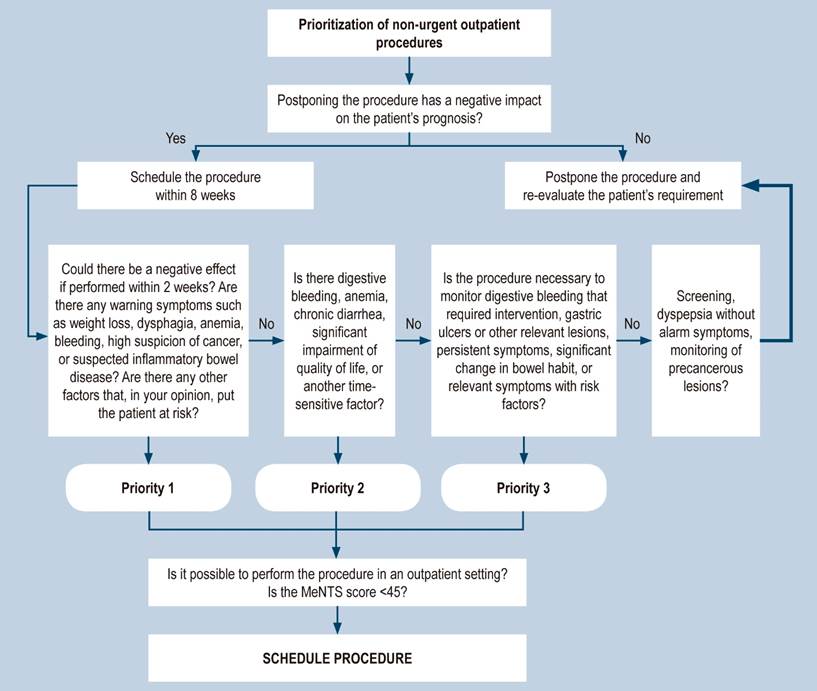
Figure 1 Flow chart for prioritizing endoscopic procedures during the mitigation phase and the rise of the COVID-19 curve. The decision to schedule or not a procedure is based on a judicious clinical evaluation and the determination of the appropriateness of the study during the pandemic period. In addition, the estimation of the MeNTS-ENDOGI score is taken into consideration. MeNTS: Medically Necessary Time-Sensitive score.
The day before assigning the appointment for the procedure and confirming it, the scheduling staff checked again for COVID-19 risk. Meanwhile, in case of referred patients, the procedure was performed, and a checklist was created to schedule prioritized patients (Table 4). When any of the patient’s answers coincided with a warning signal, the patient was scheduled for teleconsultation, during which, besides defining the indication and the time of the procedure, the level of care in the context of COVID-19 was established.
Table 4 Process and checklist for scheduling endoscopic procedures for priority patients*
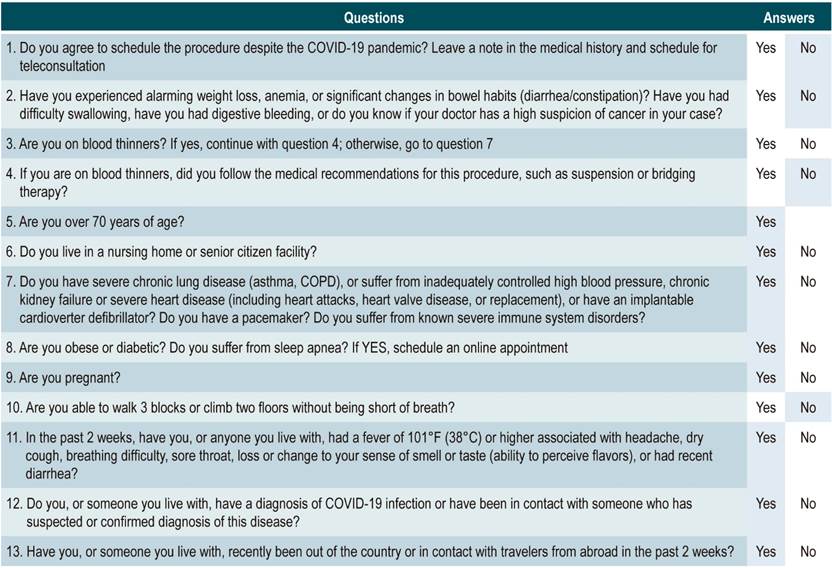
*List of questions asked to each patient by the Emdiagnostica S.A.S. appointment scheduling center by telephone to define whether to schedule the procedure or, failing that (areas shaded in blue), refer the patient to a specialized gastroenterology assessment in the teleconsultation modality to individualize and establish the behavior. This form works as a screening test to classify patients according to their risk and optimize appointment scheduling. COVID-19: Coronavirus Disease 2019; COPD: chronic obstructive pulmonary disease.
