Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista colombiana de Gastroenterología
Print version ISSN 0120-9957
Rev Col Gastroenterol vol.35 no.3 Bogotá July/Sept. 2020 Epub Mar 01, 2021
https://doi.org/10.22516/25007440.446
Original article
Elevated transaminases: a new tool for the diagnosis of choledocholithiasis. A case control study
1Internista, endocrinólogo, gastroenterólogo, Universidad Nacional de Colombia; Bogotá, Colombia
2Profesor titular de Medicina, coordinador de Gastroenterología, Universidad Nacional de Colombia, Hospital Universitario Nacional de Colombia. Gastroenterólogo, Clínica Fundadores; Bogotá, Colombia
3Profesor asociado de Medicina, unidad de Gastroenterología, Universidad Nacional de Colombia, Hospital Universitario Nacional de Colombia. Gastroenterólogo, Hospital de Kennedy y UGEC; Bogotá, Colombia
Introduction:
Choledocolithiasis (CLD) affects 10% of patients with gallstones. Bile duct obstruction is associated with pancreatitis, cholangitis, and rupture of the common bile duct. This condition usually presents with increased alkaline phosphatase, GGTP and bilirubin levels. In the last decade, it has been found that up to 10% of patients with CLD have elevated aminotransferases levels. In Latin America, this alteration has not been studied. The aim of the present work was to determine the prevalence of transaminase elevation and its evolution.
Methodology:
Case-control study. ALT was measured on admission, at 48 h and at 72 h. If ultrasound was normal, MRCP and/or echo-endoscopy and ERCP were performed, as appropriate.
Results:
A total of 72 patients with choledocholithiasis (CLD) (cases) and 128 with cholecystitis without choledocholithiasis (controls) were included. Among the cases, 83% had increased ALT levels, which was 2-9 times higher in 56.9%, 10-20 times higher in 16%, and more than 20 times higher in 8.3%. At 48 hours, those levels decreased by 30% and at 72 hours by 56%. In turn, in 27.3% of the controls, ALT was 2-9 times higher in 15.6%, 10-20 times higher in 7.8% and more than 20 times higher in 2.9%. The combination of biliary colic and ALT elevation had a positive predictive value (PPV) for CLD of 72% and a negative predictive value (NPV) of 87.7%.
Conclusion:
When biliary colic and ALT elevation are reported, it is imperative to rule out choledocholithiasis. If the ultrasound is normal, MRCP and/or biliopancreatic endoscopy should be performed.
Keywords: Choledocholithiasis; Aminotransferases; Biliary colic
Introducción:
la coledocolitiasis (CDL) afecta al 10 % de los pacientes con cálculos en la vesícula biliar. La obstrucción del colédoco se asocia a pancreatitis, colangitis y ruptura del colédoco. Clásicamente, la obstrucción biliar es considerada cuando se aumentan la fosfatasa alcalina, la γ-glutamil-transpeptidasa (GGTP) y las bilirrubinas. En la última década, se ha encontrado que hasta un 10 % de los pacientes con CDL presentan elevaciones de las aminotransferasas. En Latinoamérica, no se ha estudiado esta alteración. El objetivo del presente trabajo fue determinar la prevalencia de la elevación de transaminasas y su evolución.
Metodología:
estudio de casos y controles. Se determinó la alanina aminotransferasa (ALT) al ingreso, a las 48 h y a las 72 h. Si la ecografía era normal, se realizó una colangiorresonancia o una ecoendoscopia, así como una colangiopancreatografía retrógrada endoscópica (CPRE) cuando fue necesario.
Resultados:
se incluyeron 72 pacientes con CDL (casos) y 128 con colecistitis, sin CDL (controles). En los casos, el 83 % tuvo un aumento de ALT, mientras que el 56,9 % presentó una elevación de 2-9 veces, el 16 %, de 10-20 veces, y el 8,3 % mostró una elevación >20 veces. En contraste, a las 48 h, las ALT descendieron al 30 % y a las 72 h al 56 %. Entre tanto, en los controles hubo un aumento de ALT en el 27,3 %, mientras que en el 15,6 % se observó una elevación de 2-9 veces, en el 7,8 %, de 10-20 veces, y >20 veces en el 2,9 %. La combinación de cólico biliar y la elevación de ALT tuvo un valor predictivo positivo (VPP) para CDL del 72 %, así como un valor predictivo negativo (VPN) del 87,7 %.
Conclusión:
cuando hay un cólico biliar y una elevación de ALT es imperativo descartar una CDL, y si la ecografía es normal, es necesario realizar una colangiorresonancia o una ecoendoscopia biliopancreática.
