Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em
SciELO
Similares em
SciELO -
 Similares em Google
Similares em Google
Compartilhar
Revista colombiana de Gastroenterología
versão impressa ISSN 0120-9957
Rev Col Gastroenterol vol.35 no.3 Bogotá jul./set. 2020 Epub 01-Mar-2021
https://doi.org/10.22516/25007440.464
Original article
Are the ASGE criteria sufficient to stratify the risk of choledocholithiasis?
1Especialista en Cirugía General, Clínica CES. Docente adscrito, Universidad CES; Medellín, Colombia
2Residente de Cirugía General. Especialista en Epidemiología, Universidad CES; Medellín, Colombia
3Residente de Cirugía General, Universidad CES; Medellín, Colombia
4Médica general, especialista en Epidemiología, Universidad CES; Medellín, Colombia
Introduction:
Biliary lithiasis is one of the most frequent diseases in the area of general surgery and gastroenterology. Treatment varies depending on the location of the gallstones. Several stratification scales of the risk of choledocholithiasis have been defined, being the criteria proposed by the American Society of Gastrointestinal Endoscopy (ASGE) the most used worldwide, with a diagnostic accuracy of 70%. However, the procedures or diagnostic aids defined by these criteria, sometimes, increase hospital stay, costs, and may lead to the development of complications.
Methodology:
An observational, analytical, retrospective, cross-sectional study was conducted with data obtained from the clinical records of patients undergoing laparoscopic cholecystectomy at the CES Clinic in Medellín, Colombia, between July and December of 2017.
Results and conclusions:
424 medical records were analyzed, of which 254 (56.76%) were classified as low-risk, 94 (22.11%) as intermediate-risk and 76 (17.88%) as high-risk. The frequency of choledocholithiasis was 90.8% in high-risk patients and 26.6% in intermediate-risk patients. For the intermediate-risk category, statistically significant differences were found between the two groups for the total bilirubin, direct bilirubin, and AST values (p: 0.001, p: 0.014, p:0.007, respectively). The low frequency of choledocholithiasis in the intermediate-risk category can be explained by less than 5mm gallstones not identified by the cholangioresonance. Based on this study, we propose to adjust the ranges of the ASGE criteria variables for the intermediate-risk category for better accuracy when classifying patients with biliary lithiasis and, thus, reduce costs and hospital stay.
Keywords: Choledocholithiasis; Choledocholithiasis risk; ASGE criteria; Cholecystitis
Introducción:
la patología biliar litiásica es una de las entidades más frecuentes en el área de cirugía general y en gastroenterología. El tratamiento varía según el lugar donde se alojen los cálculos. Para esto, se han definido diversas escalas de estratificación del riesgo de presentar coledocolitiasis, pero son los criterios planteados por la Sociedad Americana de Endoscopia Gastrointestinal (American Society for Gastrointestinal Endoscopy, ASGE) los más usados a nivel mundial, ya que tienen una precisión diagnóstica definida del 70 %. Los procedimientos o ayudas diagnósticas establecidas por estos criterios, en ocasiones, prolongan el tiempo de hospitalización, aumentan los costos y pueden tener complicaciones.
Metodología:
se realizó un estudio observacional analítico, de tipo transversal retrospectivo, con datos obtenidos a partir de las historias clínicas de pacientes sometidos a colecistectomía laparoscópica, en la Clínica CES de Medellín, entre julio y diciembre de 2017.
Resultados y conclusiones:
se analizaron 424 historias clínicas de pacientes sometidos a colecistectomia laparoscópica. De ellos, 254 (56,76 %) se categorizaron como de riesgo bajo, mientras que 94 (22,11 %) fueron de riesgo intermedio y 76 (17,88 %) de riesgo alto. Se encontró una frecuencia de coledocolitiasis del 90,8 % en aquellos categorizados como de riesgo alto y del 26,6 % en los pacientes de riesgo intermedio. En la categoría de riesgo intermedio se hallaron diferencias estadísticamente significativas entre ambos grupos para los valores de bilirrubina total, bilirrubina directa y aspartato aminotransferasa (AST) (p = 0,001; p = 0,014; p = 0,007, respectivamente). La baja frecuencia de coledocolitiasis en la categoría de riesgo intermedio puede ser explicada por cálculos menores a 5 mm no visibles en la colangiorresonancia. A partir de este estudio, se propone ajustar los rangos de valores de los criterios de la ASGE para la categoría de riesgo intermedio, permitiendo tener una mayor precisión a la hora de clasificar los pacientes con patología litiásica y disminuir costos y estancia hospitalaria.
