Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista colombiana de Gastroenterología
Print version ISSN 0120-9957
Rev Col Gastroenterol vol.35 no.3 Bogotá July/Sept. 2020 Epub Mar 01, 2021
https://doi.org/10.22516/25007440.385
Case report
Treatment of choledocholithiasis by ERCP, and instrumentation through a T-tube
1Gastroenterólogo, Hospital Central de la Policía; Bogotá, Colombia
2Cirujano general, Hospital Central de la Policía; Bogotá, Colombia
3Cirujano general, Hospital Central de la Policía; Bogotá, Colombia
4Jefe del Servicio de Gastroenterología, Hospital Central de la Policía; Bogotá, Colombia
The treatment of choledocholithiasis has evolved significantly since Robert Abbé performed the first bile duct exploration via choledochotomy in New York in 1889. Endoscopic retrograde cholangiopancreatography (ERCP), which was initially used for diagnosis, is now only valid as a therapeutic tool. Currently, the main diagnostic methods are magnetic resonance cholangiopancreatography (MRCP) and endoscopic ultrasound (EUS). The treatment of choledocholithiasis moved from the open surgery in which biliary stenting was routinely performed on a Kehr tube or T-tube, to the endoscopic technique using ERCP, sphincteroplasty and instrumentation with balloons and baskets. Additional techniques are now available such as mechanical or extra-corporeal lithotripsy, endoscopic papillary large balloon dilation and SpyGlass cholangioscopy. The laparoscopic technique has been used for several years in different parts of the world for the treatment of choledocholithiasis. Recent studies even propose performing the primary closure of the bile duct or choledochoduodenostomy, so that the T-tube is not necessary. However, in many other places, and for a variety of reasons, open exploratory surgery and the T-tube continue to be used, being an important option in the treatment of some patients. Case presentation: 88-year-old male patient with recurrent choledocholithiasis and a giant gallstone that was difficult to treat endoscopically, with sepsis of biliary origin, which required open surgical drainage at the emergency room. Choledocotomy was performed, and a T-tube was inserted at the site. Subsequently, a successful joint treatment was performed by the General Surgery Service and the Gastroenterology Service, using T-tube instrumentation and ERCP, respectively.
Keywords: Choledocholithiasis; Endoscopic Retrograde Cholangiopancreatography (ERCP); Bile duct exploration; Kehr tube; Laparoscopic T-tube
El tratamiento de la coledocolitiasis ha evolucionado de forma significativa desde que Robert Abbe realizó la primera coledocotomía y la exploración de las vías biliares en Nueva York, en 1889. La colangiopancreatografía retrógrada endoscópica (CPRE), que inicialmente fue un método diagnóstico, ahora solo tiene validez como método terapéutico. En la actualidad, los principales métodos diagnósticos son la colangioresonancia magnética (CRM) y la ultrasonografía endoscópica (USE). El tratamiento de la coledocolitiasis pasó de la técnica quirúrgica abierta -en la que, de forma rutinaria, se realizaba la coledocorrafia sobre un tubo de Kehr o tubo en T- a la endoscópica, mediante el uso de la CPRE, la esfinteroplastia y la instrumentación con balones y canastilla. Hoy en día se dispone de técnicas adicionales como la litotricia mecánica (LM) o extracorpórea, la dilatación con balón (DB) de gran tamaño y el Spyglass ® . La técnica laparoscópica se usa desde hace varios años, en diversas partes del mundo, para el tratamiento de la coledocolitiasis. Estudios recientes proponen incluso el cierre primario del colédoco o la coledocoduodenostomía, con lo cual no sería necesaria la utilización del tubo en T. Pero en muchos otros sitios, y por diversas razones, se continúa usando la exploración quirúrgica abierta y el tubo en T, que representa una importante opción en el tratamiento de algunos pacientes. Caso clínico: paciente masculino de 88 años, con coledocolitiasis recidivante, cálculo gigante de difícil manejo endoscópico y sepsis de origen biliar, que requirió drenaje quirúrgico abierto de urgencias. Se realizó una coledocotomía, y se dejó el tubo en T. Posteriormente, se efectuó un tratamiento exitoso conjunto, mediante instrumentación por el tubo en T, por parte de cirugía general, y CPRE, por gastroenterología.
Palabras clave: Coledocolitiasis; colangiopancreatografía retrógrada endoscópica (CPRE); instrumentación de la vía biliar; tubo de Kehr; tubo en T; laparoscopia
Introduction
Patients with vesicular and choledochal lithiasis may be treated in two stages: first, when performing an endoscopic retrograde cholangiopancreatography (ERCP) and then, when an open or laparoscopic cholecystectomy is performed. They may also be treated in a single surgical time through laparoscopic cholecystectomy (LAPCHOL) and laparoscopic common bile duct exploration (LCBDE).