Palabras clave: Coledocolitiasis; aminotransferasas; cólico biliar
Introduction
The prevalence of cholelithiasis in the general population ranges from 5 to 10% 1. Of these patients, 10-20% develop choledocholithiasis (CDL), which is defined as the presence of stones in the common bile duct 2. This disease increases morbidity and mortality due to complications such as pancreatitis, cholangitis, and rupture of the common bile duct 3. Therefore, timely detection of common bile duct obstruction is critical for reducing such outcomes 1.
The diagnosis of CDL is often difficult and requires careful clinical, biochemical, and imaging analysis 1,4. Many experts and scientific associations have studied and proposed several criteria to determine the need to perform endoscopic retrograde cholangiopancreatography (ERCP) in patients with probable CDL 1,5,6. However, this procedure generates complications in 15% of patients 6, which is why it is indicated only for therapeutic purposes when there is already a diagnosis or a high probability of stones in the common bile duct 1,6.
When combining clinical, laboratory, and imaging findings, the probability of CDL is classified as low (<10%), intermediate (10-50%), and high (>50%) 1. Hepatobiliary ultrasound has a very low sensitivity (22-55 %) to identify stones in the common bile duct, but it is better at determining the dilation of the common bile duct (77-87 %) 1. This justifies the need for complementing said study with other two tests, resonance cholangiography and endoscopic ultrasonography, which have greater sensitivity and specificity for identifying CDL 1,6.
Recently, Suárez et al. found that, in patients with high and intermediate probability of CDL stones were observed at the time the ERCP was performed in on only 55 and 31.4%, respectively 7. This ways, sensitivity and specificity of such criteria reached 70% 7.
Most CDL patients are asymptomatic. However, when there are symptoms, people who enter the emergency department present with biliary colic and with the typical characteristics of sudden onset pain in the epigastrium or right hypochondrium, which has a variable duration, radiates to the back, is accompanied by nausea or vomiting, and is not intermittent, like colic episodes 8.
The biochemical alterations that are usually considered to predict CDL reflect cholestasis, including alkaline phosphatase, direct bilirubin and γ-glutamyl transpeptidase (GGTP) 1,6,8. However, the various guidelines and recommendations have not taken into account elevated aminotransferases as a predictor of CDL. In some case series studies, marked elevations of these enzymes have been found in patients with CDL 9-11. Despite this, in daily practice there are no protocols to determine whether elevated transaminases are a result of primary hepatocellular disease (acute hepatitis) or if the elevation is transitory due to obstruction of the common bile duct.
Thus, investigating the prevalence and relevance of aminotransferases elevation is important to establish if such elevation could predict the existence of CDL. Therefore, it is necessary to study in depth such patients through more accurate exams, given the risk of complications inherent to CDL, such as biliary pancreatitis or cholangitis, if biliary obstruction is not resolved.
Moreover, said transient hepatitis could confuse clinicians and surgeons, since symptoms could be mistaken for acute hepatitis if there is a marked elevation of aminotransferases (>10-15 times the upper normal limit), and resources would be unnecessarily spent looking for the etiology of hepatitis. This situation could expose the patient to the above-mentioned complications associated with biliary stone obstruction. Also, operating on a patient with acute hepatitis has a high morbidity.
In the literature reviewed by us, no prospective studies assessing this alteration have been conducted in Latin America. Likewise, there is not a clinical, imaging, or biochemical characterization of this group of patients that allows establishing the prevalence of aminotransferase elevation, the magnitude of the elevation, and factors associated with it.
Therefore, the present study was carried out to determine the prevalence of hypertransaminasemia and its magnitude in patients with CDL, as well as to establish if the elevation of those enzymes in an individual with biliary colic could predict CDL.
Materials and methods
Case-control study conducted between November 2015 and November 2016. Patients over 18 years of age admitted to the emergency services of the Clínica Fundadores and the Hospital El Tunal in Bogotá (Colombia) due to biliary colic were included. To determine the existence of CDL, the bile duct of all patients was studied exhaustively by means of hepatobiliary ultrasound, resonance cholangiography, echoendoscopy or ERCP.
Biliary colic was defined as a pain of sudden onset in the epigastrium or right hypochondrium, with progressive intensity until reaching the peak level, radiating to the back, and accompanied by nausea or vomiting, with a variable duration ranging from minutes to hours, and without the characteristics of a regular colic (intermittent intensity) 8.
In this context, hepatobiliary ultrasound was the first study performed. When the presence of stones in the common bile duct or its dilation (>7 mm) was not confirmed in said study, a second and more accurate study was requested in order to explore the bile duct: resonance cholangiography or biliopancreatic endosonography. The need to perform these two tests successively or individually was conditioned by the availability of such procedures. ERCP, considered the gold standard, was also used when indicated.
