Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista colombiana de Gastroenterología
Print version ISSN 0120-9957On-line version ISSN 2500-7440
Rev. colomb. Gastroenterol. vol.35 no.4 Bogotá Oct./Dec. 2020 Epub July 12, 2021
https://doi.org/10.22516/25007440.504
Original article
Zenker’s diverticulum: endoscopic treatment with or without diverticulotome
1Médico Internista y Gastroenterólogo. Unidad de Gastroenterología y Ecoendoscopia (UGEC). Hospital Universitario Nacional de Colombia. Profesor asociado de Medicina, Universidad Nacional de Colombia. Bogotá, Colombia
2Médico Internista y Gastroenterólogo. Unidad de Gastroenterología y Ecoendoscopia (UGEC). Hospital Universitario Nacional de Colombia. Bogotá, Colombia
3Médico Internista y Gastroenterólogo, Universidad Nacional de Colombia. Hospital Universitario Nacional de Colombia. Bogotá, Colombia
Zenker’s diverticulum is defined as a diverticulum located in the posterior esophageal wall, just above the cricopharyngeal muscle. Most patients experience symptoms in this area after the age of 60. In the past, the standard treatment was surgical diverticulotomy, but endoscopic treatment was introduced over 20 years ago. For more than 15 years, overtubes are introduced to facilitate the procedure, but their use is not been widely established in our country. Therefore, this study aims to evaluate whether endoscopic diverticulotomy with the use of this device is easier (faster) than the standard method.
Materials and methods:
A prospective study was conducted to establish which of the two endoscopic methods to treat Zenker’s diverticulum (ZD) made the septum incision time shorter. The time count was done using video recording and started when the probe —standard method (SM)— or the overtube (MD) were placed, as this is the exact moment when septum cutting begins. The count stopped when the cut was finalized.
Results:
A total of 20 patients were treated from January 2015 to December 2018. Zenker’s diverticulum diagnosis was achieved by endoscopy and esophagogram to classify the size of the tumor. The average age of the patients was 61 years (46-85). Ten patients were assigned to each group. Symptoms resolved in 7 patients of the SM group, compared to 9 in the MD group. The three patients who did not respond to the treatment were classified as stage II in the functional outcome swallowing scale at 18 months of follow-up. The average time of the procedure was 32 (25-45) minutes in the SM group and 12 (7-15) minutes in the MD group (p <0.001).
Conclusions:
ZD myotomy with flexible endoscopy using an overtube has potential benefits in terms of shorter operative times, shorter post-operative stays, and an earlier reintroduction of food. From a technical point of view, this method allows for better exposure of the septum, which facilitates cutting. However, more extensive studies are needed to confirm these results.
Keywords: Dysphagia; Zenker; endoscopic diverticulotomy; diverticulotome; complications
El divertículo de Zenker se define como un divertículo localizado en la pared esofágica posterior que tiene como cuello proximal al músculo cricofaríngeo. La mayoría de los pacientes presenta síntomas después de los 60 años de edad. Antes el manejo estándar se realizaba la diverticulotomía quirúrgica, pero desde hace más de 20 años se introdujo el manejo endoscópico. Desde hace más de 15 años se introdujo un diverticulotomo que facilita la realización del procedimiento, pero su uso no se ha instaurado ampliamente en Colombia. Por ello, el objetivo de este estudio es evaluar si la diverticulotomía endoscópica con el uso de este dispositivo es más fácil (rápida) que el método estándar.
Materiales y métodos:
se realizó un estudio prospectivo evaluando dos métodos endoscópicos para tratar el divertículo de Zenker, con el objetivo principal de conocer en cuál de ellos el tiempo de incisión del tabique era menor. El tiempo del procedimiento se contaba después de la colocación de la sonda en el método estándar o después de colocar el diverticulotomo en posición (método con diverticulotomo), ya que es el momento exacto en el cual se inicia el corte del tabique y se contabilizaba el tiempo (registro en video) cuando este corte terminaba.
Resultados:
de enero de 2015 a diciembre de 2018 en total se incluyeron 20 pacientes. El diagnóstico de Zenker fue realizado por una endoscopia y esofagograma para clasificar el tamaño del mismo. El promedio de edad de los pacientes fue de 61 años (46-85). En cada uno de los grupos se asignaron 10 pacientes. En 7 pacientes del grupo método estándar se resolvieron los síntomas, en comparación con 9 del grupo del método con diverticulotomo. Los tres pacientes que no respondieron presentaron en el seguimiento a 18 meses un estadio II de la escala de deglución de resultados funcionales. El tiempo promedio del procedimiento fue de 32 (25-45) minutos en el grupo del método estándar y 12 (7-15) minutos en el grupo de método con diverticulotomo (p < 0,001).