Palabras clave: Coledocolitiasis; riesgo de coledocolitiasis; criterios ASGE; colecistitis
Introduction
Biliary lithiasis is one of the main causes of consultation to the general surgery and gastroenterology services. This condition comprises a group of diseases affecting the gallbladder and the intra- and extra-hepatic bile ducts, and that are secondary to the pathological presence of stones. These stones have an impact on the patient’s morbidity and mortality, which are secondary to the obstruction of the ducts. Symptoms vary from episodes of abdominal pain to sepsis or even death 1,2.
This disease is one of the most frequent medical conditions, affecting around 20 million people worldwide, with reported prevalences of up to 20% 1,2. Of these patients, about 10% require cholecystectomy because of recurrent symptoms and about 20% may experience choledocholithiasis at some point during the course of the disease.
In Colombia, approximately 60 000 symptomatic cholelithiasis cases are surgically treated. However, the incidence of lithiasis in the country has not clearly defined, as i values ranging from 0.3% to 60% have been described 1,3.
When treating a patient with symptomatic cholelithiasis or cholecystitis, it is important to classify the risk of choledocholithiasis to be able to define the need for additional diagnostic procedures or aids 2, such as cholangiorensonance, endoscopic ultrasound or endoscopic retrograde cholangiopancreatography (ERCP), which are not exempt from complications 1,4,5.
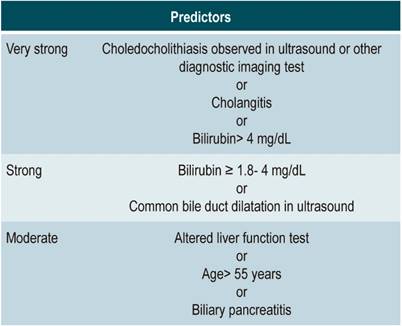
For this reason, multiple predictive scales have been created. One of the most accepted scales worldwide is the one proposed by the American Society for Gastrointestinal Endoscopy (ASGE), developed in 2010. It proposes to stratify patients according to the risk (low, intermediate, or high) of presenting choledocholithiasis. This risk is calculated based on imaging findings, liver function tests, and associated factors (Table 1).
Once the condition is categorized, one of the following procedures is performed: laparoscopic cholecystectomy, magnetic resonance cholangiography, endoscopic ultrasound, or ERCP 6,7. Currently, these criteria have a diagnostic accuracy close to 70% (8).
However, even if these criteria are applied, the diagnostic procedures or aids mentioned above pose complications to patients, as well as high costs. Therefore, establishing with greater precision the risk of choledocholithiasis in each patient first and then performing the diagnostic test or the corresponding procedure is essential to reduce morbidity and mortality, as well as costs for health systems.
The objective of this study is to describe the demographic and clinical characteristics of patients with biliary lithiasis treated at a tertiary care center, as well as the diagnostic aids used and the surgical findings that were reported. For this purpose, the frequency of choledocholithiasis in each one of the risk categories, according to ASGE criteria, was determined and the factors associated to choledocholithiasis in patients with intermediate risk were identified.
Materials and methods
This is an observational, cross-sectional, retrospective study with analytical interest. The medical records of patients who underwent laparoscopic cholecystectomy for biliary lithiasis between July and December 2017 in a private tertiary care center were reviewed. This medical center has a general surgery service, and an average of 130 laparoscopic cholecystectomies are performed every month.
After performing the laparoscopic cholecystectomy, information on the choledocholithiasis risk stratification based on the 2010 ASGE criteria was collected (Table 1). According to these parameters, patients categorized as low risk were taken directly to cholecystectomy by laparoscopy, while those at intermediate risk underwent a cholangioresonance. Depending on the result, whether it was negative or positive for choledocholithiasis, a laparoscopic cholecystectomy or an ERCP plus a laparoscopic cholecystectomy (during the same surgical procedure) was performed, respectively. Meanwhile, high-risk patients underwent and ERCP.
Patients with a malignant biliary disease, a diagnosis of recurrent choledocholithiasis, a history of bile duct interventions or biliary diversions, as well as a diagnosis of biliary dyskinesia or previous liver disease were excluded. Moreover, the medical records that did not report all the variables necessary to calculate the risk of choledocholithiasis according to ASGE criteria were excluded.
