Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em
SciELO
Similares em
SciELO -
 Similares em Google
Similares em Google
Compartilhar
Revista colombiana de Gastroenterología
versão impressa ISSN 0120-9957versão On-line ISSN 2500-7440
Rev. colomb. Gastroenterol. vol.35 no.4 Bogotá out./dez. 2020 Epub 12-Jul-2021
https://doi.org/10.22516/25007440.512
Original article
Endoscopic retrograde cholangiopancreatography at a leading cancer center
1 Clínica de Gastroenterología. Instituto Nacional de Cancerología. Profesor facultad de medicina, Universidad Nacional de Colombia. Bogotá, Colombia
2 Clínica de gastroenterología, Instituto Nacional de Cancerología. Bogotá, Colombia
3 Grupo de Investigación Clínica, Instituto Nacional de Cancerología. Profesor facultad de medicina, Universidad Nacional de Colombia. Bogotá, Colombia
4 Grupo de Investigación Clínica, Instituto Nacional de Cancerología. Bogotá, Colombia
Introduction:
Endoscopy is one of the tools necessary to treat biliary and pancreatic diseases. Endoscopic retrograde cholangiopancreatography (ERCP) is one of the most technically demanding procedures with the highest risk of complications when treating hepato-pancreato-biliary disorders.
Methodology:
Observational, retrospective, descriptive case series study based on clinical data of patients brought to ERCP in a population diagnosed with cancer of different primary origins and in different stages of the disease from January 2010 to January 2017.
Results:
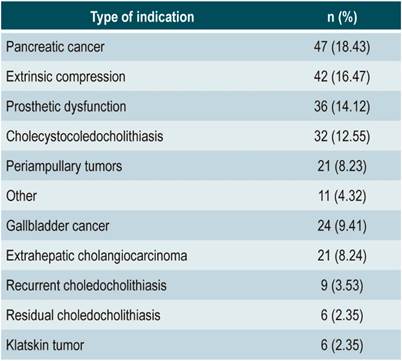
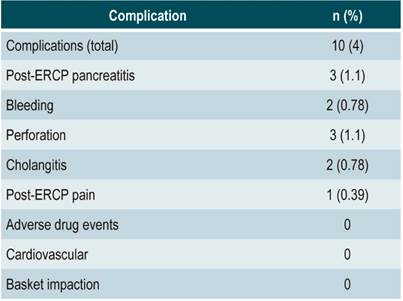
A total of 255 procedures were analyzed. The female sex was predominant with 140 cases (54.9%), and the average age was 62.9 years (SD 12.9 years). All procedures were done with therapeutic intent. The most frequent indication was pancreatic cancer (N=47; 18.43%), extrinsic compression of the common bile duct (N=42; 16.47%), biliary prosthesis dysfunction (N=36; 14.12%), cholecystocholedocholithiasis (N=32; 12. 55%), other causes (N=32; 12.55%), gallbladder cancer (N=24; 9.41%), extrahepatic cholangiocarcinoma (N=21; 8.24%), recurrent choledocholithiasis (N=9; 3.53%), residual choledocholithiasis (N=6; 2.35%), and Klatskin tumor (N=6; 2.35%). Successful cannulation was reported in 222 cases (87.06%). During the procedure, 10 patients presented complications (4.3%), with pancreatitis and perforations being the most frequent (N=3; 1.18%), followed by bleeding, cholangitis (N=2; 0.78%), and post-ERCP pain (N=1; 0.39%).
Conclusions:
In the population studied, the principal reasons for performing the procedure were related to cancer. The frequency of successful cannulation and complications reported here are similar to other results in the general population.
Keywords: Endoscopic cholangiopancreatography; cancer; reference center
Introducción:
la endoscopia es una de las herramientas necesarias para el manejo de las enfermedades biliares y pancreáticas. La colangiopancreatografía retrógrada endoscópica (CPRE) es uno de los procedimientos técnicamente más demandantes y de mayor riesgo de complicaciones realizados en el tratamiento de los desórdenes hepatopancreatobiliares.
Objetivo:
caracterizar los resultados clínicos de los pacientes llevados a CPRE en un centro de pacientes con cáncer exclusivamente.