General objective
To determine the prevalence of aminotransferase elevation in CDL patients, as well as the performance of this alteration as a predictor of CDL.
Specific objectives
To describe the biochemical behavior of patients diagnosed with CDL and hypertransaminasemia. In addition, to determine the predisposing factors for hypertransaminasemia in patients with CDL and to describe the clinical, biochemical and background behavior in patients with a definitive diagnosis of CDL.
Sample size
Patients who were admitted to the emergency service due to biliary colic, and who were diagnosed with cholelithiasis and CDL, or CDL only, by means of cholangioresonance, echoendoscopy, ultrasonography or ERCP with a positive finding of CDL, and who met the inclusion criteria, were included. The sample was adjusted to the number of events or persons who presented with hypertransaminasemia in the necroinflammatory range required for the total of variables to be evaluated in the study. In this sense, 10 events per each variable included in the model were considered necessary. A total of 7 variables were analyzed, so it was estimated that 70 events were required to properly apply a logistic regression model.
Inclusion criteria
Patients over 18 years of age diagnosed with biliary colic who were diagnosed with biliary lithiasis, using non-invasive imaging techniques or who underwent an ERCP and a positive finding for common bile duct lithiasis was reported.
Exclusion criteria
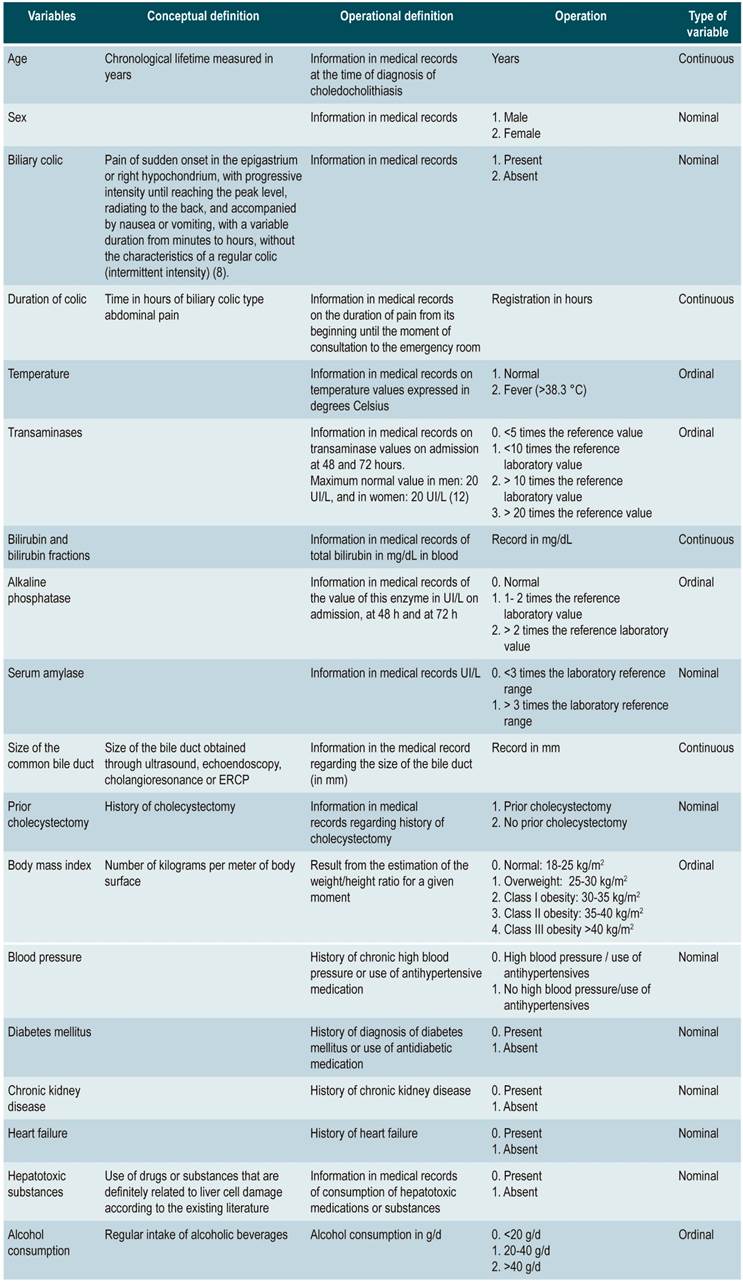
Patients with symptoms compatible with biliary colic, but without documented biliary lithiasis. Patients with shock of any etiology; patients diagnosed with hepatitis of any etiology; patients with severe comorbidities that prevented the performance of an MRI cholangiogram, ultrasound or ERCP; patients diagnosed with acute or chronic hepatitis (autoimmune, viral, toxic, metabolic), and individuals without a complete biochemical evaluation at the time of assessment. The different variables studied and the protocol for their recording are described below (Table 1).
