Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista colombiana de Gastroenterología
Print version ISSN 0120-9957
Rev Col Gastroenterol vol.35 no.3 Bogotá July/Sept. 2020 Epub Mar 01, 2021
https://doi.org/10.22516/25007440.491
Review article
Abdominal compartment syndrome
1Médica residente (MIR2), Servicio de Aparato Digestivo, Hospital Central de la Defensa Gómez Ulla; Madrid, España.
2Médico especialista, Servicio de Aparato Digestivo, Hospital Central de la Defensa Gómez Ulla; Madrid, España
3Teniente coronel médico, especialista, Servicio de Medicina Intensiva, Hospital Central de la Defensa Gómez Ulla; Madrid, España
4Teniente coronel médico, especialista. Jefe del Servicio de Aparato Digestivo. Hospital Central de la Defensa Gómez Ulla; Madrid, España
Abdominal compartment syndrome (ACS) is defined as an organ dysfunction caused by intra-abdominal hypertension (IAH). Both are common complications in severe patients admitted to intensive care units. The associated clinical manifestations are usually non-specific and, therefore, such entities should be suspected in critical patients with risk factors. The diagnosis of IAH is made by indirectly measuring intrabdominal pressure, usually by means of a urinary catheter. Treatment consists of supportive measures and, in some cases, surgical abdominal decompression. In this review the physiopathology of both entities is described, as well as the diagnostic and therapeutic approach.
Keywords: Intra-abdominal hypertension; Abdominal compartment syndrome; Acute pancreatitis
El síndrome compartimental abdominal (SCA) se define como la disfunción orgánica causada por la hipertensión intraabdominal (HIA). Ambas son complicaciones frecuentes en pacientes graves ingresados en las unidades de cuidados intensivos (UCI). Las manifestaciones clínicas asociadas suelen ser inespecíficas, por lo que dichas entidades deben ser sospechadas ante pacientes críticos con factores de riesgo. El diagnóstico de la HIA se realiza midiendo de forma indirecta la presión intraabdominal (PIA), generalmente por medio de una sonda vesical. El tratamiento consiste en medidas de soporte, y en algunos casos es necesaria la descompresión abdominal quirúrgica. En esta revisión se presenta la fisiopatología de ambas entidades, así como el enfoque diagnóstico y terapéutico.
Palabras clave: Hipertensión intraabdominal; síndrome compartimental abdominal; pancreatitis aguda
Introduction
Intra-abdominal hypertension (IAH) and abdominal compartment syndrome (ACS) are common complications in critically ill patients admitted to intensive care units (ICUs) 1. Research on both conditions in the last century has allowed achieving diagnostic improvement and developing prevention and treatment measures.
The latest consensus of the World Society for Abdominal Compartment Syndrome (WSACS) 2 allowed defining said conditions and establishing a diagnostic and therapeutic protocol based on scientific evidence. Thus, IAH is defined as a steady intra-abdominal pressure (IAP) ≥12 mm Hg and it can be classified according to its duration as:
Hyperacute: IAH that lasts for seconds as a result of, for example, laughing, coughing, or sneezing.
Acute: when IAH lasts for hours as a result of abdominal trauma or intra-abdominal bleeding.
Subacute: IAH lasts over a period of days, as in the case of severe acute pancreatitis or septic shock.
Chronic: IAH lasts for months (pregnancy) or years (morbid obesity). IAH does not cause ACS, but it can worsen it when one of the acute or subacute causes occurs 1.
On the other hand, ACS is defined as an IAP>20 mm Hg, associated with organ dysfunction or multiorgan failure that had not been previously present. It is not clear whether ACS is a phenomenon that results in multiorgan failure (MOF) or an epiphenomenon that occurs in conjunction with other organ dysfunction.
ACS is classified as primary, secondary, and recurrent. Primary ACS is caused by a disease in the abdominopelvic region (as in the case of acute pancreatitis), while secondary ACS occurs due to conditions that do not originate in the abdominal region, such as aggressive fluid resuscitation in septic shock 2. Recurrent ACS occurs after abdominal wall closure or after treatment of primary or secondary ACS. Sometimes, multiple medical conditions may overlap, leading to greater diagnostic and therapeutic difficulty 3.