Within this context, a univariate analysis was carried out, calculating the absolute and relative frequencies for qualitative variables, as well as medians with their respective interquartile ranges for quantitative variables. To compare the groups (choledocholithiasis vs. noncholedocholithiasis) in intermediate-risk patients, the chi-square test (χ²) or the Whitney Mann U test were used. A value of p ≤0.05 was considered statistically significant. Data were analyzed using the statistical program SPSS 22®.
Results
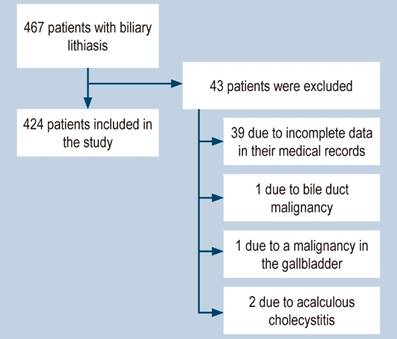
Between July and December 2017, 467 patients with biliary lithiasis underwent a laparoscopic cholecystectomy at the Clínica CES, located in Medellín, Colombia. After applying the exclusion criteria, the medical records of 424 people with this disease were analyzed (Figure 1). This way, 76 (17.8%) patients were classified as high risk, 94 (22.1%) as intermediate risk, and 254 (59.7%) as low risk. These patients were treated with ERCP, cholangioresonance, and laparoscopic cholecystectomy, respectively.
The median age of patients with choledocholithiasis was similar to the age of patients without this condition (45 vs. 41 years old; p = 0.114); in both groups, females were predominant (77 and 69%, respectively; p = 0.118). The development of acute pancreatitis and cholangitis was higher in patients with choledocholithiasis, compared to those without it (17% vs. 7.3%; p = 0.004; 13.8% vs. 0.6%; p <0.0001). The presence of acute cholecystitis was higher in the group without choledocholithiasis (77 % vs. 59.9 %; p = 0.001). All patients with Mirizzi syndrome were in the group without choledocholithiasis (Table 2).
Table 2 Characteristics of the population with biliary lithiasis
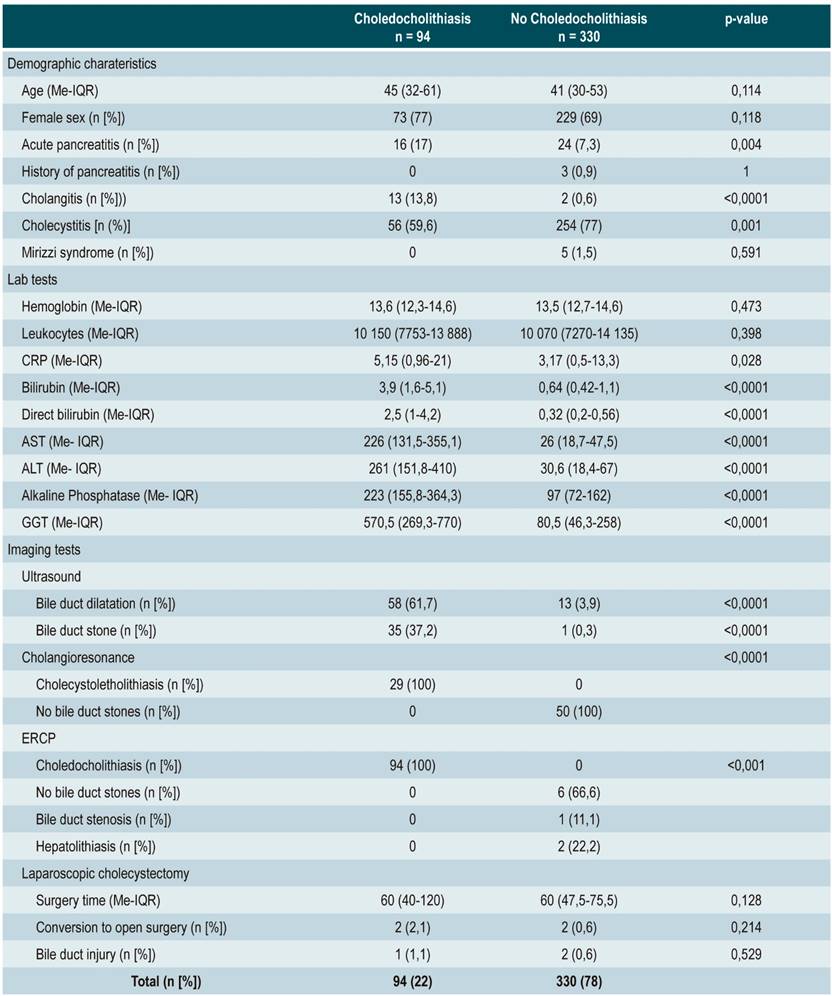
ASGE: American Society for Gastrointestinal Endoscopy; IQR: interquartile range; Me: median; n: number; CRP: C-reactive protein; AST: aspartate aminotransferase; ALT: alanine aminotransferase; GGT: γ-glutamyl transpeptidase; ERCP: endoscopic retrograde cholangiopancreatography.