Several meta-analyses conclude that both single-stage and two-stage treatments are equally effective in terms of success rate and have similar morbidity and mortality rates 1,2. The use of the single-stage or two-stage technique depends on the resources available and the experience of each medical group.
Cholecystectomy, as well as open common bile duct exploration, continue to be performed in various hospitals in our country, given the lack of resources and training. Furthermore, in leading medical centers, these procedures are limited to patients in which, for multiple reasons, endoscopic treatment for choledocholithiasis is not possible.
In patients with choledocholithiasis, ERCP is now considered the first line of treatment. On the other hand, surgical exploration is reserved for patients in whom choledocholithiasis has not been resolved because of the characteristics of the stones (size or location) or due to anatomical variations related or not to surgical history, which prevent proper cannulation of the bile duct 3.
Kehr’s tube (or T-tube) was effective and widely used for many years, especially during the second half of the past century. Its use was indicated in patients in which a choledocotomy had to be performed for the successful or unsuccessful exploration of the bile ducts, or as a splinting tool in bile duct reconstructions. However, since ERCP became available, its use has decreased over the last two decades 4,5.
Currently, some authors propose the primary closure of the bile duct and choledochorraphy over the use of stents and even choledocoduodenostomy, which leads to believe that the use of the T-tube tends to disappear 6.
However, we consider that the T-tube is still useful in our country and, on a global scale, in some selected scenarios. Consequently, we present the case of a patient with choledocholithiasis of difficult management, in whom the T-tube was used along with duodenoscopy and ERCP for instrumentation of the bile duct, achieving a successful result.
Case presentation
On December 31, 2018, an 88-year-old male was admitted to the emergency department of the Hospital Central de la Policía (HOCEN). The patient experienced colic-like abdominal pain in the upper right quadrant for three days, associated with choluria and general discomfort, without acholia or other related symptoms. The patient had a history of high blood pressure treated with losartan, chronic obstructive pulmonary disease (COPD), and cholecystectomy, which was performed 17 years before his admission.
At the time of physical examination on admission, he was found to be in a generally acceptable condition for his age: blood pressure (BP): 128/78 mm Hg, heart rate (HR): 60 bpm, and respiratory rate (RR): 18 brpm. Moreover, the individual was alert, afebrile, well-hydrated, and without mucocutaneous jaundice. He also had a decrease in respiratory sounds in the bibasilar crackles, without signs of peritoneal irritation, and slight pain on palpation of the upper right quadrant.
In his laboratory tests on admission the following findings were reported: leukocytes: 13,550; hematocrit: 34%; hemoglobin: 11 g/dL; platelet count: 532,000/mL; alkaline phosphatase: 977 IU/L; total bilirubin: 2.22 mg/dL; direct bilirubin: 1.64 mg/dL, and indirect bilirubin: 0.58 mg/dL. In addition, glutamic-pyruvic transaminase was 252 IU/L, while glutamic-oxalacetic transaminase was 220 IU/L. A complete ultrasound of the abdomen was performed, finding postcholecystectomy syndrome and fatty liver.
The patient was assessed by the Gastroenterology Service for suspected choledocholithiasis. Therefore, a magnetic resonance cholangiopancreatography (MRCP) was requested. The results (obtained on January 2, 2019) reported the presence of two faceted stones of 16 and 18 mm, with dilation of the distal bile duct of up to 17 mm and slight dilation of the intrahepatic bile duct (Figure 1).
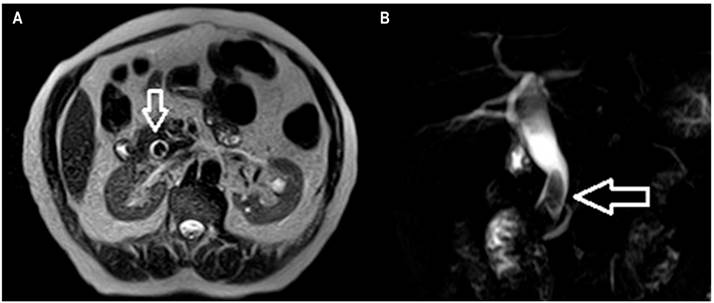
Figure 1 MRCP. A. Coronal plane showing a large stone that completely occupies the lumen of the bile duct. B. Three-dimensional reconstruction in which the two faceted stones and the dilation of the bile duct are observed.