The MeNTS-ENDOGI scale was used for this purpose (Figure 2). The version used in the paper by Prachand et al. 19 was adapted, based on adjustments made on the assessed criteria, to apply it in the scenario of endoscopic procedures and achieve objectivity in the decision. The safety of the outpatient environment for the patient was set in up to 45 points. If the score was higher, the recommendation was to refer the patient to a hospital to perform the procedure.
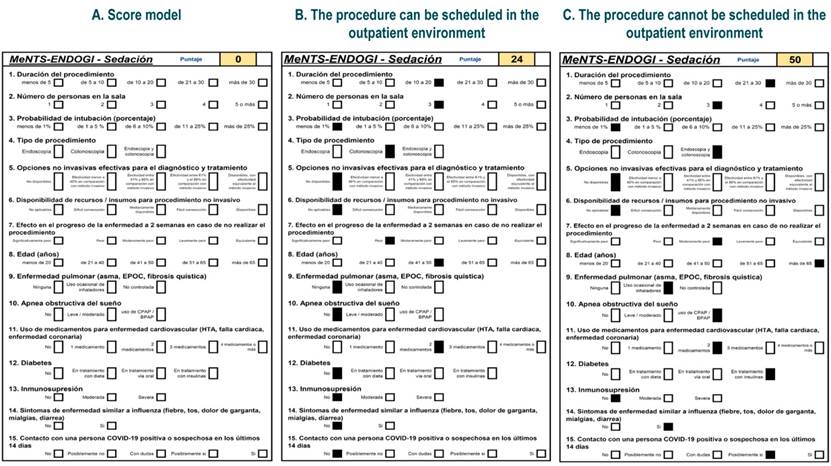
Figure 2 MeNTS-ENDOGI score These schemes represent the scale used by Emdiagnóstica S.A.S. The scale was adapted based on the original MeNTS model by Prachand et al. 19. Panel A shows the blank format before completion. Panel B shows the result after administering the MeNTS-ENDOGI scale to a patient with low risk of complications and dissemination of COVID-19, who can be scheduled for an outpatient procedure. Panel C presents the results of a patient who, due to risk factors (clinical factors and risk of dissemination of COVID-19 infection), cannot be scheduled for an outpatient procedure. Both cases are simulated scenarios and do not disclose information from real patients. Emdiagnóstica S.A.S. set 45 points as the cut-off point to define whether the procedure should be performed in an outpatient or inpatient environment.
Operative phase
Personal protective equipment and biosecurity equipment
The guidelines issued by the American College of Surgeons20, AGA 10, the Ministry of Health and the Colombian Association of Infectiology 11) were followed to establish the use of PPE according to risk areas and activity, including patients (Table 5). Meanwhile, for safe use and disposal of PPE, online training and computer graphics were available in each room. Only PPE delivered by the institution was allowed for use.
Table 5 PPE according to the area of exposure and the task performed*
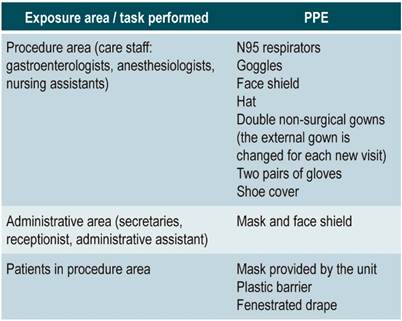
*List of PPE classified according to exposure risk level. For risk assignment, the work area and the task performed by each employee were considered (to determine the degree of exposure to droplets and aerosols). The American College of Surgeons guidelines 20 were used to make this list. PPE: personal protective equipment.
Sedation protocol
All endoscopic procedures are performed in the unit under sedation administered by anesthesiologists. Prior to the pandemic, it was customary to keep patients under moderate sedation according to the Practice Guidelines for Sedation and Analgesia by non-Anesthesiologist 21. Due to the requirement of depth of anesthesia to intubate safely and pass the cricopharyngeus muscle without cough reflex, it was decided to administer the medications conventionally used (remifentanyl and propofol) until this objective was achieved.
However, to reduce prolonged periods of apnea with desaturation and hypoxemia, it was established that all patients would receive routine preoxygenation for 3 min with oxygen by nasal cannula at 2-3 L/min (below the isolation barrier), with deep inspirations. In case the patient’s apnea was accompanied by desaturation (oxygen saturation by pulse oximetry [SpO2] <90 %), the defined action plan was to increase oxygen flow up to 5 L/min and perform maneuvers for airway permeability.