Conclusiones:
La miotomía del divertículo de Zenker con el uso de endoscopia flexible utilizando el diverticulotomo tiene beneficios potenciales en términos de tiempos operatorios más cortos, estancias posoperatorias más cortas y un inicio más temprano de la dieta. Desde el punto de vista técnico, permite una mejor exposición del tabique, lo que facilita su corte, pero se necesitan estudios más grandes para confirmar estos resultados.
Palabras claves: Disfagia; Zenker; diverticulotomía endoscópica; diverticulotomo; complicaciones
Introduction
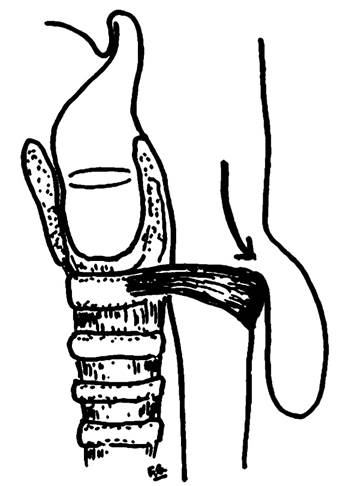
Zenker’s diverticulum is a pulsion diverticulum that, due to its critical location, causes dysphagia. Since it prevents proper nutrition and triggers symptoms such as regurgitation, chronic cough, and weight loss, it has a direct negative impact on the patients’ quality of life. This condition is also associated with other complications, the most severe being recurrent aspiration, which results in recurrent pneumonias and, consequently, a high rate of morbidity and mortality1. The anatomical region where it is located is called the Killian triangle, which is in the posterior wall of the hypopharynx, between the inferior pharyngeal constrictor muscle and the transverse fibers of the cricopharyngeal muscle (Figure 1)2. Zenker’s diverticulum was named after the German pathologist Friedrich Albert von Zenker, who, together with von Ziemssen, reported 23 cases at the University of Erlangen in 1878 and defined it as “a hernia of the posterior hypopharyngeal membrane proximal to the upper sphincter of the esophagus”. However, it should be noted that it was first described in 1769 by Dr. Abraham Ludlow, and not by Dr. Zenker3,4.
From a pathophysiological perspective, it is a pulsion diverticulum caused by an increase of intraluminal pressure, resulting in mucosal and submucosal prolapse (hence the term pseudodiverticulum) in Killian’s triangle, where a normally low wall tone is associated with relatively low pressures in the adjacent retropharyngeal space, leading to diverticulum formation in the posterior part (Figure 1). However, it is not yet clear what are the forces contributing to the increase in luminal pressures, so manometric measurement is considered a challenge due to the asymmetry of the sphincter pressure and its wide range of motion5,6. Zenker’s diverticulum is a rare disorder (with incidence rates ranging from 0.01% to 0.11% in the general population), but its true incidence rate is difficult to determine due to variations in the severity of symptoms, although it is more prevalent in men between the seventh and eighth decades of life6,7. Dysphagia is the cardinal symptom, and two causal mechanisms are known: incomplete opening of the upper esophageal sphincter and extrinsic compression of the cervical esophagus by the diverticulum itself. From a clinical standpoint, cervical borborygmi, particularly in the presence of a palpable mass in the neck, is almost pathognomonic of Zenker’s diverticulum, although it is not a frequent finding8. Warning signs such as local pain and hemoptysis or hematemesis may indicate ulceration or squamous cell carcinoma within Zenker’s diverticulum, with an incidence rate between 0.4% and 1.5%6,9.
Videofluoroscopic swallowing study is useful for its diagnosis because it provides information on size and location of the diverticulum and sometimes mucosal lesions in the diverticular pouch can be identified10,11. In addition, it allows making a differential diagnosis of the less common and smaller Killian-Jamieson diverticulum, which occurs in the anterolateral wall of the proximal esophagus and below the cricopharyngeal muscle12. Although useful, the diagnostic performance of modified barium swallow is conditioned by variations in quality of its execution and interpretation. Performing upper gastrointestinal endoscopy is necessary to rule out the presence of squamous cell carcinoma13 and is essential to describe the anatomy of the diverticulum and, therefore, guide the therapeutic strategy.