On January 3, the patient was taken for an ERCP (in addition to a papillotomy), performed by two gastroenterologists specialized in the bile duct. The cholangiography revealed two stones of approximately 20 mm, which could not be removed; it was not possible to insert a stent either. During the procedure, the patient presented hemodynamic instability, so he was transferred to the intensive care unit (ICU), where life support was required. He was diagnosed with sepsis of biliary origin, so the general surgery service assessment was requested.
The patient required emergency drainage of the bile duct, so he was taken to the operating room for open surgical drain. Due to hemodynamic instability, only one choledocotomy and instrumentation with Randall forceps were performed. During the procedure, a dilated bile duct (25 mm) was observed, and a 20mm faceted stone was removed. In addition, the bile duct was washed using a Nélaton probe, which advanced easily to the duodenum. Due to the urgency of the procedure, a cholangiography was not performed, and finally a choledochorraphy and closure with T-tube drainage was carried out.
During the postoperative period, the patient remained in the ICU for several days, with inotropic support and on mechanical ventilation. Once the emergency was resolved and based on the good evolution of the patient, a cholangiography was performed through the T-tube (January 9, 2019), identifying a filling defect in the distal portion of the bile duct, which reached a diameter of 18 mm, suggesting the presence of a stone. There was no evidence of the passage of the contrast agent within the intestinal loops. Consequently, biliary obstruction, apparently secondary to choledocholithiasis, was diagnosed (Figure 2).
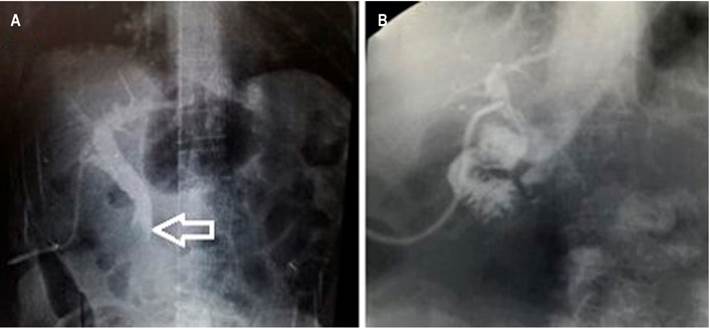
Figure 2 A. Dilation of the bile duct and the giant stone that prevents the passage of the agent into the duodenum. B. Cholangiography after combined instrumentation, without finding filling defects or proper passage of the agent into the duodenum.
Based on the results, combined instrumentation of the bile duct was carried out by the general surgery and the gastroenterology services through T-tube and endoscopy, respectively. The procedure was performed in the fluoroscopy room, for which a Dormia basket and a mechanical lithotriptor were inserted through the T-tube. As a result, partial fragmentation was achieved, and fragments were advanced into the duodenum.
Also, by the endoscopic route, stones were fragmented and extracted by means of a Dormia basket (Figure 3) and an extraction balloon. A cholangiography was performed using the T-tube, and an adequate passage of the contrast agent into the duodenum was observed, without extravasation, nor evidence of residual stones (Figure 2B).
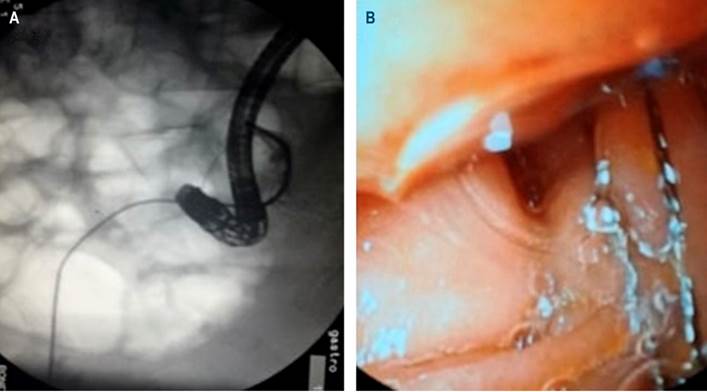
Figure 3 A. Combined instrumentation fluoroscopy. B. Duodenoscopic view of the Dormia basket inserted through the T-tube.
The patient had a good evolution, and, before discharging him, another cholangiography was performed through the T-tube, as well as a liver panel, obtaining normal results.
Discussion
Cholelithiasis is an endemic disease that affects up to 20% of the population in both eastern and western countries 7,8. Between 10-20% of these patients may develop choledocholithiasis simultaneously. About half of the people with cholelithiasis are asymptomatic and do not require surgery. However, people with choledocholithiasis must be treated given the risk of developing acute pancreatitis or cholangitis due to pancreatic or biliary flow obstruction 9.