When comparing the lab tests of both patient groups, no differences were found in the values for the complete blood count and the acute phase reactants. However, a higher frequency of cholestatic pattern was observed in patients with choledocholithiasis. In addition, increased bilirubin, direct bilirubin, γ-glutamyl transpeptidase (GGT), alkaline phosphatase and transaminases levels were observed in this group (Table 2).
Likewise, bile duct dilatation (>6 mm) and the presence of hypoechoic images compatible with stones in the bile duct, evidenced in the ultrasound scan, were more frequent in patients with choledocholithiasis (61.7% vs. 3.9% and 37.2% vs. 0.3%, respectively; all with p <0.0001). Also, ERCP was performed in 103 patients. Of these, 94 (91.3%) had a confirmed diagnosis of choledocholithiasis, while 9 (8.7%) had other diagnoses: in 6 evidence of stones was not found, 1 was diagnosed with bile duct stenosis, and 2, with hepatolithiasis. There were not differences between both groups regarding surgical procedure times, risk of conversion and bile duct injury (Table 2).
When categorizing the risk of choledocholithiasis, in 90.8% of patients who were classified as having a high risk this condition was confirmed through an ERCP. On the other hand, regarding patients at intermediate risk, 26.6% of them had choledocholithiasis, and 73.4% had cholelithiasis, both diagnosed through cholangioresonance.
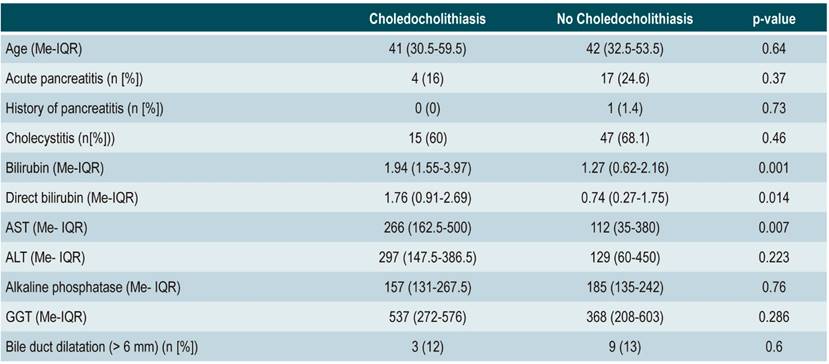
All patients in which choledocholithiasis was reported in the cholangioresonance underwent an ERCP, which confirmed the diagnosis in 100% of the cases. For this group (intermediate risk, according to the ASGE), bilirubin, direct bilirubin, and AST levels differed between those with and without choledocholithiasis (p = 0.001; p = 0.014; p = 0.007, respectively) (Table 3).
Discussion
Currently, biliary lithiasis is a clearly identified condition that forces general physicians, gastroenterologists, and general surgeons to take an appropriate diagnostic approach. When this disease has a spectrum of clinical and laboratory manifestations depending on the location of the lithiasis, and, to date, there is no optimal approach to patients at risk of choledocholithiasis.
The available literature describes several predictive models that aim to focus the optimal treatment of these patients. The ASGE scale stratifies these patients according to clinical, ultrasound imaging, and laboratory criteria, and categorizes them into three different subgroups to perform risk-based management of choledocholithiasis.
Since the publication of the 2010 ASGE guidelines, several studies have been conducted to assess their diagnostic performance in different populations. In this sense, performance rates of 75.59 % in the high risk and 49.35 % in the intermediate risk categories have been reported 9. Likewise, other retrospective studies in which the ERCP was considered as the reference test, have shown predictive values between 70 and 90% for the high-risk category, and between 34 and 50% for the intermediate risk category 10,11.
When analyzing the data obtained here, it is evident that the frequency of choledocholithiasis in the high and low risk categories is similar to that reported internationally, results that make this approach reliable. In contrast to what has been reported in the relevant literature, in patients categorized as having an intermediate risk, choledocholithiasis frequency reached 25%.