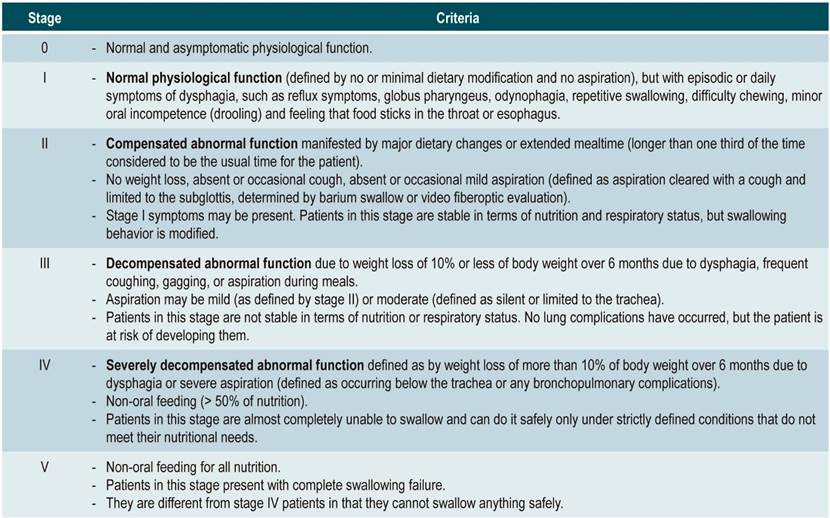
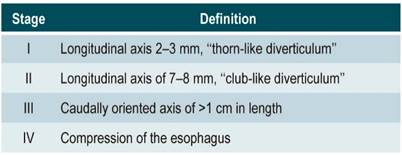
Several classification systems based on size and morphology have been proposed, including the Brombart classification (Table 1)14) and the Morton/Bartley classification (Table 2)15.
Table 1 Brombart classification (size and morphology of diverticula)14
Taken from: Mantsopoulos K et al. EUR Arch Otorhinolaryngol. 2014;271(3):583-8.
Table 2 Morton/Bartley Classification (Size)15
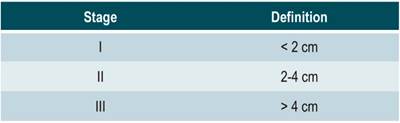
Taken from: Miller FR, Taylor C. Zenker’s Diverticulum: Endoscopic Surgical Management Options. Clin Surg. 2017;2:1422.
Surgical treatment has been described since the 19th century, with an approach to hernia treatment. Cricopharyngeal myotomy was only recently (over the last decades) implemented and, more recently, endoscopic septotomy has been recognized as a fundamental technique in correcting Zenker’s diverticulum, showing improvement in relation to food retention (liquids and solids) and suppression of all or the vast majority of symptoms after being performed15. However, both open and endoscopic transcervical approaches are associated with potential complications and risks that are less frequent with the endoscopic technique, which is why the latter is the first option for treatment, considering that these patients are usually malnourished, older, and almost always present with associated comorbidities, which significantly increases surgical risk16-18.
Materials and methods
A prospective study comparing two endoscopic methods to treat Zenker’s diverticulum was conducted to know which method allows shorter septum incision times, resulting in a shorter procedure (surgical and anesthetic time) and reduced risk of morbidity and mortality.
Secondary objectives of the study included the evaluation of symptom resolution according to the functional outcome swallowing scale (FOSS), which was assessed before and after the procedure, as well as the evaluation of the resolution of major complications such as bleeding (requiring transfusion support or endoscopic reintervention for control), perforation, and recurrence of symptoms with an average follow-up of 18 months.
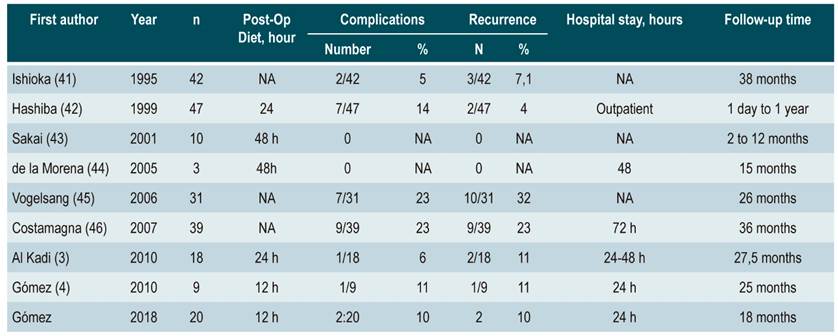
Patients who underwent diverticulotomy were clinically tested for dysphagia to solids or liquids, cough, regurgitation, globus pharyngeus, aspiration, weight loss, and need for supplemental nutrition, among others. A pre- and post-procedure FOSS score was established using the methodology for calculating this score described by Salassa (Table 3)19,20. Only FOSS stage II, III, IV, and V patients were considered, and a videofluoroscopic swallowing study was performed as a confirmatory diagnostic method using Brombart classification stages II, III, and IV (Table 1)21. To ensure a periodic balance in the number of subjects allocated to either of the two endoscopic diverticulotomy procedures (with or without diverticulum overtube), patients were randomized in blocks, also known as permuted block randomization. The procedure was timed from the moment the probe was placed in position in the usual method or after the diverticulum overtube was placed in the method that used this accessory (overtube method), since this is the moment when the septum is cut, until the cut was completed (video recording). The details of how the procedure was performed in each group are described below.