For years, the diagnosis of choledocholithiasis was confirmed by ERCP. However, at present, this diagnosis is relatively easy to reach and can be confirmed by MRC or endoscopic ultrasound (EUS). In most cases, choledocholithiasis is secondary to the migration of stones from the gallbladder, and in very few cases, it is associated with primary or de novo formation of stones in the bile duct 7.
In 1889, in New York, Robert Abbe performed the first choledocotomy, as well as the first exploration of the bile duct 10. Since then, and for nearly a century, cholecystocholedocholithiasis was treated in a single surgical time by means of open surgery. During the first years of laparoscopic cholecystectomy (LAP CHOLE), laparoscopic bile duct exploration favored the performance of ERCP. Therefore, this technique became the gold standard, and the treatment of cholecystocoledocholithiasis passed from being one stage to two stages treatment.
Although the success rate is high (87-97%), between 5 and 10% of patients require two or more ERCPs 1,2,7. When the resolution of choledocholithiasis is not achieved, a surgical, laparoscopic, or open, exploration should be performed.
Currently, the treatment of choledocholithiasis, whether primary or secondary, is carried out through open or laparoscopic surgery (simultaneously or in a single surgical time in the case of cholelithiasis) or using endoscopy alone or combined with other surgical techniques in the case of choledocholithiasis (sequential or in two stages) 11.
In a meta-analysis that included 16 randomized studies comparing the use of open surgery, laparoscopic surgery, and techniques combined with endoscopy (LAP CHOLE plus ERCP) for the treatment of choledocholithiasis, no significant differences were found in terms of morbidity (13-20%) and mortality (0-3%). However, a lower percentage of recurrent stones was identified in the open surgery groups (6%), compared to the LAP CHOLE and ERCP groups (16%). From these results, it was concluded that the open surgery technique appeared to be superior to the combined technique in the treatment of choledocholithiasis, although the former was associated with a longer hospital stay 9,12. The laparoscopic technique had the advantage of being more cost-effective and did not show morbidity and mortality associated with ERCP 13.
On the other hand, due to improvements in materials and in the laparoscopic technique, as of now laparoscopic bile duct exploration (LBDE) has been performed in many countries for several years. With this technique, cholecystocoledocolithiasis is resolved in a single surgical time, with all the benefits of laparoscopy and without the inconveniences related to ERCP 14.
ERCP and laparoscopic methods for bile duct exploration are not available in many hospitals due to the lack of equipment or trained medical staff. The exploration of the bile duct should be carried out according to the resources and experience of the personnel available at each health care institution and, although open surgery is an invasive method, it should not be considered obsolete since it is still useful in difficult cases or during procedures that require conversion to the open surgery technique 13,14.
Once choledocholithiasis is resolved, the common bile duct) can be sutured (or choledochlorography) as traditionally done during open surgery by inserting a T-tube into the bile duct through the incision in the common bile duct. This allows splinting the bile duct and achieving a secure suture to prevent the leakage of bile or the formation of intra-abdominal collections since this favors the formation of a fistula. Moreover, it allows decompression of the bile duct if the pressure in the sphincter of the duodenal papilla increases and, in the case of residual stones, it allows the re-exploration of the bile duct, thus avoiding a new ERCP or surgical reintervention 15,16.
Initially, T-tube placement was an essential part of the laparoscopic technique, but recent studies have shown that choledochorography on a transpapillary biliary prosthesis by laparoscopy is an effective and safe method for the one-stage treatment of cholecystocoledocholithiasis. This way, all complications related to the handling of the T-tube are avoided, and a shorter hospital stay is achieved. In fact, some authors consider that the T-tube should only be used in cases in which it is technically impossible to place the biliary prosthesis 17.
Other authors propose to perform a primary closure following laparoscopic bile duct exploration based on a meta-analysis in which 12 studies were included. According to said meta-analysis, the routine use of the T-tube is not justified considering the morbidity rates related to its use, compared to the very low morbidity reported in patients who undergo primary closure 18,19.
Thus, the exploration of the bile duct and the performance of laparoscopic choledocoduodenostomy by experts has proven to be effective and safe in the treatment of complex cases of choledocholithiasis (multiple choledocholithiasis, impacted stones, stones in liver ducts, biliary stenosis, and recurrent choledocholithiasis) or failed ERCP scenarios. This surgical technique has also associated with a short hospital stay 20.
In patients with sepsis of biliary origin and hemodynamic instability, emergency treatment consists of biliary drainage, which can be done percutaneously, endoscopically (ERCP), or surgically, as well as laparoscopically or openly, as was the case with our patient.