Statistical analysis; descriptive statistics
Quantitative variables were evaluated and expressed as averages or medians. Qualitative variables were expressed as percentages or proportions.
Analytical statistics; logistic regression
A model of association with forward variable selection was made. The fundamental determinant for including variables in the model was the statistic using Wald test and the likelihood ratio. A p <0.05 was used as a reference value to consider statistical significance.
Similarly, the Hosmer-Lemeshow goodness-of-fit test was used to evaluate the model. Non-typical events were identified by calculating:
Leverage: this average was calculated among the participants, and those who had 3 times or more the value of this average were taken as influential, or not typical.
Residual: it was assumed that events follow a chi-square distribution (χ²) with a degree of freedom, so those >4 were interpreted as influential values.
Influence: those events with a value> 0.9 were considered as atypical observations. Once the atypical observations were identified, the biological plausibility of each data was evaluated and typing errors were checked.
The association of the variables with the outcome was expressed using the Odds Ratio (OR), with a 95% confidence interval (CI). Data analysis was done through the STATA 13.0 program. StataCorp. 2013. Stata Statistical Software: Release 13. College Station, TX: StataCorp LP.
Procedures and information collection
Information was collected based on the patients’ medical records and a re-interrogation process. A questionnaire was used to confirm the diagnosis of CDL (annex). All patients signed an informed consent form. The ethics committees of the participating institutions approved the research protocol and such informed consent form.
Results
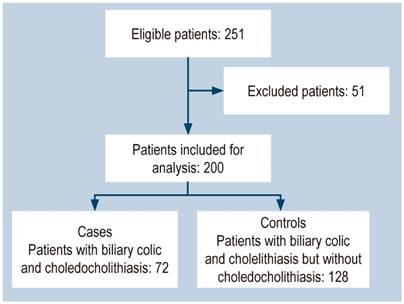
Figure 1 shows the patients’ selection process flowchart. Initially, 251 patients with a diagnosis of cholelithiasis were evaluated. 51 of them were excluded due to diagnoses of acute viral hepatitis, absence of proven biliary lithiasis and suspicion of toxic hepatitis. A total of 200 patients were included for analysis.
37.5% (75) of the patients were male. Of the total, 125 (62.5%) met the inclusion criteria. In addition, 72 (36%) had CDL and 128 (64%), cholelithiasis but no CDL. The characteristics of all patients in each group are shown in Table 2.
Table 2 Baseline characteristics of patients included in the study
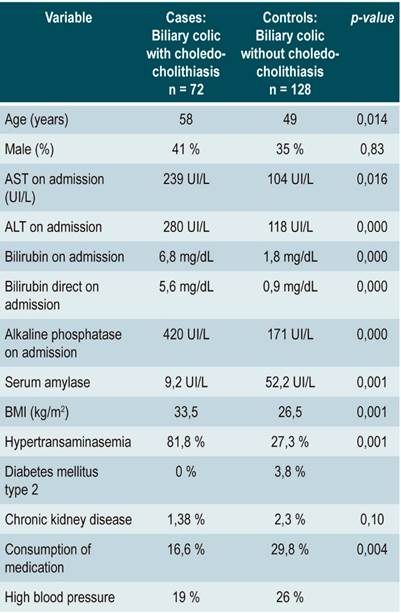
ALT: alanine aminotransferase; AST: aspartate aminotransferase; BMI: body mass index
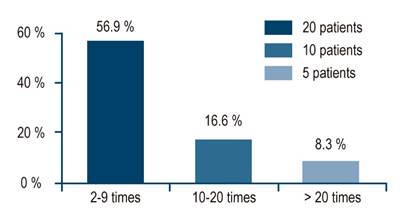
Out of the 72 CDL cases, 59 (81.9%) presented an elevation of aminotransferases >2 times. Moreover, 41 participants (56.9%) had a 2-9 times elevation; 12 (16.6%), a 10-20 times elevation, and 6 patients (8.3%) had a >20 times elevation (Figure 2).