If desaturation persisted, the indication was to suspend the endoscopic procedure and administer oxygen through a well-sealed mask using a two-handed E-C clamp technique to avoid endotracheal intubation or positive pressure ventilation as much as possible. A checklist of complications associated with sedation was adopted 22.
Endoscopic procedures
Patients were scheduled alternately in each of the three available rooms, allowing for ventilation, cleaning, and disinfection of each area prior to the admission of the next patient. This way, despite having negative pressure, each room is used again after 1 hr., initially using 30% of the installed capacity. On the other hand, a plastic barrier is used for endoscopy 23 and a fenestrated drape for colonoscopy. In all cases, the registration of quality indicators for endoscopy and colonoscopy are recorded in the roadmap and verification of processes form, as usual, while the lesions found are resected depending on the characterization of each lesion. In addition, the health care staff changes their external anti-fluid gown for receiving new patients.
Postoperative stage
Follow-up and feedback
A satisfaction survey is administered to all patients for follow-up after the procedure and for monitoring complications after polypectomy between 12-48 hr. and at 7 and 14 days. They are also asked about their satisfaction level and their sense of safety while they were in the unit (Table 6).
Table 6 Questions asked to patients to monitor their condition during the COVID-19 pandemic*
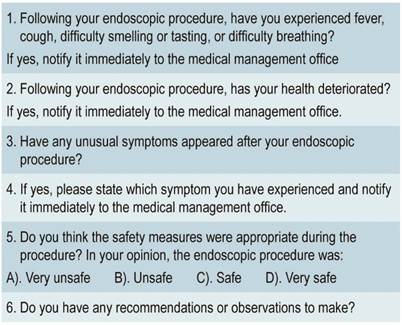
*Questionnaire for telephone follow-up of patients who underwent an endoscopic diagnostic study at Emdiagnóstica S.A.S. Data obtained are used to assess the possible cases of COVID-19 that have been overlooked due to the window period (asymptomatic patients) and to estimate the degree of patient satisfaction with the service received. The level of safety perceived by the patient during their stay at Emdiagnóstica S.A.S. is also evaluated.
Discussion
The mandatory lockdown managed to contain the pandemic’s exponential growth in the country, providing time to avoid the collapse of the ICUs. However, it also led to accumulating an exponential number of non-urgent but time-sensitive procedures that could not be performed due to the closure of outpatient endoscopy units.
Therefore, such procedures were scheduled in the current time window of care to optimize the available resources in the endoscopy units that were prepared to provide safe care services for an uncertain period, which mainly depended on the percentage of ICUs occupation.
The Colombian scenario was different from that of other countries with exponential curves, as they did not implement this containment period. The current pandemic has required leadership and teamwork from health services provision companies to create solutions and evaluate proposals applicable to a new scenario that did not resemble any other country considering the epidemiological behavior.
The adaptations made to our unit have allowed us to provide our services again with 30% of the installed capacity before the epidemiological peak was reached, planning progressive increases according to the descent of the curve. Determining the criteria for the appropriate utilization of the installed capacity, human talent, and inputs, always in line with the local situation, was essential to answer the question: how to resume our activities?
We acknowledge that the COVID-19 pandemic context is dynamic and even unpredictable by presenting this document as a working experience. Based on the proposal of scheduling patients according to the priorities in this window period, we intend to solve the problem of whom to schedule first in order to optimize diagnostic resources and provide timely treatment to impact the prognosis of patients directly.
The results obtained by registering the procedures, monitoring patients, taking actions to reduce contagion risk, and the diagnoses made are subjects that must be considered in further studies. Resuming these activities has made evident the changes in the practice of the specialty, which imply significant challenges for the sustainable operation of endoscopy units.
Likewise, economic aspects such as higher costs and fewer procedures could threaten the stability of health care institutions and independent providers. Filtering, prioritizing, weighting cases based on clinical criteria, and planning expenses carefully has become even more important now, since the legal framework is constantly changing. Our challenge now is to adapt to continue providing sustainable and quality services.
Acknowledgments
To the administrative and health care staff of Emdiagnóstica S.A.S., who are an amazing group of gastroenterologists, anesthesiologists and nursing assistants that strive to follow recommendations, based on a planned management system, to reduce risks and provide safe and quality care.
