Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista colombiana de Gastroenterología
Print version ISSN 0120-9957
Rev Col Gastroenterol vol.35 no.3 Bogotá July/Sept. 2020 Epub Mar 01, 2021
https://doi.org/10.22516/25007440.383
Case report
Modified sugiura procedure: an alternative for non-cirrhotic patients with extrahepatic portal vein thrombosis and recurrent variceal bleeding
1Cirujano hepatobiliar y de trasplantes, Centro Médico Imbanaco; Cali, Colombia
2Cirujano hepatobiliar, Centro Médico Imbanaco; Cali, Colombia
3Médica epidemióloga, Instituto de Investigaciones, Centro Médico Imbanaco; Cali, Colombia
One of the most serious consequences of extrahepatic portal vein thrombosis is portal hypertension with recurrent variceal bleeding. Once endoscopic variceal ligation fails and the spleno-portal axis is not permeable, modified Sugiura devascularization may be the only alternative. Its use in patients with cirrhosis has been reported, but there is little information on non-cirrhotic patients. This article presents a series of four cases of non-cirrhotic patients that underwent this procedure. Patients were followed for twelve months; none presented episodes of esophageal varices re-bleeding nor required ligation of residual varices. This surgery is outlined as a therapeutic alternative for this type of patients.
Keywords: Thrombosis, portal vein, extrahepatic; Portal hypertension; Modified Sugiura; Esophageal varices; Cirrhosis
Una de las consecuencias más graves de la trombosis de la vena porta extrahepática es la hipertensión portal con sangrado variceal recurrente. Una vez falla la ligadura endoscópica de las várices y el eje esplenoportal no se encuentra permeable, la devascularización tipo Sugiura modificado puede ser la única alternativa. Se ha documentado su uso en pacientes con cirrosis, pero hay poca información en personas no cirróticas. En este artículo se describe una serie de 4 casos de pacientes no cirróticos, en los cuales se realizó dicho procedimiento. Los pacientes fueron seguidos durante 12 meses y ninguno presentó episodios de resangrado de las várices esofágicas, ni tampoco se requirió la ligadura de las várices residuales. Esta cirugía se perfila como una alternativa terapéutica para este tipo de pacientes.
Palabras clave: Trombosis; vena porta extrahepática; hipertensión portal; Sugiura modificado; várices esofágicas; cirrosis
Introduction
Azygos and portal vein devascularization were first described in the literature in 1973 by Dr. Sugiura 1. This procedure involves removing the penetrating veins of the distal esophagus and the gastric fundus by making a transection in the left gastric vein, the gastroepiploic artery, and the short gastric arteries located at the beginning of the greater curvature. This procedure initially included esophageal transection and subsequent end-to-end anastomosis, as well as pyloroplasty, splenectomy, and selective vagotomy.
Early reports described the effectiveness of this procedure, which had an incidence of rebleeding of <1.5 % and a 10-year survival of >70 % and >50 % in scheduled and urgent patients, respectively 2. However, failure of esophageal anastomosis was associated with many complications and a significant mortality rate. For this reason, the technique was modified, and transection of the esophagus was excluded at first, followed by vagotomy and pyloroplasty 3. Figure 1 shows the differences between the original and the modified technique.
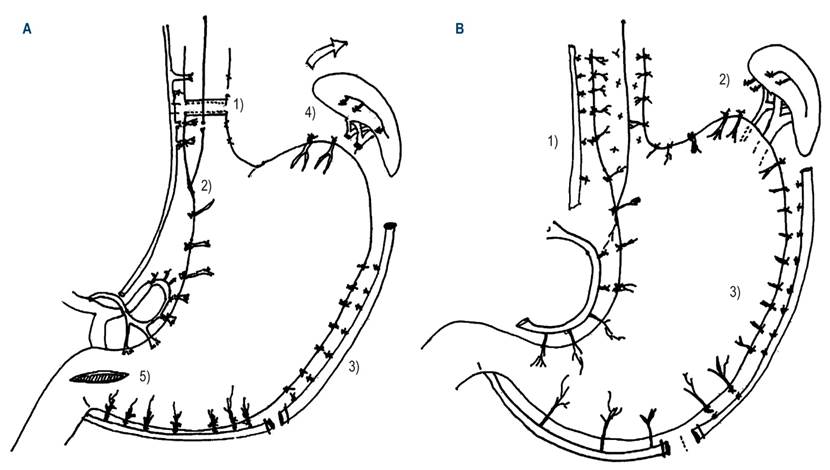
Figure 1 Original Sugiura Technique vs. Modified Technique. A. Original Sugiura Technique: 1) esophageal transection and vagus nerve ligation; 2) devascularization of the lesser curvature and distal esophagus; 3) devascularization of the greater curvature; 4) splenectomy; 5) pyloroplasty. B. Modified Sugiura Technique: 1) devascularization of the lesser curvature and distal esophagus; 2) ligation of the short arteries; 3) devascularization of the greater curvature.