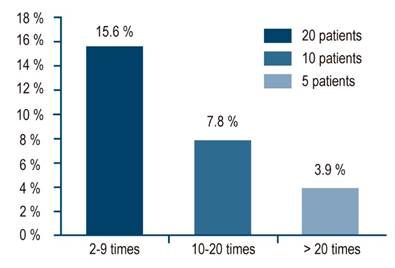
Also, 2 patients had elevations >960 IU/L and 1 showed an elevation of 1240 IU/L. Of the 128 controls, 35 (27.3%) had some degree of hypertransaminasemia >2 times above the upper normal limit. Moreover, 20 participants (15.6%) presented a 2-9 times elevation; 10 (7.8%) a 10-20 times elevation, and 5 (3.9%), a >20 times elevation (Figure 3).
Among those who had elevations >20 times, 3 patients had elevations >1000 and in 1 patient, the elevation was >2200 IU/L. ALT and AST averages were similar, but ALT averages were a little higher, which is why this enzyme was considered representative (Table 3).
Table 3 Comparative average ALT and AST values on admission
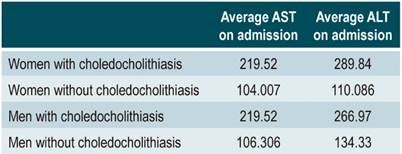
ALT: alanine aminotransferase; AST: aspartate aminotransferase
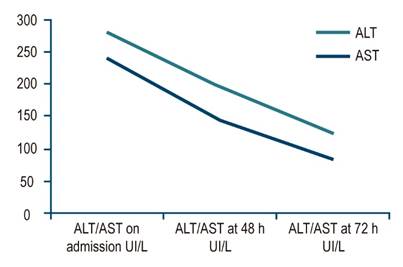
Average AST and ALT elevations, as well as their behavior, are described below. AST: 239 UI/L on admission; 146 UI/L (a 33% drop) at 48 h; 86 UI/L (a 64% drop compared to the value on admission) at 72 h. On the other hand, ALT values were: 280 UI/L on admission; 195 UI/L (a 30% drop) at 48 h; 124 UI/L (a 55% drop compared to the value on admission) at 72 h (Figure 4).
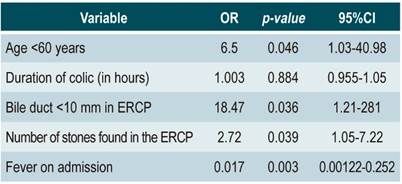
According to the multivariate analysis, the presence of hypertransaminasemia yielded an OR of 4.2 (CI, 95%: 1.98-9.02) for CDL, while the risk of elevated transaminases had an OR of 37.6 (CI, 95%: 1.25-112.6) when CDL was present. Based on the multivariate logistic regression analysis, it was established that the variables sex, duration of biliary colic in hours, obesity, body mass index, prior cholecystectomy, heart failure, chronic kidney disease, diabetes mellitus, alcohol consumption, and use of medications associated with elevated transaminases were not statistically associated with the presence of hypertransaminasemia in patients with CDL (p >0.05).
Similarly, a bile duct <10 mm, being under 60 years of age, and the number of stones found in the ERCP were positively associated with the presence of hypertransaminasemia in patients with CDL (Table 4).
Discussion
To the best of our knowledge, this is the first study that makes a prospective assessment of the prevalence and behavior of aminotransferase elevation in patients with CDL. It was found that aminotransferases increased twice or more in 83.3% of these patients. Likewise, 25% had a 10-fold or higher increase, while in patients with isolated cholelithiasis aminotransferase elevation was observed in 27.3 and 11.7%, respectively.
In this study a drop in ALT and AST values >30% at 48 h and >50% at 72 h was also observed. Following the ERCP and the extraction of the stones, this decrease was >90 %. This continuous decrease in transaminases levels is the key to identifying the transient nature of hepatitis, in the presence of blocked bile ducts and biliary colic, and differentiating it from a primary hepatocellular disease. The trend of transaminases towards a continuous decrease can help clinicians to guide the diagnosis of a patient with acute elevation of transaminases and biliary colic.
The practical implication of our results is that patients with biliary colic and transaminases levels in the range of hepatitis on admission, and who experience a transaminases values drop >30% at 48 h and >50% at 72 h, do not require additional studies for viral, toxic, or other types of hepatitis. Instead, the clinician must make an effort to determine, using precise methods such as endoscopic ultrasonography and resonance cholangiography, the presence of lithiasis in the common bile duct 7,13.
Two retrospective studies identified patients with CDL and an aminotransferase elevation >1000 IU/L. However, these studies did not establish the prevalence of such elevations in these patients, nor did they determine their behavior over time 2,14.