Standard method
The procedure is performed under general anesthesia with the patient in a left lateral decubitus position. Adequate endoscopic exposure of the septum that separates the diverticulum from the esophageal lumen is a key element. It is usually accomplished by inserting a nasogastric tube (NGT), which is left in place during the procedure. The NGT protects the contralateral esophageal wall from thermal injury during septum transection. The endoscope is placed with a short cap and the septum of the diverticulum is cut with a pointed papillotome. After completing the cut, a hemoclip is placed at the vertex of the cut to prevent perforation of the mediastinum.
Method with diverticulum overtube
Dr. Deviere built a plastic diverticulum overtube (Figure 2) with two flaps: a long one that is placed in the esophagus and a short one that is placed in the diverticulum and exposes the septum, which is cut with the needle papillotome; the NGT and the cap are not needed, and the clip is placed at the end of the procedure (Figure 3). The diverticulum overtube may also be made in an endoscopy unit using a colonic or enteroscopy overtube (Figure 4); it should be noted that the flap left in the esophagus (the long flap) is 3 cm long and the one left in the diverticulum is 2 cm long.

Figure 3 Zenker’s diverticulum with an overtube clearly separating the septum, which has been cut with a pointed scalpel.
Results
A total of 20 patients treated from January 2015 to December 2018 were included. In all of them, the main symptom was dysphagia to solids and liquids. Zenker’s diverticulum diagnosis was achieved by initial endoscopy, and an esophagogram was performed to classify the size of the tumor. Patients’ average age was 61 years (46-85 years), there was only one woman (curiously, the youngest patient, 46 years). Ten patients were assigned to each group. The average size of the diverticulum was 3.5 cm (2.5-7.0; stage III according to the Brombart classification), which was similar in both groups. Participants were assessed using the FOSS and were as stages II-III patients. Symptoms were resolved in 7 patients in the standard method group vs. 9 in the diverticulum overtube method group (stage 0 of the FOSS, minimum follow-up time: 18 months). The three patients who did not respond to the standard treatment method were classified as stage II according to the FOSS at 18 months of follow-up. One patient in the standard method group presented emphysema as a complication, but no perforation was evident and was treated conservatively; two experienced bleeding and required the use of the coagulation clamp with adequate control. No complications were reported in the diverticulum overtube method group, and only one patient reported odynophagia 15 days after the procedure was carried out; when endoscopy was done, it was discovered that the hemoclip remained in place but impacted against the contralateral wall, so it was removed, and the patient’s condition improved immediately. The average time of the procedure was 32 (25-45) minutes in the standard method group versus 12 (7-15) minutes in the overtube method group (p <0.001).
Discussion
Zenker’s diverticulum generally occurs between the seventh and eighth decades of life and it rarely does before the age of 406,22. Its estimated annual incidence is 2 per 100 000 inhabitants, and its onset is associated with aging, affecting men predominantly. Its prevalence in the general population ranges between 0.01 % and 0.11 % and varies depending on the geographical region; for example, it is more common in northern Europe than in southern Europe and is occurrence frequency in the United States, Canada, and Australia is higher, but lower in Japan and Indonesia. However, these data only include symptomatic cases, so the number of patients with asymptomatic Zenker’s diverticulum is unknown to date6,23. Before a diagnosis is made, symptoms can be present for weeks or years. Although it has been linked to a wide range of symptoms, 80% to 90% of patients complain of dysphagia, regurgitation, halitosis, esophageal mass sensation, persistent cough, odynophagia, throat clearing, and aspiration pneumonia22. It can also be an incidental finding in many cases, as it was the case in 17% of our patients, or patients can go to the emergency room with a foreign body, as it happened in 5% of our cases22.
Given its widespread availability, modified barium swallow with lateral views of the hypopharynx is the most suitable diagnostic study for confirming the diagnosis of Zenker’s diverticulum. However, dynamic continuous fluoroscopy is preferred (where available) because static imaging may be inadequate in patients with small diverticula. In addition, videofluoroscopic swallowing study allows assessing the presence of regurgitation and aspiration, as well as differentiating the Killian-Jamieson diverticulum (since it is unclear if the efficacy and safety of endoscopic treatment in these patients are comparable to those in patients with Zenker’s diverticulum)23-25. The Brombart classification allows classifying diverticulum involvement based on the results of these types of imaging studies (Table 1). However, the usual scenario is a patient who complains of dysphagia and is taken to upper gastrointestinal tract endoscopy. Due to the increased risk of perforation during the procedure, it is important to have a high level of suspicion of Zenker’s diverticulum in older adult patients who report complains of dysphagia26.