Once the procedure is performed, follow-up is made through endoscopies and the ligation of residual or new varicose veins. Some studies have shown 5-year rebleeding control in over 80% of cases, which makes it a good therapeutic alternative for patients in whom beta blocker and ligation management are not sufficient to control recurrent bleeding episodes 4.
According to the World Health Organization (WHO), extrahepatic portal vein thrombosis has a prevalence of nearly 5 cases per 10 000 inhabitants 5. In 60 % of those cases, an underlying hematological disease is identified, while the remaining 40 % have different etiologies 6. Risk factors identified include gastrointestinal infections, umbilical vein catheterization, myeloproliferative disorders, use of contraceptives, pregnancy, and certain abdominal surgeries.
Nevertheless, there is not much research on the management of variceal bleeding in the context of this condition, and current recommendations are based on data from patients with portal hypertension and cirrhosis 7. This is a case series study in non-cirrhotic patients with extrahepatic portal vein thrombosis and recurrent variceal bleeding, who underwent modified Sugiura devascularization.
Description of the cases
Between 2014 and 2017, our service received 6 non-cirrhotic patients with extrahepatic portal vein thrombosis and recurrent bleeding of the esophageal varices, despite repeated ligations and management with beta- and terlipressin blockers. Of these patients, 2 could undergo classic shunting, so a splenorenal shunt was performed; the remaining 4 had episodes of recurrent variceal bleeding that required multiple transfusions and hospitalizations.
At the time of assessment, 3 patients were in the intensive care unit (ICU), extubated and receiving terlipressin, while 1 remained in the general ward. Moreover, in the last month, 3 of them had received multiple transfusions and had undergone at least 2 attempts to control bleeding through endoscopy. The other patient had suffered the most recent episode, 5 weeks earlier.
The assessment protocol included a dual-source abdominopelvic tomography with contrast agent, which was performed in all patients, together with combined splenography, and femoral venography in 2 patients. Initially, the possibility of a conventional splenorenal, mesocaval or meso-Rex shunt was considered. The lack of dilatation of the splenic vein or thrombosis of the splenic vein, or the distance between the renal vein and the splenic vein prevented the performance of a splenorenal shunt in all cases.
Likewise, the absence of superior mesenteric vein permeability, with grade IV thrombosis according to Yerdel›s classification 8, prevented the use of this structure as the site of entry for a portal cava or intrahepatic left portal shunt.
3 of the patients were operated on in the context of emergency bleeding, and the fourth underwent scheduled surgery since no active bleeding had been observed for several weeks. The hematology department ruled out the existence of thrombophilic diseases in all patients.
The modified Sugiura procedure, reported in the literature, was performed with a single-staged approach to the abdomen by making an incision in the supraumbilical midline, ligating the penetrating arteries of the proximal thirds of the stomach, and dissecting and ligating all the veins that penetrate the distal esophagus. The transhiatal technique was also used —at least 7 cm into the thorax— and a dissection was performed down to the distal muscle layers to achieve the ligation of the varicose veins and the transection of the left coronary vein and the left gastroepiploic vessels, at the junction between the antrum and the greater curvature.
Short arteries were also sectioned, and energy devices were used in vessels <5 mm, as well as ligatures with 2-0 and 3-0 silk suture. Splenectomy, ligation of the splenic artery, esophagus section, pyloroplasty, and selective vagotomy were not performed.