Another relevant concept is abdominal perfusion pressure (APP), which is defined as the difference between mean arterial pressure (MAP) and IAP. An APP >60 mm Hg has been shown to correlate with improved survival for IAH and ACS, as well as with a lower probability of developing MOF 1-3.
Patients with an IAP <10 mm Hg usually do not develop ACS, unlike those with an IAP >25 mm Hg. People with an IAP between 10 and 25 mm Hg may or may not develop ACS, depending on individual variables such as APP and abdominal wall compliance. Similarly, patients who maintain normal APP (despite having a high IAP) have a lower risk of ACS 4.
On the other hand, abdominal wall compliance minimizes the extent to which an increase in intra-abdominal volume can increase IAP 1. Mortality due to ACS is between 40 and 100 % 2-4. Incidence rates of IAH and ACS vary according to the diagnostic criteria used and the diseases that causes the clinical signs and symptoms. Recent studies have shown a high prevalence of these conditions in medical-surgical patients admitted to the ICU. Prevalence of IAH and ACS is estimated at around 37-94% and 4-12%, respectively.
Risk factors
People who develop ACS are often critically ill patients who are unable to communicate and are mainly treated in the ICU. Its clinical manifestations are nonspecific, including malaise, weakness, lightheadedness, dyspnea, or abdominal pain. Abdominal distension is a poor predictor of ACS 3.
In this scenario, there are multiple factors for the development of ACS that can be classified depending on the occurrence of decreased abdominal wall or diaphragm compliance or increased intra-abdominal volume or the occurrence of both (Table 1).
Table 1 Risk factors for the development of ACS
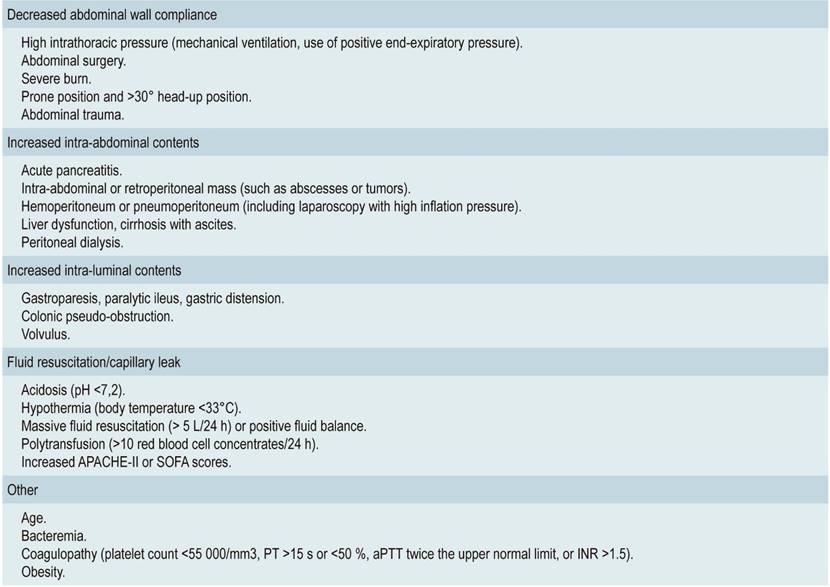
ACS: abdominal compartment syndrome; PT: prothrombin time; aPTT: activated partial thromboplastin time; INR: International Normalized Ratio; APACHE II: Acute Physiology and Chronic Health Evaluation II; SOFA: Sequential Organ Failure Assessment. Adapted from references 2 and 3.
Septic shock is highly prevalent in IAH and ACS, 82% and 38%, respectively. Therefore, it is a risk factor, as it causes distributive shock that results in peripheral vasodilatation and third spacing. All this is aggravated by massive fluid resuscitation 3-6.
In acute pancreatitis, a similar alteration occurs, with an estimated incidence of IAH and ACS of 60 and 27 %, respectively, with a higher prevalence in severe acute pancreatitis 7. Acute pancreatitis associated with IAH or ACS has been found to be associated with a significant increase in the extent of pancreatic necrosis, MOF, length of stay in hospitals, and mortality.