Therapeutic measures for this condition have been described since the 19th century. They are similar to those used for hernia treatment in that they include mobilization and removal of the diverticular pouch, with or without defect closure, or endoluminal inversion. Cricopharyngeal myotomy (current technique) was introduced later. Its approach may be transoral with self-contained sutures or more invasive, by lateral cervicotomy with or without cricopharyngeal myotomy; however, the latter is associated with complications such as mediastinitis, infection of the superficial operative site, recurrent laryngeal nerve palsy, and development fistulas, and is no longer used27,28. The main disadvantages of surgical resection are a higher rate of complications, such as recurrent laryngeal nerve palsy or hematoma, and longer hospital stay; however, up to 90% of patients have been confirmed to be symptom-free after undergoing surgical procedure29.
Endoscopic treatment of Zenker’s diverticulum has progressed steadily. Dr. Mosher was the first to use a rigid endoscope and separate the pouch from the esophageal wall in 1917 (with the occurrence of a complication due to mediastinitis). Subsequently, in 1932, the technique was modified by Seiffert, although Dohlman and Matson were successful in performing diverticulotomies via endoscopy. In 1982, Van Overbeek added the use of carbon dioxide (CO2) laser to the technique and, in 1993, Collard et al., in Belgium, and Martin-Hirsch and Newbegin, in the United Kingdom, independently reported the performance of a diverticulotomy using mechanical sutures28,30,31. The main advantages of flexible endoscopy, compared to surgical treatment options, are that it is safer, patients have shorter hospital stays (some may even be ambulatory), the overall success rate is of up to 90%, and symptom recurrence occurs in only 10.5% of patients32. The overall complication and mortality rates from flexible endoscopic Zenker’s diverticulotomy are 15% and 0%, respectively, and the most common complications are cervical emphysema (5.7 % do not need to be treated if there is no extravasation of medium), perforation (4.0 % usually resolve with clip placement), and bleeding (3.1 % are usually controlled during the same procedure)33-36.
The use of peroral endoscopic myotomy (POEM) has been recently described in the management of Zenker’s diverticulum (Z-POEM), with a clinical success rate of 92% and a perforation rate of 5.5%37. This technique has gained popularity in recent years, and its potential advantage over standard endoscopic septotomy is complete septum division, which reduces the risk of symptom recurrence. However, it should be noted that in the case of post-Z-POEM recurrence (theoretically lower), the management strategy is still unknown, especially given the possibility of subsequent submucosal fibrosis. These aspects should be considered when selecting patients; however, this method plays a leading and critical role today and in the near future37,38.
Table 4 shows the endoscopic series published so far compared to ours. It should be noted that our series is small, but significant to our context. Despite this, the success of the procedure and the low complication rate reported here are consistent what is currently reported. It is worth noting that although many authors perform this endoscopic procedure under sedation, we believe that it should always be performed under general anesthesia as it is better to have the patient completely immobile, since there is a potential risk of bleeding. Therefore, protecting the airway is recommended due to the risk of aspiration, which can be minimized in the initial phase by using coagulation current in the electrosurgical unit. Another useful measure consists of using an endoscopic laser scalpel (hook knife, triangle, ceramic tip, among others) instead of a precut papillotome because it is very thin and often binds to the tissue, requiring regular removal and reinsertion for cleaning. Another suggestion is to use a ceramic-tipped papillotome in the initial phase to support the septum and avoid esophageal wall perforation.
As shown in our study, the experience with endoscopic diverticulotomy using the diverticulum overtube has been highly satisfactory and resulted in a procedure that requires a significantly shorter time to be performed, which, in the context of this group of patients, who are usually considered to be at high surgical risk (due to age, comorbidities, nutritional status and increased fragility), makes a significant difference in their postoperative recovery, without affecting the procedure results in terms of symptom recurrence39,40. The mean procedure time in the standard method group was 3225-45 minutes versus only 127-15 minutes in the overtube method group (p<0.001), with no major variations in terms of complications or symptoms recurrence, and with comparable results to the cases series published in the literature. However, the proven safety of the method proposed here should be assessed prospectively in subsequent studies with larger sample sizes that allow performing a higher number of procedures to be evaluated.
Conclusion
Myotomy of Zenker’s diverticulum with flexible endoscopy using a diverticulum overtube has potential benefits in terms of shorter surgical times, shorter post-operative stays, and earlier food reintroduction. Technically, this method allows for a better exposure of the septum, which facilitates transection, although studies conducted in larger samples are required to validate these results.