The average surgical time was 2.5 hours and none of the patients received vasoactive agents during the procedure. Furthermore, the average bleeding during the interventions was 200 cm3, without the need for transfusions due to intraoperative bleeding. The 4 patients were extubated during surgery and transferred to the ICU, with stable hemodynamics. During the postoperative period, the oral route was gradually started, and feeding tubes were not needed. The main characteristics of these patients are described below (Table 1).
Table 1 Patient characteristics
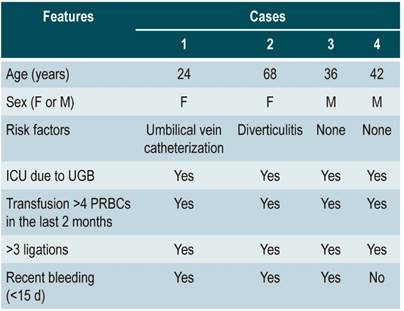
F: female; M: male; ICU: intensive care unit; UGB: upper gastrointestinal bleeding; PRBC: packed red blood cell
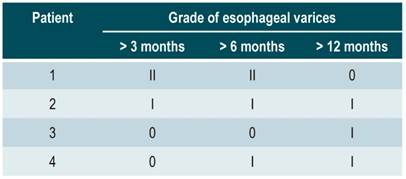
During the postoperative period, 1 patient developed transient ascites, which was resolved with diuretics, while another had delayed gastric emptying, which was corrected without treatment. There were no reinterventions or residual collections. All patients met oral caloric requirements and were discharged with follow-up order and serial endoscopies at 8 days and at 1, 3, 6 and 12 months. Endoscopic findings are summarized below (Table 2).
In this context, in the 3-month follow-up, only 2 patients had residual grade I and II varices (<5 mm), while in the first patient they disappeared by insufflation. The other 2 individuals did not have varices in the esophagus or gastric fundus, although portal hypertensive gastropathy was observed.
Prophylactic ligatures were not necessary, and the beta-blocker was removed in all patients, except for the person with grade II varices, who had a bleeding from colonic varices a month after the surgery was performed. This patient was treated conservatively by increasing the beta blocker dose. No rebleeding was reported at the 8-month follow-up.
Follow-up at 1 year revealed 3 patients with varices <5 mm, which disappeared with insufflation, while the fourth patient had no varicose manifestations. Finally, bleeding from esophageal varices was not observed in any of the patients.
Discussion
Multiple reports describe the results of this surgical procedure in terms of variceal rebleeding control. However, most of these reports are from patients with cirrhosis and thrombosis of the entire splenoportal axis. These patients were taken to devascularization, as liver transplantation was not technically feasible and multivisceral transplantation was not available 3.
Complications of portal hypertension due to thrombosis of the extrahepatic portal vein, not associated with cirrhosis, have been poorly described. In case of medical and endoscopic failure, surgical or percutaneous shunts are the treatment of choice. However, these options are limited since thrombosis of the splenic and upper mesenteric veins has been observed in up to 50% of cases. In this scenario, the modified Sugiura procedure becomes a suitable option for this type of patients 7,9-11.
Studies conducted in Japan have reported rebleeding control in over 70 % of cases at 10 years and in over 80 % at 5 years 12. On the contrary, some studies, such as the one by Mercado et al., do not report good long-term results 13.
The 4 patients assessed in the present study developed severe symptoms due to variceal bleeding recurrence and underwent multiple hospitalizations and transfusions. At the time of writing this paper, none of them had required variceal ligation and the only rebleeding case was associated with colonic varices. Also, no patient had shown any signs of liver dysfunction and all of them were able to resume their working activity. Therefore, regular follow-up with endoscopy allows early detection of residual varices and establishing the need for ligation.
In our experience, the modified Sugiura procedure may be a safe option to control the risk of rebleeding in patients with recurrent variceal hemorrhage and thrombosis of the extrahepatic spleno-mesenteric portal axis —of non-cirrhotic origin—, who, in addition, are not candidates for other conventional therapies such as portosystemic shunts. Studies with larger samples and long-term follow-up are needed to strengthen knowledge in this area.