Endoscopic technique: ERCP
Postoperative ERCP is indicated in cases where LBDE has not been successful or when the presence of stones is identified by T-tube cholangiography after surgery, which can occur in up to 2.5 % of patients 21. 85-90 % of bile duct stones can be successfully treated by the standard endoscopic technique, with the performance of a sphincterotomy and using a balloon and a Dormia basket 22.
Endoscopic sphincterotomy (ES) of the papilla was simultaneously described in 1974 by both Classen and Demling in Germany, and Kaway in Japan. This technique consists of cutting the sphincter of Oddi to allow the extraction of stones by pulling them with baskets or balls 23,24. Thus, the main causes of failed ERCP are large stones (>2 cm.), their impaction, and distal narrowing of the bile duct. In such cases, the use of additional techniques is necessary 22,25.
Rendezvous technique
The rendezvous technique was first described in 1998 26. However, the first combined treatment including surgical and endoscopic instrumentation of the bile duct was performed by Dr. Rodolfo Mazzariello. In 1976, he and Dr. Magnanini performed an endoscopic papillotomy in Buenos Aires (Argentina), which consisted of advancing a papillotome through a T-tube fistula. The papillotome was recovered and located by endoscopy to perform the electrical cut, and then, the stone was spontaneously eliminated 27.
Before this, Dr. Mazzariello had described the technique that bears his name, and that was used by many surgeons. It consists of exploring and extracting the stones from the bile duct through the T-tube or the fistula formed by it 28.
Some modifications of the rendezvous technique have been described in the literature. An example of such changes is when patients who have undergone surgery have a T-tube in the bile duct, and the guide is advanced through that tube; it is subsequently recovered through endoscopy, and then sphincterotomy and exploration of the bile ducts are performed 29.
However, in the case reported here, the availability of the T-tube allowed successful treatment in a patient with choledocholithiasis that was difficult to manage and in which ERCP was unsuccessful for this purpose. This treatment was achieved by means of the combined technique of instrumentation of the biliary tract —Dormia basket and the lithotripter through the T-tube— and instrumentation utilizing an ERCP with Dormia Basket and extraction balloon.
The use of percutaneous transhepatic cholangiography (PTHC) has been described as part of a modified rendezvous technique. Here, the guide is advanced through the PTHC and then recovered in the duodenum; finally, sphincterotomy is performed 30,31.
Giant or difficult stones
Between 10-15% of patients with choledocholithiasis have giant stones (10-15 mm). Although challenging, their extraction can be done endoscopically and, in most cases, using multiple techniques 32.
Staritz first described the balloon dilation (BD) technique in 1982 33. It involves the dilation of the biliary sphincter with balloons of up to 10mm in diameter without performing a prior sphincterotomy. It is intended to replace endoscopic sphincterotomy (ES) for stone extraction. In 2004, a randomized study reported an incidence of pancreatitis of 15.4% when BD was performed, compared to 0.8% with ES 34.
Some meta-analyses published later concluded that the use of BD for stone extraction, compared to ES, is associated with a lower rate of therapeutic success and a greater need for mechanical lithotripsy (ML). For all these reasons, BD is not recommended as a routine method for stone extraction, but it is a reasonable option in patients with coagulopathy, periampullary diverticulum, or a history of Billroth II operation 35.
Thus, ML achieves stone fragmentation in about 95% of cases; in the remaining patients, failure is explained by the inadequate opening of the lithotripter in the bile duct or the difficulty of capturing the stone due to its shape or size 36.
On the other hand, endoscopic sphincterotomy plus large-balloon dilation (ES-LBD) was described by Esroz in 2003 for the treatment of difficult stones. This technique has been successful in 89-95% of patients. The procedure consists of performing a sphincterotomy and dilating the orifice of the duodenal papilla with 12-20mm diameter balloons, which causes great dilation of the papillary orifice and facilitates the extraction of large or difficult stones 25,37.
Currently, ES-LBD is considered an effective and safe procedure for the treatment of complicated choledocholithiasis. This method reduces the need for lithotripsy and repeated ERCP sessions. Proper patient selection and some technical considerations are important to reduce the risk of complications 36-39.
Generally, large or impacted stones are handled with fragmentation techniques such as ML. In failed cases, treatment consists of either electrohydraulic lithotripsy (EHL), extracorporeal shock wave lithotripsy (ESWL) —which is helpful in patients with anatomical abnormalities such as those with Billroth II or Roux-en-Y operations—, or laser lithotripsy (LL), which is guided by conventional cholangioscopy.
In recent years, Spyglass® has become available. With this technique, through direct cholangioscopy, a single operator can perform a diagnostic or therapeutic procedure with EHL or laser in the bile and pancreatic duct. Moreover, it allows a better visual field, as well as a superior endoscopic image. Nevertheless, its disadvantage is its high cost, limiting its use in most medical centers 22.