On the other hand, Suarez et al. 7 reported that aminotransferase elevation was found in 19 cases out of 32 CDL patients who underwent two tests to establish the levels of aminotransferases, finding an elevation on symptom onset, as well as a 30% decrease in the second test 7. However, these values were not compared to those of patients without CDL. In addition, in a similar study, Adams et al. 15 found a 30% decrease in aminotransferases levels from two measurements made on 72 patients, of which 28 (38.9%) had CDL, while the remaining 61.1% did not have this condition.
Somehow, none of these two studies describe whether patients had biliary colic or not. In general, participants were chosen based on their high probability of CDL according to the recommendations of the American Society for Gastrointestinal Endoscopy (ASGE) 1.
In our study, transaminases in all patients were measured in a planned manner on three occasions, without considering the probability of performing a pre-test, which is recommended in international guidelines. This serial measurement allowed identifying a drop of 30% at 48 hours, which further dropped by more than 50% at 72 hours.
Results obtained here, as well as those reported by the two studies mentioned above, consistently show this 30% decrease. Furthermore, in our study, patients with biliary colic and elevated aminotransferases had an OR of 4.2 (95%CI: 1.98-9.02). Likewise, when CDL is present, the probability of transaminases elevation is 37.6. The positive predictive value (PPV) of the combination of biliary colic and elevated aminotransferases (twice or higher) was 71.9%, while the negative predictive value (NPV) was 87.7%.
The reason for the elevation of transaminases in CDL patients is still unknown. Currently available studies have shown variable and inconsistent results regarding the etiology of this disease. In any case, in this study factors related to transaminases levels in the range of hepatitis such as age, size of the common bile duct, time of evolution of the biliary colic, previous cholecystectomy, sex and comorbidities (diabetes, obesity, high blood pressure and chronic kidney disease) were evaluated.
In that context, only age under 60 years, with an OR of 6.5, a size of the bile duct <10 mm, with an OR of 18.4, and the number of stones found in the ERCP (OR 2.72) showed a positive association for hypertransaminasemia in patients with lithiasis in the common bile duct. Bile duct dilatation is a compensatory phenomenon to relieve pressure within the common bile duct. Indeed, some studies have shown that people with a smaller bile duct size have the highest transaminase values 16,17. It is possible that this behavior is the result of higher pressure within the biliary tree. Findings reported here are consistent with those observations.
On the other hand, the number of gallstones found in the ERCP may be related to a higher degree of bile duct obstruction and higher pressures at this level, which would explain their association with the presence of elevated transaminases. Multiple studies have found that in younger patients, transaminases levels tend to be in in higher ranges, while several authors have shown that older patients have a physiological bile duct dilatation. This may be a compensatory factor that helps reduce pressure in the biliary tree and could also explain why younger patients show a different behavior by having a more significant elevation of transaminases when their common bile duct is blocked 17-19.
The pathophysiological mechanisms of aminotransferase elevation with acute bile duct obstruction are unknown. However, in the mid-1970s, experimental studies conducted on animal models showed that common bile duct ligation in dogs caused significant elevations of transaminases 20. In fact, according to histology findings, necrosis in hepatocytes has been found when the common bile duct was blocked 21.
In this sense, Mosberg 20 and Rosse 21 have described that acute obstruction could produce regurgitation of transaminases from the bile ducts. More recent studies suggest that the increase in chenodeoxycholic acid, caused by acute cholestasis, induces necrosis of hepatocytes 22. This process may be a consequence of decreased adenosine triphosphate (ATP), mitochondrial damage and persistent calcium influx, leading to cell death 20,22.
Although CDL can cause an atypical biochemical pattern of hepatitis without a concomitant increase in alkaline phosphatase, the additional clinical and biochemical characteristics and risk profile of these patients are unknown. Transaminase elevations are higher after performing extrahepatic bile duct ligation or intravenous morphine injection in animals undergoing cholecystectomy compared to controls 20,21. The proposed explanation for these alterations is that the gallbladder could compensate for the sudden elevations of pressure in the biliary tract 23.
The high frequency of marked aminotransferase elevations in patients with cholelithiasis and without CDL found in the present study could be related to a higher consumption of hepatotoxic drugs in these patients compared to those with CDL (29.8% vs.16.6%; p = 0.046). Alternatively, it cannot ruled out that these patients may have had a migration of small stones (<5 mm) through the bile duct, with a spontaneous resolution of the common bile duct obstruction 1.
It is possible that the exclusion of aminotransferases as predictors of CDL in the main guidelines 1,13 is due to the lack of studies on the subject. We consider that this work can contribute to the proper treatment of these difficult patients.