REFERENCES
1. World Health Organization [internet]. WHO Director-General’s opening remarks at the media briefing on COVID-19 - 11 March 2020: Coronavirus disease (COVID-2019) situation report-50 [actualizada el 11 de marzo de 2020]. Disponible en: Disponible en: https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020 [ Links ]
2. Ministerio de Salud y Protección Social [internet]. Lineamientos de prevención del contagio por COVID-19 y atención en salud para las personas con discapacidad, sus familias, las personas cuidadoras y actores del sector salud. Bogotá: marzo de 2020. Disponible en: Disponible en: https://www.minsalud.gov.co/sites/rid/Lists/BibliotecaDigital/RIDE/DE/PS/asif13-personas-con-discapacidad.covid-19.pdf [ Links ]
3. Ministerio de Salud y Protección Social [internet]. Lineamientos para el manejo clínico de pacientes con infección por nuevo coronavirus COVID-19. Bogotá: julio de 2020. Disponible en: Disponible en: https://www.minsalud.gov.co/Ministerio/Institucional/Procesos%20y%20procedimientos/PSSS03.pdf [ Links ]
4. Ministerio de Salud y Protección Social [internet]. Colombia confirma su primer caso de COVID-19: boletín de prensa [actualizada el 6 de marzo de 2020]. Disponible en: Disponible en: https://www.minsalud.gov.co/Paginas/Colombia-confirma-su-primer-caso-de-COVID-19.aspx [ Links ]
5. Decreto número 636 de 2020. Por el cual se imparten instrucciones en virtud de la emergencia generada por la pandemia del coronavirus COVID-19, y el mantenimiento del orden público (6 de mayo 2020). Ministerio del Interior de la República de Colombia. [ Links ]
6. Presidencia de la República de Colombia [internet]. Aislamiento preventivo obligatorio [consultada el 25 de agosto de 2020]. Disponible en: Disponible en: https://id.presidencia.gov.co/especiales/200323-Aislamiento-Preventivo-Obligatorio/index.html [ Links ]
7. Tse F, Borgaonkar M, Leontiadis GI. COVID-19: Advice from the Canadian Association of Gastroenterology for Endoscopy Facilities, as of March 16, 2020. J Can Assoc Gastroenterol. 2020;3(3):147-149. http://doi.org/10.1093/jcag/gwaa012 [ Links ]
8. American Gastroenterological Association [internet]. Joint GI society message: COVID-19 clinical insights for our community of gastroenterologists and gastroenterology care providers. 2020 [actualizada el 16 de marzo de 2020]. Disponible en: Disponible en: https://gastro.org/press-releases/joint-gi-society-message-covid-19-clinical-insights-for-our-community-of-gastroenterologists-and-gastroenterology-care-providers/ [ Links ]
9. Thompson CC, Shen L, Lee LS. COVID-19 in endoscopy: Time to do more? Gastrointest Endosc. 2020;92(2):435-439. http://doi.org/10.1016/j.gie.2020.03.3848 [ Links ]
10. Sultan S, Lim JK, Altayar O, Davitkov P, Feuerstein JD, Siddique SM, Falck-Ytter Y, El-Serag HB; AGA Institute. AGA Rapid Recommendations for Gastrointestinal Procedures During the COVID-19 Pandemic. Gastroenterology. 2020;159(2):739-758.e4. http://doi.org/10.1053/j.gastro.2020.03.072 [ Links ]
11. Consenso colombiano de atención, diagnóstico y manejo de la infección por SARS-COV-2/COVID-19 en establecimientos de atención de la salud: Recomendaciones basadas en consenso de expertos e informadas en la evidencia. Infectio. 2020;24(3 Suppl 2). [ Links ]
12. Sociedad Española de Endoscopia Digestiva (SEED) [internet]. Recomendaciones de la SEED: protección en unidades de endoscopia frente al COVID-19. 2020 [actualizada el 13 de marzo de 2020]. Disponible en: Disponible en: https://www.wseed.org/~josepr23/sociedades/SEEDv3/images/site/guia_clinica/2020/RecomendacionesSEED_UnidadesEndoscopia_COVID19_v1.pdf [ Links ]