In a review conducted in 2014, which included 7 studies with a total of 271 patients with acute pancreatitis, it was found that mortality in patients with ACS was 49% and that it dropped to 11% in those who did not develop it 8. Increased IAP is caused by tissue inflammation, ascites, aggressive fluid therapy resuscitation beyond 48 h, paralytic ileus, or formation of pancreatic collections. Although fluid resuscitation remains a cornerstone in the treatment of acute pancreatitis, overhydration beyond 48 hours can increase mortality 8.
Obese patients are at increased risk of severe acute pancreatitis 9,10. In this sense, multiple local and systemic factors have been associated with the pathogenesis of the adverse prognosis of obesity. On a systemic level, obesity itself constitutes a pro-inflammatory state, while, on a local level, it has been shown that peripancreatic adipose tissue in obese people produce more extensive fat necrosis. Thus, this condition is a risk factor for developing ACS. However, few studies link obesity in acute pancreatitis with ACS.
Pathophysiology
Increased IAP may alter the function of different organs and systems. In the central nervous system (CNS), this elevation can lead to increased intracranial pressure and reduced brain perfusion pressure, as it affects venous return. At the cardiovascular level, central venous pressure, pulmonary capillary pressure and vascular resistance increase, while venous return and cardiac output decrease.
On the other hand, increased IAP causes increased airway pressure and intrathoracic pressure, as well as reduced total compliance of the respiratory system, especially the chest wall due to diaphragmatic compression. Therefore, dead space and intrapulmonary shunt increase, leading to the development of atelectasis. All this creates a trend toward hypercapnia and hypoxemia 1-3.
Regarding gastrointestinal effects, if IAP is >20 mm Hg, intestinal mucosa perfusion decreases, whereas if IAP is >40 mm Hg, perfusion of the upper celiac and mesenteric artery decreases. The decrease in blood flow in the intestinal mucosa results in a decrease in gastric intramucosal pH and subsequent ischemia.
In the liver, lactate clearance decreases, as well as the rest of its metabolic functions, with the possibility of an increase in liver enzymes due to hepatocellular hypoxia and centrilobular injury.
The kidney is also one of the most vulnerable organs and oliguria is one of the earliest signs. It is caused by a decrease in glomerular filtration and the activation of the renin-angiotensin-aldosterone system. Oliguria is common if IAH is >15 mm Hg, while anuria occurs if IAH is >30 mm Hg 1-3.
Diagnosis
In order to diagnose IAH, IAP must be measured indirectly using a urinary, intragastric, or intracolonic catheter, or by inserting a catheter into the inferior vena cava. The urinary catheter is recommended by the WSACS 2 since it is easy to use, minimally invasive, accurate, and economical. For proper measurement, the patient must be in supine position, with the bed at 0°.
IAP is measured at end-expiration, with no voluntary abdominal contractions, and placing the catheter at the axillary midline level on the iliac crest. In the case of IAH, it is recommended to measure IAP every 4-6 hours, or even, under certain circumstances, permanently 1,2,5.
Treatment
The initial treatment is conservative and staggered 2. There are multiple non-surgical measures available for the prevention and treatment of these entities, which are based on four fundamental pillars 2,3: a) reducing or evacuating intraluminal contents by inserting a nasogastric or rectal tube; starting prokinetic agents; reducing or suspending enteral nutrition; administering enemas; and decompressing through colonoscopy; b) assessing the drainage of space-occupying lesions in the abdomen, using a percutaneous catheter or surgery; c) improving abdominal wall compliance, ensuring adequate sedation and analgesia; considering reverse-Trendelemburg position; and, as a last resort, neuromuscular blockers; d) optimizing resuscitation with fluid therapy and avoiding aggressive fluid therapy by providing neutral or even negative fluid management. Other measures, such as using colloids or hemodialysis, remain controversial.
Prevention and early identification of risk factors is the best way to deal with ACS. When ACS diagnosis is achieved, surgical decompression is the treatment of choice. No precise threshold has been established for surgical decompression, nor has it been determined which technique would be the most appropriate. In case of organ dysfunction, some authors recommend surgical decompression when IAP is >25 mm Hg 11-14.