Limitations of the study
One of the main limitations of this study was not having the same human and technological resources available to evaluate the bile duct with resonance cholangiography and echoendoscopy. No model was made taking into account clinical variables of CDL, comorbidities, bile duct size and other laboratory parameters, such as bilirubin and alkaline phosphatase, to predict the probability of CDL together with aminotransferases. However, the purpose of this study was to specifically determine the usefulness of aminotransferase elevation as a simple marker to study such patients.
Another limitation is that this was not a multicenter study; however, this type of study in our environment may involve variables that are difficult to control given the interobserver variability and the unavailability of experts in resonance cholangiography, echoendoscopy, and ERCP.
Conclusions
Patients with biliary colic and CDL present with elevations in aminotransferases. These elevations are marked in 25% of these patients and, in many of them, simulate the characteristics of acute hepatitis. Based on our results, it is possible to state that patients with biliary colic and normal hepatobiliary ultrasound should undergo a complete liver function panel.
Similarly, if aminotransferases levels increase, including >10-fold elevations, it is necessary to make serial measurements. If a significant decrease is found (30% at 48 h and more than 50% at 72 h), a thorough study of the bile duct is required, using more accurate techniques such as cholangioresonance or biliopancreatic endoscopy, in order to rule out CDL.
The absence of aminotransferase elevation in such patients has a NPV for CDL of 87.7 %. In other words, only 12.3% of individuals with biliary colic and normal transaminases levels can have CDL. This information can easily contribute to the management of patients with this disease.
REFERENCES
1. ASGE Standards of Practice Committee, Maple JT, Ben-Menachem T, Anderson MA, Appalaneni V, Banerjee S, Cash BD, Fisher L, Harrison ME, Fanelli RD, Fukami N, Ikenberry SO, Jain R, Khan K, Krinsky ML, Strohmeyer L, Dominitz JA. The role of endoscopy in the evaluation of suspected choledocholithiasis. Gastrointest Endosc. 2010;71(1):1-9. http://doi.org/10.1016/j.gie.2009.09.041 [ Links ]
2. Tozatti J, Mello AL, Frazon O. Predictor factors for choledocholithiasis. Arq Bras Cir Dig. 2015;28(2):109-112. http://doi.org/10.1590/S0102-67202015000200006 [ Links ]
3. Copelan A, Kapoor BS. Choledocholithiasis: Diagnosis and Management. Tech Vasc Interv Radiol. 2015;18(4):244-255. http://doi.org/10.1053/j.tvir.2015.07.008 [ Links ]
4. Gómez M, Pion J, Otero W. Predictores de coledocolitiasis en pacientes sometidos a colangiografía retrógrada endoscópica en el Hospital El Tunal de Bogotá. Rev Col Gastroenterol. 2011;26(4):243-252. [ Links ]
5. Frossard JL, Morel PM. Detection and management of bile duct stones. Gastrointest Endosc. 2010;72(4):808-816. http://doi.org/10.1016/j.gie.2010.06.033 [ Links ]
6. ASGE Standards of Practice Committee, Anderson MA, Fisher L, Jain R, Evans JA, Appalaneni V, Ben-Menachem T, Cash BD, Decker GA, Early DS, Fanelli RD, Fisher DA, Fukami N, Hwang JH, Ikenberry SO, Jue TL, Khan KM, Krinsky ML, Malpas PM, Maple JT, Sharaf RN, Shergill AK, Dominitz JA. Complications of ERCP. Gastrointest Endosc. 2012;75(3):467-73. http://doi.org/10.1016/j.gie.2011.07.010 [ Links ]
7. Suárez AL, LaBarre NT, Cotton PB, Payne KM, Coté GA, Elmunzer BJ. An assessment of existing risk stratification guidelines for the evaluation of patients with suspected choledocholithiasis. Surg Endosc. 2016;30(10):4613-8. http://doi.org/10.1007/s00464-016-4799-8 [ Links ]
8. Portincasa P, Wang DQ. Gallstones. En: Podolsky DK, Camilleri M, Fitz G, Kalloo AN, Shanahan F, Wang TC. Yamada’s Textbook of Gastroenterology. Chichester: John Wiley and Sons Ltda, 6a edición; 2016. p. 1808-1834. https://doi.org/10.1002/9781118512074.ch89 [ Links ]