13. Beilenhoff U, Biering H, Blum R, Brljak J, Cimbro M, Dumonceau JM, Hassan C, Jung M, Kampf B, Neumann C, Pietsch M, Pineau L, Ponchon T, Rejchrt S, Rey JF, Schmidt V, Tillett J, van Hooft JE. Reprocessing of flexible endoscopes and endoscopic accessories used in gastrointestinal endoscopy: Position Statement of the European Society of Gastrointestinal Endoscopy (ESGE) and European Society of Gastroenterology Nurses and Associates (ESGENA)-Update 2018. Endoscopy. 2018;50(12):1205-1234. http://doi.org/10.1055/a-0759-1629 [ Links ]
14. Aguila EJT, Lontok MAD, Francisco CPD. Follow Your Gut: Challenges in Nutritional Therapy During the COVID-19 Pandemic. Clin Gastroenterol Hepatol. 2020;S1542-3565(20)30753-9. http://doi.org/10.1016/j.cgh.2020.05.046 [ Links ]
15. Chiu PWY, Ng SC, Inoue H, Reddy DN, Ling Hu E, Cho JY, Ho LK, Hewett DG, Chiu HM, Rerknimitr R, Wang HP, Ho SH, Seo DW, Goh KL, Tajiri H, Kitano S, Chan FKL. Practice of endoscopy during COVID-19 pandemic: position statements of the Asian Pacific Society for Digestive Endoscopy (APSDE-COVID statements). Gut. 2020;69(6):991-996. http://doi.org/10.1136/gutjnl-2020-321185 [ Links ]
16. American Society for Gastrointestinal Endoscopy [internet]. Guidance for resuming GI endoscopy and practice operations after the COVID-19 pandemic. 2020 [actualizada el 28 de abril de 2020]. Disponible en: Disponible en: https://www.asge.org/docs/default-source/default-document-library/asge-guidance-for-reopeningl_4-28-2020.pdf [ Links ]
17. Repici A, Maselli R, Colombo M, Gabbiadini R, Spadaccini M, Anderloni A, Carrara S, Fugazza A, Di Leo M, Galtieri PA, Pellegatta G, Ferrara EC, Azzolini E, Lagioia M. Coronavirus (COVID-19) outbreak: what the department of endoscopy should know. Gastrointest Endosc. 2020;92(1):192-197. http://doi.org/10.1016/j.gie.2020.03.019 [ Links ]
18. Cennamo V, Bassi M, Landi S, Apolito P, Ghersi S, Dabizzi E, Polifemo AM, Gizzi G, Guicciardi S, Indelicato G, Cascone C, Tovoli D, Tumietto F, Viale P, Jovine E, Repici A. Redesign of a GI endoscopy unit during the COVID-19 emergency: A practical model. Dig Liver Dis. 2020. http://doi.org/10.1016/j.dld.2020.05.007 [ Links ]
19. Prachand VN, Milner R, Angelos P, Posner MC, Fung JJ, Agrawal N, Jeevanandam V, Matthews JB. Medically Necessary, Time-Sensitive Procedures: Scoring System to Ethically and Efficiently Manage Resource Scarcity and Provider Risk During the COVID-19 Pandemic. J Am Coll Surg. 2020;231(2):281-288. http://doi.org/10.1016/j.jamcollsurg.2020.04.011 [ Links ]
20. American College of Surgeons [internet]. Personal Protective Equipment (PPE): ASA and APSF Joint Statement on Perioperative Testing for the COVID-19 Virus. 2020 [actualizada el 1 junio de 2020]. Disponible en: Disponible en: https://www.asahq.org/about-asa/newsroom/news-releases/2020/04/asa-and-apsf-joint-statement-on-perioperative-testing-for-the-covid-19-virus [ Links ]
21. American Society of Anesthesiologists Task Force on Sedation and Analgesia by Non-Anesthesiologists. Practice guidelines for sedation and analgesia by non-anesthesiologists. Anesthesiology. 2002;96(4):1004-1017. http://doi.org/10.1097/00000542-200204000-00031 [ Links ]
22. Roback MG, Green SM, Andolfatto G, Leroy PL, Mason KP. Tracking and Reporting Outcomes Of Procedural Sedation (TROOPS): Standardized Quality Improvement and Research Tools from the International Committee for the Advancement of Procedural Sedation. Br J Anaesth. 2018;120(1):164-172. http://doi.org/10.1016/j.bja.2017.08.004 [ Links ]
23. Luis S, Margarita H, Javier P, Daniela S. New protection barrier for endoscopic procedures in the era of pandemic COVID-19. VideoGIE. 2020;10.1016/j.vgie.2020.05.006. http://doi.org/10.1016/j.vgie.2020.05.006 [ Links ]
Citation: Molano-Caro J, Borrero-Cortés C, Lizarazo-Rodríguez J, Gómez-Chacón NE. Restarting care-related activities in the context of COVID-19: Prioritization, protocols, and procedures. Experience of a gastroenterology outpatient unit in Bogotá, Colombia. Rev Colomb Gastroenterol. 2020;35(3):287-297. https://doi.org/10.22516/25007440.598
Received: June 18, 2020; Accepted: August 14, 2020











 text in
text in 