REFERENCES
1. Tabola R, Lewandowski A, Cirocchi R, Augoff K, Kozminska U, Grabowski K. Zenker diverticulum: Experience in surgical treatment of large diverticula. Medicine (Baltimore). 2018;97(19):e0557. https://doi.org/10.1097/MD.0000000000010557 [ Links ]
2. Visser LJ, Hardillo JA, Monserez DA, Wieringa MH, Baatenburg de Jong RJ. Zenker’s diverticulum: Rotterdam experience. Eur Arch Otorhinolaryngol. 2016;273(9):2755-63. https://doi.org/10.1007/s00405-015-3825-0 [ Links ]
3. Al-Kadi A, Maghrabi A, Thomson D, MGillman L, Dhalla S. Endoscopic Treatment of Zenker. Diverticulum: Results of a 7-Year Experience. J Am Coll Surg. 2010;211(2):239-243. https://doi.org/10.1016/j.jamcollsurg.2010.04.011 [ Links ]
4. Gómez Z MA, Ardila SF, Arbeláez V. Experiencia en el manejo del divertículo de Zenker: Una serie de 18 casos. Rev Col Gastroenterol. 2011;26(2):100-105. [ Links ]
5. Ishaq S, Sultan H, Siau K, Kuwai T, Mulder CJ, Neumann H. New and emerging techniques for endoscopic treatment of Zenker’s diverticulum: State-of-the-art review. Dig Endosc. 2018;30(4):449-460. https://doi.org/10.1111/den.13035 [ Links ]
6. Law R, Katzka DA, Baron TH. Zenker’s Diverticulum. Clinical Gastroenterology and Hepatology. 2014;12(11):1773-1782. https://doi.org/10.1016/j.cgh.2013.09.016 [ Links ]
7. Ciuc D, Birlă R, Panaitescu E, Tanţău M, Constantinoiu S. Zenker Diverticulum Treatment: Endoscopic or Surgical? Chirurgia (Bucur). 2018;113(2):234-243. https://doi.org/10.21614/chirurgia.113.2.234 [ Links ]
8. Jones D, Aloraini A, Gowing S, Cools-Lartigue J, Leimanis M, Tabah R, Ferri L. Evolving Management of Zenker’s Diverticulum in the Endoscopic Era: A North American Experience. World J Surg. 2016;40(6):1390-6. https://doi.org/10.1007/s00268-016-3442-0 [ Links ]
9. Prisman E, Genden EM. Zenker diverticulum. Otolaryngol Clin North Am. 2013;46(6):1101-11. https://doi.org/10.1016/j.otc.2013.08.011 [ Links ]
10. Henry MA, Lerco MM, Tagliarini JV, Castilho EC, Novaes FT, Lamonica VC. Pharyngoesophageal diverticulum: evaluation of treatment results. Rev Col Bras Cir. 2013;40(2):104-9. https://doi.org/10.1590/S0100-69912013000200004 [ Links ]
11. Aghajanzadeh M, Yousefi-Mashhoor M, Delshad MAE, Massahnia S. Zenker’s Diverticulum: Report Rare Presentation and Management of Six Cases. Gastroenterol Hepatol Open Access 2016, 4(6): 00124. https://doi.org/10.15406/ghoa.2016.04.00124 [ Links ]
12. Stewart, KE, Smith DRK, Woolley SL. Simultaneously occurring Zenker’s diverticulum and Killian-Jamieson diverticulum: case report and literature review. Gastroenterol Hepatol Open Access. 2017;131(8),661-666. https://doi.org/10.1017/S0022215117001268 [ Links ]
13. Dina I, Ginghina O, Toderescu CD, Bălălău C, Galateanu B, Negrei C, Iacobescu C. Zenker’s diverticulum and squamous esophageal cancer: a case report. J Mind Med Sci. 2017;4(2):193-197. https://doi.org/10.22543/7674.42.P193197 [ Links ]
14. Mantsopoulos K, Psychogios G, Karatzanis A, Künzel J, Lell M, Zenk J, Koch M. Clinical relevance and prognostic value of radiographic findings in Zenker’s diverticulum. Eur Arch Otorhinolaryngol. 2014;271(3):583-8. https://doi.org/10.1007/s00405-013-2562-5 [ Links ]
15. Aiolfi A, Scolari F, Saino G, Bonavina L. Current status of minimally invasive endoscopic management for Zenker diverticulum. World J Gastrointest Endosc 2015;7(2):87-93. https://doi.org/10.4253/wjge.v7.i2.87 [ Links ]
16. Albers DV, Kondo A, Bernardo WM, Sakai P, Moura RN, Silva GL, Ide E, Tomishige T, de Moura EG. Endoscopic versus surgical approach in the treatment of Zenker’s diverticulum: systematic review and meta-analysis. Endosc Int Open. 2016;4(6):E678-E686. https://doi.org/10.1055/s-0042-106203 [ Links ]