These criteria help clinicians to rule out the disease, but they are not accurate to confirm it, which causes an overuse of cholangioresonance, in which results will mostly be negative. This scenario increases costs and hospital stay times in these patients. Moreover, it should be noted that this diagnostic aid is not routinely available at all care facilities.
For that reason, this study specifically analyzed which intermediate risk variables could be associated with the presence of choledocholithiasis, finding that bilirubin levels higher than 1.94 mg/dL, direct bilirubin levels higher than 1.76 mg/dL and AST levels higher than 266 mg/dL showed a statistically significant association with the presence of this condition.
In this regard, several articles describe the usefulness of total bilirubin and alkaline phosphatase levels as predictors of choledocholithiasis 11,12.
In intermediate-risk patients, ultrasound findings did not show a significant association with the presence of choledocholithiasis. However, the measurement of the common bile duct dilatation must be interpreted based on the characteristics of each patient, such as age and body mass index 13.
In August 2019, the ASGE criteria were updated 14. Some of the main modifications were removing the history or presence of acute pancreatitis and including bile duct dilatation >6 mm as a high-risk sign, along with bilirubin >4 mg/dL. In addition, bilirubin >4 mg/dL is left alone as an intermediate risk predictor.
As a limitation of this study, it should be noted that no single gold standard method was available to determine the presence or absence of choledocholithiasis. The existing literature reports different diagnostic aids for intermediate risk patients, including cholangioresonance, endoscopic ultrasound, or intraoperative cholangiography. However, the last two are not routinely available at the medical center where the present study was conducti, which prevented us from having a diagnostic test scope.
Also, it is worth noting that not all the diagnostic tests suggested by the ASGE guidelines are available in the health care service provision context in Colombia. Endoscopic ultrasound is one of the rarest tests and is only available at quaternary care centers in Medellín. On the other hand, although it could be said that cholangioresonance is the most available method, there are still great social and economic barriers that prevent its use when necessary.
In this study, patients at high- and low-risk for choledocholithiasis achieve diagnostic accuracy in accordance with the ASGE proposal, which implies performing ERCP and laparoscopic cholecystectomy, without the need for additional studies. It is considered that, although the use of the ASGE guidelines contributes to developing an approach to patients with a risk model, it is necessary to search for alternatives that allow a better identification of those who truly require expensive and difficult to access diagnostic tests such as cholangioresonance.
Based on the results of the present study, further research to evaluate the behavior and usefulness of liver profile tests to identify the presence of choledocholithiasis is required. These tests include independent markers, mainly bilirubin, direct bilirubin, and AST, as variables for intermediate risk patients. Furthermore, specific cut-off points for each one of these tests should be looked for. These studies should be developed based on the new 2019 ASGE criteria, as these will change the number of false positives detected.
Conclusion
This study confirms that there are differences in liver function tests, acute phase reactants and imaging tests between patients with choledocholithiasis and those without it. Similarly, it was observed that the predictors of choledocholithiasis and the risk categories proposed by the 2010 ASGE guidelines allow predicting adequately the presence of choledocholithiasis in high and low risk categories.
However, according to our findings, a choledocholithiasis prevalence of 25% was observed in patients with intermediate risk reach a frequency of choledocholithiasis of 25%, which is a great help for medical personnel to rule out the disease, but not to confirm its diagnosis. The low frequency of choledocholithiasis, by means of cholangioresonance in the intermediate risk category can be explained by the existence of <5 mm stones, for which the use of endoscopic ultrasonography could be very useful. Therefore, it is necessary to consider this research as an initial step towards more accurate strategies for the prediction of choledocholithiasis.
Acknowledgments
To the Clínica CES and the Universidad CES for their support in the making of this study; to Dr. José Hugo Arias Botero for his review and methodological advice.