REFERENCES
1. Sugiura M, Futagawa S. A new technique for treating esophageal varices. J Thorac Cardiovasc Surg. 1973;66(5):677-685. https://doi.org/10.1016/S0022-5223(19)40560-6 [ Links ]
2. Sugiura M, Futagawa S. Esophageal transection with paraesophagogastric devascularizations (the Sugiura procedure) in the treatment of esophageal varices. World J Surg. 1984;8(5):673-679. http://doi.org/10.1007/BF01655762 [ Links ]
3. Voros D, Polydorou A, Polymeneas G, Vassiliou I, Melemeni A, Chondrogiannis K, Arapoglou V, Fragulidis GP. Long-term results with the modified Sugiura procedure for the management of variceal bleeding: standing the test of time in the treatment of bleeding esophageal varices. World J Surg. 2012;36(3):659-66. http://doi.org/10.1007/s00268-011-1418-7 [ Links ]
4. Schettini AV, Pinheiro RS, Pescatore P, Lerut J. Modified Sugiura Operation for Idiopathic Portal Hypertension with Bleeding Oesophageal Varices. A Case Report. Acta Chir Belg. 2015;115(3):237-240. http://doi.org/10.1080/00015458.2015.11681105 [ Links ]
5. Garcia-Pagán JC, Hernández-Guerra M, Bosch J. Extrahepatic portal vein thrombosis. Semin Liver Dis. 2008;28(3):282-292. http://doi.org/10.1055/s-0028-1085096 [ Links ]
6. Valla DC, Condat B. Portal vein thrombosis in adults: pathophysiology, pathogenesis and management. J Hepatol. 2000;32(5):865-871. http://doi.org/10.1016/s0168-8278(00)80259-7 [ Links ]
7. Llop E, Seijo S. Treatment of non-cirrhotic, non-tumoural portal vein thrombosis. Gastroenterol Hepatol. 2016;39(6):403-410. http://doi.org/10.1016/j.gastrohep.2015.09.007 [ Links ]
8. Yerdel MA, Gunson B, Mirza D, Karayalçin K, Olliff S, Buckels J, Mayer D, McMaster P, Pirenne J. Portal vein thrombosis in adults undergoing liver transplantation: risk factors, screening, management, and outcome. Transplantation. 2000;69(9):1873-81. http://doi.org/10.1097/00007890-200005150-00023 [ Links ]
9. Grace ND. Prevention of initial variceal hemorrhage. Gastroenterol Clin North Am. 1992;21(1):149-161. [ Links ]
10. de Franchis R, Primignani M. Endoscopic treatments for portal hypertension. Semin Liver Dis. 1999;19(4):439-455. http://doi.org/10.1055/s-2007-1007131 [ Links ]
11. Soonawalla ZF, Shah SR, Mathur SK. Modified sugiura procedure. J Am Coll Surg. 2002;194(2):247. https://doi.org/10.1016/S1072-7515(01)01146-2 [ Links ]
12. Dagenais M, Langer B, Taylor BR, Greig PD. Experience with radical esophagogastric devascularization procedures (Sugiura) for variceal bleeding outside Japan. World J Surg. 1994;18(2):222-8. http://doi.org/10.1007/BF00294405 [ Links ]
13. Mercado MA, Orozco H, Vasquez M, Pantoja JP, Contreras A, Catzin-Kuhlmann A, Flores A, Rodriguez-Davalos M. Comparative study of 2 variants of a modified esophageal transection in the Sugiura-Futagawa operation. Arch Surg. 1998;133(10):1046-9. http://doi.org/10.1001/archsurg.133.10.1046 [ Links ]
Citation: Rico JM, Castro-Villegas F, Ocampo CE. Modified sugiura procedure: an alternative for non-cirrhotic patients with extrahepatic portal vein thrombosis and recurrent variceal bleeding. Rev Colomb Gastroenterol. 2020;35(3):377-381. https://doi.org/10.22516/25007440.383
Received: March 27, 2019; Accepted: July 31, 2019











 text in
text in