Métodos:
estudio de serie de casos observacional, retrospectivo, descriptivo con base en datos clínicos de pacientes llevados a CPRE en una población diagnosticada con cáncer de distintos orígenes primarios y en diferentes estadios de enfermedad desde enero de 2010 hasta enero de 2017.
Resultados:
se analizaron 255 procedimientos en los que predominó el sexo femenino con 140 casos (54,9 %), el promedio de edad fue 62,9 años (desviación estándar [DE]: 12,9 años). Todos los procedimientos se hicieron con intención terapéutica. La indicación más frecuente fue cáncer de páncreas (n = 47; 18,43 %), compresión extrínseca de la vía biliar (n = 42; 16,47 %), disfunción de prótesis (n = 36; 14,12%), colecistocoledocolitiasis (n = 32; 12,55 %), otras causas (n = 32; 12,55 %), cáncer de vesícula (n = 24; 9,41 %), colangiocarcinoma extrahepático (n = 21; 8,24 %), coledocolitiasis recidivante (n = 9; 3,53%), coledocolitiasis residual (n = 6; 2,35 %) y tumor de Klatskin (n = 6; 2,35 %). La canalización exitosa se presentó en 222 casos (87,06 %). Durante el procedimiento, 10 pacientes presentaron complicaciones (4,3 %), de las cuales la pancreatitis y las perforaciones fueron las más frecuentes (n = 3; 1,18 %), seguidas por sangrado, colangitis (n = 2; 0,78 %) y dolor post-CPRE 1 (0,39 %).
Conclusiones:
en la población evaluada, la causa predominante para realizar el procedimiento está relacionada con cáncer y la frecuencia tanto de canalización exitosa como de complicaciones es similar a la de los reportes en las poblaciones generales.
Palabras clave: Colangiopancreatografía endoscópica; cáncer; centro de referencia
Introduction
Endoscopic procedures are often used to treat both biliary tract and pancreatic diseases. Since its introduction in 1968, endoscopic retrograde cholangiopancreatography (ERCP) has played an important role in the treatment of both benign and malignant diseases1,7. Although endoscopic cholangiography provided new diagnostic possibilities for diseases of the biliary tree and the pancreas for several years, with the development of non-invasive studies such as magnetic resonance and endoscopic ultrasound, the primary role of ERCP has now shifted to be therapeutic, avoiding purely diagnostic explorations and the possibility of complications resulting from the procedure2.
Neoplasms of the biliary tract and the pancreas, as well as other digestive system tumors and even those originating in other organs, may cause biliary obstruction by both locally advanced involvement and metastatic disease, requiring endoscopic therapeutic procedures to alleviate biliary obstruction and its implications. Similarly, cancer patients are not exempt from presenting complications associated with biliary lithiasis.
Centers that exclusively treat cancer patients usually have highly complex digestive endoscopy services to diagnose and provide preoperative or palliative treatment for the different digestive system tumors that affect the biliary tract3.
ERCP is a specialized endoscopic technique in which bile and pancreatic ducts are approached with the aim of verifying situations requiring management, such as stone extraction, tissue collection, and bile flow restitution, using self-expandable plastic or metal stents. The procedure is performed using image-guided fluoroscopy and sedation or general anesthesia. There are risks of complications associated with any endoscopic procedure, but there are other risks specific to this intervention, such as acute pancreatitis (which is the most common), bleeding, perforation, cholangitis, post-ERCP pain, and biliary basket impaction, among others. Several case series studies report an incidence of complications of up to 10%, and a mortality rate up to 1 %4.
Risk factors for the development of complications associated with the procedure are well described, with proper preparation of the person performing the procedure playing a major role, as well as patient-specific factors and the relationship between these factors, which will determine the occurrence of such events5,6.
The present study was carried out to describe the ERCPs performed in patients with a cancerous disease either in or outside the pancreatic and bile ducts treated at the Instituto Nacional de Cancerología between January 2010 and January 2017 for in order to characterize the outcomes of this intervention.
Materials and methods
Observational, retrospective, descriptive case series study. The information was extracted by reviewing the medical records of patients undergoing ERCP in the gastrointestinal surgery and digestive endoscopy unit of the Instituto Nacional de Cancerología of Bogotá from January 2010 to January 2017. In case the information was not found, the patient was contacted by telephone using the number provided in the medical record.