However, other authors recommend basing surgical decompression on APP, which has a poor prognosis when it is <50-60 mm Hg. In patients who, despite medical treatment, continue with elevated IAP associated with MOF, decompressive laparotomy should be considered. After resolving the intra-abdominal pathology, it is possible to close the abdominal cavity without exerting any tension or leaving the abdomen open.
In open abdomen, the abdominal wall can be closed using different methods 2,3: a) closing by means of clamps or staples for skin closure; b) covering the wound with a sterile translucent bag called the Bogotá bag; c) closing using a Wittmann patch or an abdominal re-approximation anchor system; d) using the ‘sandwich’ technique; e) closing with prosthetic materials or silicone coverings; f) closing techniques with negative pressure therapy.
The most used techniques currently involve the use of negative pressure. Vacuum-assisted closure (VAC) applies a negative pressure that favors abdominal muscle retraction and allows delayed fascial closure. Consequently, the abdominal fluid content is absorbed and evacuated, facilitating the control of IAP.
On the other hand, decompressive laparotomy generates an immediate improvement in the decline of IAP and improves organ dysfunction, although complications may occur, up to 50% 2. The longer the abdomen is open, the greater the morbidity. Therefore, specific strategies should be considered to prevent visceral adhesions, loss of soft tissue coverage, lateralization of the abdominal musculature and its fascia, malnutrition, and enteric fistulas 2.
Negative pressure systems are the gold standard for abdominal wound therapy 2, as they decrease the incidence of surgical complications such as wound infection, eventrations by abdominal fascia retraction, hernias, or hydroelectrolytic alterations. A complication of using these strategies is the appearance of enterocutaneous or enteroatmospheric fistulas, with an incidence of around 20 %. This complication may occur even within 8 days of initial laparotomy. Patients with intestinal anastomosis are at increased risk for this complication 2.
Regarding damage control surgery, the WACS 2 suggests that patients undergoing abdominal laparotomy due to trauma by physiologic exhaustion could be treated with prophylactic use of open abdomen vs. closure and control of IAH.
For non-traumatic acute abdomen patients, there is little evidence to support damage control techniques with prophylactic use of open abdomen. Finally, in patients with abdominal sepsis undergoing emergency laparotomy, open abdomen approach should not be routinely used, unless IAH is a specific concern.
REFERENCES
1. De Waele JJ, Cheatham ML, Malbrain ML, Kirkpatrick AW, Sugrue M, Balogh Z, Ivatury R, De Keulenaer B, Kimball EJ. Recommendations for research from the International Conference of Experts on Intra-abdominal Hypertension and Abdominal Compartment Syndrome. Acta Clin Belg. 2009;64(3):203-9. http://doi.org/10.1179/acb.2009.036 [ Links ]
2. Kirkpatrick AW, Roberts DJ, De Waele J, Jaeschke R, Malbrain ML, De Keulenaer B, Duchesne J, Bjorck M, Leppaniemi A, Ejike JC, Sugrue M, Cheatham M, Ivatury R, Ball CG, Reintam Blaser A, Regli A, Balogh ZJ, D’Amours S, Debergh D, Kaplan M, Kimball E, Olvera C; Pediatric Guidelines Sub-Committee for the World Society of the Abdominal Compartment Syndrome. Intra-abdominal hypertension and the abdominal compartment syndrome: updated consensus definitions and clinical practice guidelines from the World Society of the Abdominal Compartment Syndrome. Intensive Care Med. 2013;39(7):1190-206. http://doi.org/10.1007/s00134-013-2906-z [ Links ]