Conclusions
Cholecystectomy, as well as open common bile duct exploration, continue to be performed in various hospitals in our country, given the lack of resources and, at times, the lack of training or expertise.
In addition, in leading medical centers, open or laparoscopic exploration of the bile duct is limited to patients in whom, for multiple reasons —and despite the wide variety of techniques currently available to treat choledocholithiasis—, such procedure has been impossible to perform.
The use of the T-tube remains useful in patients who are taken to surgical exploration of the bile duct. In cases of persistent choledocholithiasis, it facilitates the exploration and resolution of choledocholithiasis, along with endoscopic methods.
REFERENCES
1. Bansal VK, Misra MC, Rajan K, Kilambi R, Kumar S, Krishna A, Kumar A, Pandav CS, Subramaniam R, Arora MK, Garg PK. Single-stage laparoscopic common bile duct exploration and cholecystectomy versus two-stage endoscopic stone extraction followed by laparoscopic cholecystectomy for patients with concomitant gallbladder stones and common bile duct stones: a randomized controlled trial. Surg Endosc. 2014;28(3):875-85. http://doi.org/10.1007/s00464-013-3237-4 [ Links ]
2. Ding G, Cai W, Qin M. Single-stage vs. two-stage management for concomitant gallstones and common bile duct stones: a prospective randomized trial with long-term follow-up. J Gastrointest Surg. 2014;18(5):947-951. http://doi.org/10.1007/s11605-014-2467-7 [ Links ]
3. Hungness ES, Soper NJ. Management of common bile duct stones. J Gastrointest Surg. 2006;10(4):612-619. http://doi.org/10.1016/j.gassur.2005.08.015 [ Links ]
4. Xiao LK, Xiang JF, Wu K, Fu X, Zheng MY, Song XX, Xie W. The reasonable drainage option after laparoscopic common bile duct exploration for the treatment of choledocholithiasis. Clin Res Hepatol Gastroenterol. 2018;42(6):564-569. http://doi.org/10.1016/j.clinre.2018.07.005 [ Links ]
5. Xu Y, Dong C, Ma K, Long F, Jiang K, Shao P, Liang R, Wang L. Spontaneously removed biliary stent drainage versus T-tube drainage after laparoscopic common bile duct exploration. Medicine (Baltimore). 2016;95(39):e5011. http://doi.org/10.1097/MD.0000000000005011 [ Links ]
6. Yin Z, Xu K, Sun J, Zhang J, Xiao Z, Wang J, Niu H, Zhao Q, Lin S, Li Y. Is the end of the T-tube drainage era in laparoscopic choledochotomy for common bile duct stones is coming? A systematic review and meta-analysis. Ann Surg. 2013;257(1):54-66. http://doi.org/10.1097/SLA.0b013e318268314b [ Links ]
7. Costi R, Gnocchi A, Di Mario F, Sarli L. Diagnosis and management of choledocholithiasis in the golden age of imaging, endoscopy and laparoscopy. World J Gastroenterol. 2014;20(37):13382-13401. http://doi.org/10.3748/wjg.v20.i37.13382 [ Links ]
8. Everhart JE, Khare M, Hill M, Maurer KR. Prevalence and ethnic differences in gallbladder disease in the United States. Gastroenterology. 1999;117(3):632-639. http://doi.org/10.1016/s0016-5085(99)70456-7 [ Links ]
9. Dasari BV, Tan CJ, Gurusamy KS, Martin DJ, Kirk G, McKie L, Diamond T, Taylor MA. Surgical versus endoscopic treatment of bile duct stones. Cochrane Database Syst Rev. 2013;(9):CD003327. http://doi.org/10.1002/14651858.CD003327.pub3 [ Links ]
10. Verbesey JE, Birkett DH. Common bile duct exploration for choledocholithiasis. Surg Clin North Am. 2008;88(6):1315-28. http://doi.org/10.1016/j.suc.2008.08.002 [ Links ]
11. Restrepo C, Sierra S, Penagos S, Palacios OG, Mendoza MC. Manejo sincrónico de la colecistocoledocolitiasis, ¿seguro? Rev Colomb Cir. 2014;29(3):197-203. [ Links ]