9. Bangaru S, Thiele D, Sreenarasimhaiah J, Agrawal D. Severe Elevation of Liver Tests in Choledocholithiasis: An Uncommon Occurrence With Important Clinical Implications. J Clin Gastroenterol. 2017;51(8):728-733. http://doi.org/10.1097/MCG.0000000000000608 [ Links ]
10. Song SH, Kwon CI, Jin SM, Park HJ, Chung CW, Kwon SW, Ko KH, Hong SP. Clinical characteristics of acute cholecystitis with elevated liver enzymes not associated with choledocholithiasis. Eur J Gastroenterol Hepatol. 2014;26(4):452-7. http://doi.org/10.1097/MEG.0000000000000053 [ Links ]
11. Agahi A, McNair A. Choledocholithiasis presenting with very high transaminase level. BMJ Case Rep. 2012;2012:bcr2012007268. http://doi.org/10.1136/bcr-2012-007268 [ Links ]
12. Kim HC, Nam CM, Jee SH, Han KH, Oh DK, Suh I. Normal serum aminotransferase concentration and risk of mortality from liver diseases: prospective cohort study. BMJ. 2004;328(7446):983. http://doi.org/10.1136/bmj.38050.593634.63 [ Links ]
13. Williams E, Beckingham I, El Sayed G, Gurusamy K, Sturgess R, Webster G, Young T. Updated guideline on the management of common bile duct stones (CBDS). Gut. 2017;66(5):765-782. http://doi.org/10.1136/gutjnl-2016-312317 [ Links ]
14. Nathwani RA, Kumar SR, Reynolds TB, Kaplowitz N. Marked elevation in serum transaminases: an atypical presentation of choledocholithiasis. Am J Gastroenterol. 2005;100(2):295-298. http://doi.org/10.1111/j.1572-0241.2005.40793.x [ Links ]
15. Adams MA, Hosmer AE, Wamsteker EJ, Anderson MA, Elta GH, Kubiliun NM, Kwon RS, Piraka CR, Scheiman JM, Waljee AK, Hussain HK, Elmunzer BJ. Predicting the likelihood of a persistent bile duct stone in patients with suspected choledocholithiasis: accuracy of existing guidelines and the impact of laboratory trends. Gastrointest Endosc. 2015;82(1):88-93. http://doi.org/10.1016/j.gie.2014.12.023 [ Links ]
16. Hu KC, Wang HY, Chang WH, Chu CH, Lin SC, Liu CJ, Wu MS, Shih SC. Clinical presentations of patients from different age cohorts with biliary tract stone diseases. J Gastroenterol Hepatol. 2014;29(8):1614-9. http://doi.org/10.1111/jgh.12581 [ Links ]
17. Huh CW, Jang SI, Lim BJ, Kim HW, Kim JK, Park JS, Kim JK, Lee SJ, Lee DK. Clinicopathological features of choledocholithiasis patients with high aminotransferase levels without cholangitis: Prospective comparative study. Medicine (Baltimore). 2016;95(42):e5176. http://doi.org/10.1097/MD.0000000000005176 [ Links ]
18. Bachar GN, Cohen M, Belenky A, Atar E, Gideon S. Effect of aging on the adult extrahepatic bile duct: a sonographic study. J Ultrasound Med. 2003;22(9):879-885. http://doi.org/10.7863/jum.2003.22.9.879 [ Links ]
19. Barthet M, Spinoza S, Affriat C, Berthezene P, Sahel J. Influence of age and biliary lithiasis on the diameter of the common bile duct. Gastroenterol Clin Biol. 1995;19(2):156-160. [ Links ]
20. Mossberg SM, Bloom A, Berkowitz J, Ross G. Serum enzyme activities following morphine. A study of transaminase and alkaline phosphatase levels in normal persons and those with gallbladder disease. Arch Intern Med. 1962;109:429-437. http://doi.org/10.1001/archinte.1962.03620160055008 [ Links ]
21. Rosser BG, Gores GJ. Liver cell necrosis: cellular mechanisms and clinical implications. Gastroenterology. 1995;108(1):252-275. http://doi.org/10.1016/0016-5085(95)90032-2 [ Links ]
22. Spivey JR, Bronk SF, Gores GJ. Glycochenodeoxycholate-induced lethal hepatocellular injury in rat hepatocytes. Role of ATP depletion and cytosolic free calcium. J Clin Invest. 1993;92(1):17-24. http://doi.org/10.1172/JCI116546 [ Links ]
23. Ginsberg AL. Very high levels of SGOT and LDH in patients with extrahepatic biliary tract obstruction. Am J Dig Dis. 1970;15(9):803-807. http://doi.org/10.1007/BF02236040 [ Links ]
Citation: Yurgaky-Sarmiento J, Otero-Regino W, Gómez-Zuleta M. Elevated transaminases: a new tool for the diagnosis of choledocholithiasis. A case control study. Un estudio de casos y controles. Rev Colomb Gastroenterol. 2020;35(3):319-328. https://doi.org/10.22516/25007440.446
Received: July 10, 2019; Accepted: August 26, 2019











 text in
text in