17. Bloom JD, Bleier BS, Mirza N, Chalian AA, Thaler ER. Factors predicting endoscopic exposure of Zenker’s diverticulum. Ann Otol Rhinol Laryngol. 2010;119(11):736-41. https://doi.org/10.1177/000348941011901116 [ Links ]
18. Saetti R, Silvestrini M, Peracchia A, Narne S. Endoscopic stapler-assisted Zenker’s diverticulotomy: which is the best operative facility? Head Neck. 2006;28(12):1084-9. https://doi.org/10.1002/hed.20431 [ Links ]
19. Salassa J. A Functional Outcome Swallowing Scale for Staging Oropharyngeal Dysphagia. Dig Dis. 1999;17(4):230-4. https://doi.org/10.1159/000016941 [ Links ]
20. Bergeron JL, Long JL, Chhetri DK. Dysphagia Characteristics in Zenker’s Diverticulum. Otolaryngol Head Neck Surg. 2013;148(2): 223-228. https://doi.org/10.1177/0194599812465726 [ Links ]
21. Miller FR, Taylor C. Zenker’s Diverticulum: Endoscopic Surgical Management Options. Clin Surg. 2017;2:1422. [ Links ]
22. Ferreira LE, Simmons DT, Baron TH. Zenker’s diverticula: pathophysiology, clinical presentation, and flexible endoscopic management. Dis Esophagus. 2008;21(1):1-8. https://doi.org/10.1111/j.1442-2050.2007.00795.x [ Links ]
23. Bizzotto A, Iacopini F, Landi R, Costamagna G. Zenker’s diverticulum: exploring treatment options. Acta Otorhinolaryngol Ital. 2013;33(4):219-29. [ Links ]
24. Naprawa G, Białkowska J. Foreign body in a Zenker’s diverticulum (looking for the lost dentures). Prz Gastroenterol. 2014;9(4):254-8. https://doi.org/10.5114/pg.2014.45109 [ Links ]
25. Wong HJ, Ujiki MB. Per Oral Zenker Diverticulotomy. Surg Clin North Am. 2020;100(6):1215-1226. https://doi.org/10.1016/j.suc.2020.08.005 [ Links ]
26. Babür, T. Iatrogenic Zenker’s diverticulum perforation: A conservatively treated case. Ulus Cerrahi Derg. 2013;30(4):234-6. https://doi.org/10.5152/UCD.2013.24 [ Links ]
27. Rizzetto C, Zaninotto G, Costantini M, Bottin R, Finotti E, Zanatta L, Guirroli E, Ceolin M, Nicoletti L, Ruol A, Ancona E. Zenker’s diverticula: feasibility of a tailored approach based on diverticulum size. Journal of Gastrointestinal Surgery, 2008;12(12), 2057-2065. https://doi.org/10.1007/s11605-008-0684-7 [ Links ]
28. Sakai P. Endoscopic myotomy of Zenker’s diverticulum: lessons from 3 decades of experience. Gastrointestinal endoscopy. 2016;83(4):774-5. https://doi.org/10.1016/j.gie.2015.10.031 [ Links ]
29. Verdonck J, Morton RP. Systematic review on treatment of Zenker’s diverticulum. Eur Arch Otorhinolaryngol. 2015;272(11):3095-107. https://doi.org/10.1007/s00405-014-3267-0 [ Links ]
30. Battaglia G, Antonello A, Realdon S, Cesarotto M, Zanatta L, Ishaq S. Flexible endoscopic treatment for Zenker’s diverticulum with the SB Knife. Preliminary results from a single-center experience. Dig Endosc. 2015;27(7):728-33. https://doi.org/10.1111/den.12490 [ Links ]
31. Nielsen HU, Trolle W, Rubek N, Homøe P. New technique using LigaSure for endoscopic mucomyotomy of Zenker’s diverticulum: diverticulotomy made easier. Laryngoscope. 2014;124(9):2039-42. https://doi.org/10.1002/lary.24558 [ Links ]
32. Ishaq S, Hassan C, Antonello A, Tanner K, Bellisario C, Battaglia G, Anderloni A, Correale L, Sharma P, Baron TH, Repici A. Flexible endoscopic treatment for Zenker’s diverticulum: a systematic review and meta-analysis. Gastrointest Endosc. 2016;83(6):1076-1089.e5. https://doi.org/10.1016/j.gie.2016.01.039 [ Links ]
33. Wilmsen J, Baumbach R, Stüker D, Weingart V, Neser F, Gölder SK, Pfundstein C, Nötzel EC, Rösch T, Faiss S. New flexible endoscopic controlled stapler technique for the treatment of Zenker’s diverticulum: A case series. World J Gastroenterol. 2017;23(17):3084-3091. https://doi.org/10.3748/wjg.v23.i17.3084 [ Links ]