12. Clayton ES, Connor S, Alexakis N, Leandros E. Meta-analysis of endoscopy and surgery versus surgery alone for common bile duct stones with the gallbladder in situ. Br J Surg. 2006;93(10):1185-1191. http://doi.org/10.1002/bjs.5568 [ Links ]
13. Rogers SJ, Cello JP, Horn JK, Siperstein AE, Schecter WP, Campbell AR, Mackersie RC, Rodas A, Kreuwel HT, Harris HW. Prospective randomized trial of LC+LCBDE vs ERCP/S+LC for common bile duct stone disease. Arch Surg. 2010;145(1):28-33. http://doi.org/10.1001/archsurg.2009.226 [ Links ]
14. Berggren U, Gordh T, Grama D, Haglund U, Rastad J, Arvidsson D. Laparoscopic versus open cholecystectomy: hospitalization, sick leave, analgesia and trauma responses. Br J Surg. 1994;81(9):1362-1365. http://doi.org/10.1002/bjs.1800810936 [ Links ]
15. Williams JA, Treacy PJ, Sidey P, Worthley CS, Townsend NC, Russell EA. Primary duct closure versus T-tube drainage following exploration of the common bile duct. Aust N Z J Surg. 1994;64(12):823-826. http://doi.org/10.1111/j.1445-2197.1994.tb04556.x [ Links ]
16. Palermo M, Giménez M, Álvarez F, Ortega A, Bruno M, Tarsitano FJ. Abordaje transfistular para el tratamiento de la litiasis residual de la vía biliar. Acta Gastroenterol Latinoam. 2010;40(3):239-243. [ Links ]
17. Martínez D, Parra P, Díaz D, Lorente JM. Exploración laparoscópica de la vía biliar y coledocorrafia sobre prótesis biliar: dejando atrás el tubo de Kehr. Rev Esp Enferm. 2013;105(3):125-130. http://dx.doi.org/10.4321/S1130-01082013000300002 [ Links ]
18. Gurusamy KS, Koti R, Davidson BR. T-tube drainage versus primary closure after laparoscopic common bile duct exploration. Cochrane Database Syst Rev. 2013;(6):CD005641. http://doi.org/10.1002/14651858.CD005641.pub3 [ Links ]
19. Liu JG, Wang YJ, Shu GM, Lou C, Zhang J, Du Z. Laparoscopic versus endoscopic management of choledocholithiasis in patients undergoing laparoscopic cholecystectomy: a meta-analysis. J Laparoendosc Adv Surg Tech A. 2014;24(5):287-294. http://doi.org/10.1089/lap.2013.0546 [ Links ]
20. Senthilnathan P, Sharma D, Sabnis SC, Srivatsan Gurumurthy S, Senthil Anand E, Nalankilli VP, Anand Vijai N, Praveen Raj P, Parthasarathy R, Rajapandian S, Palanivelu C. Laparoscopic choledochoduodenostomy as a reliable rescue procedure for complicated bile duct stones. Surg Endosc. 2018;32(4):1828-1833. http://doi.org/10.1007/s00464-017-5868-3 [ Links ]
21. Anwar S, Rahim R, Agwunobi A, Bancewicz J. The role of ERCP in management of retained bile duct stones after laparoscopic cholecystectomy. N Z Med J. 2004;117(1203):U1102. [ Links ]
22. Gómez M, Gutiérrez O, Jaramillo M. Manejo del cálculo difícil en la vía biliar: serie de casos. Rev Col Gastroenterol. 2015;30(4):461-468. https://doi.org/10.22516/25007440.10 [ Links ]
23. Classen M, Demling L. Endoskopische Sphinkterotomie der Papilla Vateri und Steinextraktion aus dem Ductus choledochus. Dtsch Med Wochenschr 1974;99(11): 496-497. https://doi.org/10.1055/s-0028-1107790 [ Links ]
24. Kawai K, Akasaka Y, Murakami K, Tada M, Koli Y. Endoscopic sphincterotomy of the ampulla of Vater. Gastrointest Endosc. 1974;20(4):148-151. http://doi.org/10.1016/s0016-5107(74)73914-1 [ Links ]
25. Ersoz G, Tekesin O, Ozutemiz AO, Gunsar F. Biliary sphincterotomy plus dilation with a large balloon for bile duct stones that are difficult to extract. Gastrointest Endosc. 2003;57(2):156-159. http://doi.org/10.1067/mge.2003.52 [ Links ]
26. Cavina E, Franceschi M, Sidoti F, Goletti O, Buccianti P, Chiarugi M. Laparo-endoscopic “rendezvous”: a new technique in the choledocholithiasis treatment. Hepatogastroenterology. 1998;45(23):1430-1435. [ Links ]