REFERENCES
1. Quintanilla C, Flisfisch H. Coledocolitiasis. Rev Medicina y Humanidades. 2009;1(3):160-168. [ Links ]
2. Oblitas NM. Pruebas de laboratorio como predictores de coledocolitiasis en pacientes sometidos a CPRE en un hospital nacional de referencia. Lima: Facultad de Medicina, Universidad Nacional Mayor de San Marcos; 2015. [ Links ]
3. Almora CL, Arteaga Y, Plaza T, Prieto Y, Hernández Z. Diagnóstico clínico y epidemiológico de la litiasis vesicular. Revisión bibliográfica. Rev Ciencias Médicas. 2012;16(1):200-214. [ Links ]
4. Wilkins T, Agabin E, Varghese J, Talukder A. Gallbladder Dysfunction: Cholecystitis, Choledocholithiasis, Cholangitis, and Biliary Dyskinesia. Prim Care. 2017;44(4):575-597. http://doi.org/10.1016/j.pop.2017.07.002 [ Links ]
5. Gómez M, Pion J, Otero W. Predictores de coledocolitiasis en pacientes sometidos a colangiografía retrógrada endoscópica en el Hospital El Tunal de Bogotá. Rev Col Gastroenterol. 2011;26(4):243-252. [ Links ]
6. ASGE Standards of Practice Committee, Maple JT, Ben-Menachem T, Anderson MA, Appalaneni V, Banerjee S, Cash BD, Fisher L, Harrison ME, Fanelli RD, Fukami N, Ikenberry SO, Jain R, Khan K, Krinsky ML, Strohmeyer L, Dominitz JA. The role of endoscopy in the evaluation of suspected choledocholithiasis. Gastrointest Endosc. 2010;71(1):1-9. http://doi.org/10.1016/j.gie.2009.09.041 [ Links ]
7. Abuhadba NE. Asociación entre predictores de coledocolitiasis diagnosticada por colangiografía intraoperatoria en el Hospital Nacional Arzobispo Loayza. Lima: Universidad de San Martín de Porres; 2016. [ Links ]
8. Sethi S, Wang F, Korson AS, Krishnan S, Berzin TM, Chuttani R, Pleskow DK, Sawhney MS. Prospective assessment of consensus criteria for evaluation of patients with suspected choledocholithiasis. Dig Endosc. 2016;28(1):75-82. http://doi.org/10.1111/den.12506 [ Links ]
9. Sethi S, Krishnan S, Korson AS, Chuttani R, Pleskow DK, Berzin TM, Cury M, Wang F, Sawhney M, Whadhwa V. Prospective validation of ASGE criteria for the evaluation of suspected choledocholithiasis [abstract]. J Gastroenterol Hepatol. 2013;28 Suppl 3:18. [ Links ]
10. Rubin MI, Thosani NC, Tanikella R, Wolf DS, Fallon MB, Lukens FJ. Endoscopic retrograde cholangiopancreatography for suspected choledocholithiasis: testing the current guidelines. Dig Liver Dis. 2013;45(9):744-749. http://doi.org/10.1016/j.dld.2013.02.005 [ Links ]
11. Magalhães J, Rosa B, Cotter J. Endoscopic retrograde cholangiopancreatography for suspected choledocholithiasis: From guidelines to clinical practice. World J Gastrointest Endosc. 2015;7(2):128-134. http://doi.org/10.4253/wjge.v7.i2.128 [ Links ]
12. Al-Jiffry BO, Elfateh A, Chundrigar T, Othman B, Almalki O, Rayza F, Niyaz H, Elmakhzangy H, Hatem M. Non-invasive assessment of choledocholithiasis in patients with gallstones and abnormal liver function. World J Gastroenterol. 2013;19(35):5877-82. http://doi.org/10.3748/wjg.v19.i35.5877 [ Links ]
13. Caddy GR, Tham TC. Gallstone disease: Symptoms, diagnosis and endoscopic management of common bile duct stones. Best Pract Res Clin Gastroenterol. 2006;20(6):1085-1101. http://doi.org/10.1016/j.bpg.2006.03.002 [ Links ]
14. ASGE Standards of Practice Committee, Buxbaum JL, Abbas Fehmi SM, Sultan S, Fishman DS, Qumseya BJ, Cortessis VK, Schilperoort H, Kysh L, Matsuoka L, Yachimski P, Agrawal D, Gurudu SR, Jamil LH, Jue TL, Khashab MA, Law JK, Lee JK, Naveed M, Sawhney MS, Thosani N, Yang J, Wani SB. ASGE guideline on the role of endoscopy in the evaluation and management of choledocholithiasis. Gastrointest Endosc. 2019;89(6):1075-1105.e15. http://doi.org/10.1016/j.gie.2018.10.001 [ Links ]
Citation: Toro-Calle J, Guzmán-Arango C, Ramírez-Ceballos M, Guzmán-Arango N. Are the ASGE criteria sufficient to stratify the risk of choledocholithiasis?. Rev Colomb Gastroenterol. 2020;35(3):304-310. https://doi.org/10.22516/25007440.464
Received: September 24, 2019; Accepted: February 10, 2020











 texto em
texto em