34. Yuan Y, Zhao YF, Hu Y, Chen LQ. Surgical treatment of Zenker’s diverticulum. Dig Surg. 2013;30(3):207-18. https://doi.org/10.1159/000351433 [ Links ]
35. Fan HS, Stavert B, Chan DL, Talbot ML. Management of Zenker’s diverticulum using flexible endoscopy. VideoGIE. 2019;4(2):87-90. https://doi.org/10.1016/j.vgie.2018.12.007 [ Links ]
36. Pescarus R, Shlomovitz E, Sharata AM, Cassera MA, Reavis KM, Dunst CM, Swanström LL. Trans-oral cricomyotomy using a flexible endoscope: technique and clinical outcomes. Surg Endosc. 2016;30(5):1784-9. https://doi.org/10.1007/s00464-015-4445-x [ Links ]
37. Yang J, Novak S, Ujiki M, Hernández Ó, Desai P, Benias P, Lee D, Chang K, Brieau B, Barret M, Kumta N, Zeng X, Hu B, Delis K, Khashab MA. An international study on the use of peroral endoscopic myotomy in the management of Zenker›s diverticulum. Gastrointest Endosc. 2020;91(1):163-168. https://doi.org/10.1016/j.gie.2019.04.249 [ Links ]
38. Ishaq S, Kuwai T, Siau K, Mulder CJ, Neumann H. Is Z-POEM for Zenker›s the same as POEM for achalasia? Or we are barking up the wrong tree? Gastrointest Endosc. 2020;91(1):204-205. https://doi.org/10.1016/j.gie.2019.07.028 [ Links ]
39. Ko FC. Preoperative Frailty Evaluation: A Promising Risk-stratification Tool in Older Adults Undergoing General Surgery. Clin Ther. 2019;41(3):387-399. https://doi.org/10.1016/j.clinthera.2019.01.014 [ Links ]
40. Shinall MC Jr, Arya S, Youk A, Varley P, Shah R, Massarweh NN, Shireman PK, Johanning JM, Brown AJ, Christie NA, Crist L, Curtin CM, Drolet BC, Dhupar R, Griffin J, Ibinson JW, Johnson JT, Kinney S, LaGrange C, Langerman A, Loyd GE, Mady LJ, Mott MP, Patri M, Siebler JC, Stimson CJ, Thorell WE, Vincent SA, Hall DE. Association of Preoperative Patient Frailty and Operative Stress With Postoperative Mortality. JAMA Surg. 2019;155(1):e194620. https://doi.org/10.1001/jamasurg.2019.4620 [ Links ]
41. Ishioka S, Sakai P, Maluf Filho F, Melo JM. Endoscopic incision of Zenker’s diverticula. Endoscopy. 1995;27(6):433-7. https://doi.org/10.1055/s-2007-1005736 [ Links ]
42. Hashiba K, de Paula AL, da Silva JG, Cappellanes CA, Moribe D, Castillo CF, Brasil HA. Endoscopic treatment of Zenker’s diverticulum. Gastrointest Endosc. 1999;49(1):93-7. https://doi.org/10.1016/s0016-5107(99)70452-9 [ Links ]
43. Sakai P, Ishioka S, Maluf-Filho F, Chaves D, Moura EG. Endoscopic treatment of Zenker’s diverticulum with an oblique-end hood attached to the endoscope. Gastrointest Endosc. 2001;54(6):760-3. https://doi.org/10.1067/mge.2001.119606 [ Links ]
44. de la Morena E, Pérez-Arellano E, Carreño R, Tomás E, González-Lama Y. Tratamiento endoscópico del divertículo de Zenker [Endoscopic treatment of Zenker’s diverticulum]. Cir Esp. 2005;78(4):256-9. [ Links ]
45. Vogelsang A, Preiss C, Neuhaus H, Schumacher B. Endotherapy of Zenker’s diverticulum using the needle-knife technique: long-term follow-up. Endoscopy. 2007;39(2):131-6. https://doi.org/10.1055/s-2006-944657 [ Links ]
46. Costamagna G, Iacopini F, Tringali A, Marchese M, Spada C, Familiari P, Mutignani M, Bella A. Flexible endoscopic Zenker’s diverticulotomy: cap-assisted technique vs. diverticuloscope-assisted technique. Endoscopy. 2007;39(2):146-52. https://doi.org/10.1055/s-2007-966140 [ Links ]
Citation: Gómez MA, Ruíz OF, Marulanda H. Zenker’s diverticulum: endoscopic treatment with or without diverticulotome. Rev Colomb Gastroenterol. 2020;35(4):421-429. https://doi.org/10.22516/25007440.504
Received: February 03, 2020; Accepted: August 24, 2020











 text in
text in