3. Sánchez-Miralles A, Castellanos G, Badenes R, Conejero R. Síndrome compartimental abdominal y síndrome de distrés intestinal agudo. Med Intensiva. 2013;37(2):99-109. http://doi.org/10.1016/j.medin.2011.11.019 [ Links ]
4. Malbrain ML, Chiumello D, Pelosi P, Bihari D, Innes R, Ranieri VM, Del Turco M, Wilmer A, Brienza N, Malcangi V, Cohen J, Japiassu A, De Keulenaer BL, Daelemans R, Jacquet L, Laterre PF, Frank G, de Souza P, Cesana B, Gattinoni L. Incidence and prognosis of intraabdominal hypertension in a mixed population of critically ill patients: a multiple-center epidemiological study. Crit Care Med. 2005;33(2):315-22. http://doi.org/10.1097/01.ccm.0000153408.09806.1b [ Links ]
5. Malbrain ML. Different techniques to measure intra-abdominal pressure (IAP): time for a critical re-appraisal. Intensive Care Med. 2004;30(3):357-371. http://doi.org/10.1007/s00134-003-2107-2 [ Links ]
6. Wilson A, Longhi J, Goldman C, McNatt S. Intra-abdominal pressure and the morbidly obese patients: the effect of body mass index. J Trauma. 2010;69(1):78-83. http://doi.org/10.1097/TA.0b013e3181e05a79 [ Links ]
7. Trikudanathan G, Vege SS. Current concepts of the role of abdominal compartment syndrome in acute pancreatitis - an opportunity or merely an epiphenomenon. Pancreatology. 2014;14(4):238-243. http://doi.org/10.1016/j.pan.2014.06.002 [ Links ]
8. van Brunschot S, Schut AJ, Bouwense SA, Besselink MG, Bakker OJ, van Goor H, Hofker S, Gooszen HG, Boermeester MA, van Santvoort HC; Dutch Pancreatitis Study Group. Abdominal compartment syndrome in acute pancreatitis: a systematic review. Pancreas. 2014;43(5):665-74. http://doi.org/10.1097/MPA.0000000000000108 [ Links ]
9. Cruz-Monserrate Z, Conwell DL, Krishna SG. The Impact of Obesity on Gallstone Disease, Acute Pancreatitis, and Pancreatic Cancer. Gastroenterol Clin North Am. 2016;45(4):625-637. http://doi.org/10.1016/j.gtc.2016.07.010 [ Links ]
10. Davis PJ, Eltawil KM, Abu-Wasel B, Walsh MJ, Topp T, Molinari M. Effect of obesity and decompressive laparotomy on mortality in acute pancreatitis requiring intensive care unit admission. World J Surg. 2013;37(2):318-332. http://doi.org/10.1007/s00268-012-1821-8 [ Links ]
11. Malbrain ML, Cheatham ML, Kirkpatrick A, Sugrue M, Parr M, De Waele J, Balogh Z, Leppäniemi A, Olvera C, Ivatury R, D’Amours S, Wendon J, Hillman K, Johansson K, Kolkman K, Wilmer A. Results from the International Conference of Experts on Intra-abdominal Hypertension and Abdominal Compartment Syndrome. I. Definitions. Intensive Care Med. 2006;32(11):1722-32. http://doi.org/10.1007/s00134-006-0349-5 [ Links ]
12. Cheatham ML, Malbrain ML, Kirkpatrick A, Sugrue M, Parr M, De Waele J, Balogh Z, Leppäniemi A, Olvera C, Ivatury R, D’Amours S, Wendon J, Hillman K, Wilmer A. Results from the International Conference of Experts on Intra-abdominal Hypertension and Abdominal Compartment Syndrome. II. Recommendations. Intensive Care Med. 2007;33(6):951-62. http://doi.org/10.1007/s00134-007-0592-4 [ Links ]
13. De Waele JJ, De Laet I, Kirkpatrick AW, Hoste E. Intra-abdominal Hypertension and Abdominal Compartment Syndrome. Am J Kidney Dis. 2011;57(1):159-169. http://doi.org/10.1053/j.ajkd.2010.08.034 [ Links ]
14. Mentula P, Hienonen P, Kemppainen E, Puolakkainen P, Leppäniemi A. Surgical decompression for abdominal compartment syndrome in severe acute pancreatitis. Arch Surg. 2010;145(8):764-769. http://doi.org/10.1001/archsurg.2010.132 [ Links ]
Citation: Sáez-Sáez AI, De La Fuente-Fernández E, Sáenz-Casco LV, Ramos-Meca MA. Abdominal compartment syndrome. Rev Colomb Gastroenterol. 2020;35(3):345-350. https://doi.org/10.22516/25007440.491
Received: December 15, 2019; Accepted: May 29, 2020











 text in
text in 