27. Mazzariello R. Tratamiento instrumental postoperatorio de la patología biliar no litiásica. Rev Arg Cir. 1978;34:21-25. [ Links ]
28. Mazzariello RM. Transcholecystic extraction of residual calculi in common bile duct. Surgery. 1974;75(3):338-347. [ Links ]
29. Odabasi M, Yildiz MK, Abuoglu HH, Eris C, Ozkan E, Gunay E, Aktekin A, Muftuoglu MT. A modified Rendezvous ERCP technique in duodenal diverticulum. World J Gastrointest Endosc. 2013;5(11):568-73. http://doi.org/10.4253/wjge.v5.i11.568 [ Links ]
30. Lee JH, Kim HW, Kang DH, Choi CW, Park SB, Kim SH, Jeon UB. Usefulness of percutaneous transhepatic cholangioscopic lithotomy for removal of difficult common bile duct stones. Clin Endosc. 2013;46(1):65-70. http://doi.org/10.5946/ce.2013.46.1.65 [ Links ]
31. Meek J, Fletcher S, Crumley K, Culp WC, Meek M. Percutaneous rendezvous technique for the management of a bile duct injury. Radiol Case Rep. 2017;13(1):175-178. http://doi.org/10.1016/j.radcr.2017.11.004 [ Links ]
32. Garzón MA, Hernández G, Pérez O, Martínez JD, Molano JC, Marulanda JC, Lizarazo JI, Hormaza N, Rey MH. Factores asociados con el uso de litotripsia mecánica en pacientes con cálculos gigantes de la vía biliar: ¿puede la dilatación papilar con balón grande disminuir su requerimiento? Rev Col Gastroenterol. 2017;32(3):202-208. http://doi.org/10.22516/25007440.151 [ Links ]
33. Staritz M, Ewe K, Meyer zum Büschenfelde KH. Endoscopic papillary dilatation: an alternative to papillotomy? Dtsch Med Wochenschr. 1982;107(23):895-897. http://doi.org/10.1055/s-2008-1070041 [ Links ]
34. Disario JA, Freeman ML, Bjorkman DJ, Macmathuna P, Petersen BT, Jaffe PE, Morales TG, Hixson LJ, Sherman S, Lehman GA, Jamal MM, Al-Kawas FH, Khandelwal M, Moore JP, Derfus GA, Jamidar PA, Ramirez FC, Ryan ME, Woods KL, Carr-Locke DL, Alder SC. Endoscopic balloon dilation compared with sphincterotomy for extraction of bile duct stones. Gastroenterology. 2004;127(5):1291-9. http://doi.org/10.1053/j.gastro.2004.07.017 [ Links ]
35. ASGE Standards of Practice Committee, Maple JT, Ikenberry SO, Anderson MA, Appalaneni V, Decker GA, Early D, Evans JA, Fanelli RD, Fisher D, Fisher L, Fukami N, Hwang JH, Jain R, Jue T, Khan K, Krinsky ML, Malpas P, Ben-Menachem T, Sharaf RN, Dominitz JA. The role of endoscopy in the management of choledocholithiasis. Gastrointest Endosc. 2011;74(4):731-44. http://doi.org/10.1016/j.gie.2011.04.012 [ Links ]
36. García VA, Zárate AM, Corral A, Pérez A. Manejo actual de la coledocolitiasis. Rev Med Hosp Gen Mex. 1999;62(2):121-127. [ Links ]
37. Jeong SU, Moon SH, Kim MH. Endoscopic papillary balloon dilation: revival of the old technique. World J Gastroenterol. 2013;19(45):8258-8268. http://doi.org/10.3748/wjg.v19.i45.8258 [ Links ]
38. Espinoza J, Aliaga M, Rodríguez J, Miraval E, Zegarra A, Bravo E, Prochazka R. Esfinterotomía seguida de dilatación con balón de gran tamaño en el manejo de coledocolitiasis. Eficacia y seguridad en un hospital de Lima-Perú. Rev Gastroenterol Perú. 2016;36(3):203-208. [ Links ]
39. Marín L, Vera A, Gómez A, Cervera Z, Dávalos M, Alva E, Palacios F, Díaz R, Guzmán E, García G. Dilatación con balón de gran diámetro en el manejo de coledocolitiasis de difícil extracción: experiencia clínica. Rev Gastroenterol Perú. 2016;36(4):330-335. [ Links ]
Citation: Prieto-Ortiz RG, Duarte-Osorio AI, García-Echeverri P, Ballén-Párraga H. Treatment of choledocholithiasis by ERCP, and instrumentation through a T-tube. Rev Colomb Gastroenterol. 2020;35(3):382-389. https://doi.org/10.22516/25007440.385
Received: April 02, 2019; Accepted: July 05, 2019











 text in
text in 