Procedures were performed by specialists in gastrointestinal surgery, gastroenterology, and digestive endoscopy with an experience of more than 150 cases per year, and, in some cases with the participation of training specialists, using the Olympus TJF-145 video duodenoscope and with patients under general anesthesia. Demographic and clinical characteristics related to the indication of the procedure, as well as the frequency of complications during and after the procedure, were recorded for each patient older than 18 years who underwent the procedure at the Instituto Nacional de Cancerología during the study period and had a follow-up of at least 30 days. Information regarding the measurement of variables was entered into a database designed for this purpose in the ACCESS® software; the database allowed for the management of the variables that were then exported to Stata 12® for the corresponding analysis. This project was approved and monitored by the Research Ethics Committee of the Instituto Nacional de Cancerología.
Statistical analysis
The descriptive method was used in the study for data analysis. Categorical variables were summarized as percentages. In the case of continuous variables, means and standard deviations (SD) or medians and the corresponding interquartile ranges (IQR) were used as a summary measure. Procedure-related death was considered as an outcome; incidence density rates were calculated to explain it, taking into account the different follow-up periods. These ratios were expressed using 1000 patients per month as the denominator and were calculated by taking follow-up losses or the absence of outcome as right censoring; ratios were calculated along with their corresponding 95% confidence intervals (CI).
Results
A total of 255 ERCPs were performed during the study period to treat hepato-pancreato-biliary diseases. The sociodemographic and clinical characteristics of the patients are described in Table 1.
Table 1 Sociodemographic and clinical characteristics of the patients who underwent ERCP.
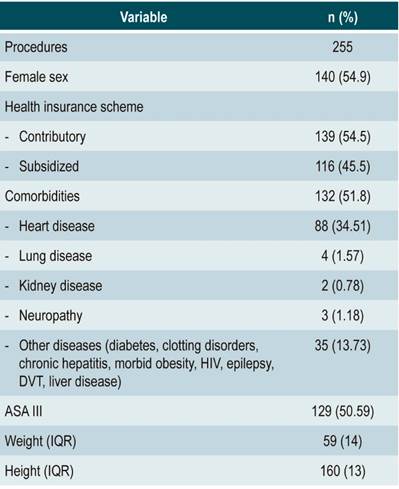
ASA: American Society of Anesthesiologists classification; DVT: deep vein thrombosis; HIV: human immunodeficiency virus.
More interventions were performed in female patients; patients’ mean age was 62.9 years (SD: 12.9 years). Approximately half of the patients had some kind of comorbidity, with heart failure being the most frequent. In 192 patients, the mean body mass index (BMI) was 22 kg/m2. All ERCPs were performed with therapeutic intent.
The most frequent indications for the procedure were pancreatic cancer, extrinsic compression of the bile duct, stent dysfunction, and cholecystocoledocholithiasis (Table 2). The most frequent neoplastic causes of compression of the bile duct were lymphomas, breast and cervical cancer, and testicular seminomas with retroperitoneal involvement. Other causes included periampullary tumors, pancreas divisum, biliary fistula, pancreatic fistula, and cholecodal cysts. Only two procedures were performed in patients with altered gastrointestinal tract anatomy due to a history of subtotal gastrectomy as a result of stomach cancer and reconstruction with loop gastrojejunostomy, which allowed treating the papilla with a conventional duodenoscope through papillotomy on a plastic stent (FleximaTM) of 7 cm x 7 Fr with needle scalpel (MicroKnifeTM), with subsequent extraction of stones (Figure 1).
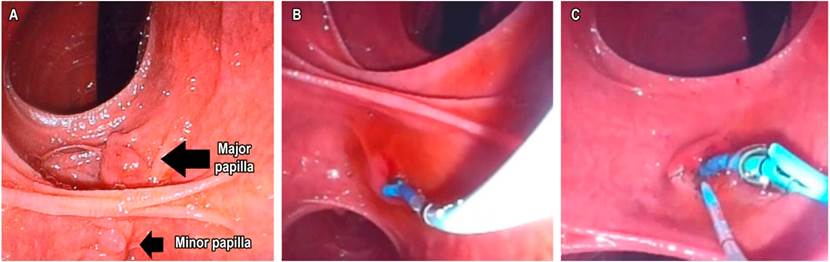
Figure 1 A. Papillary region from a retrograde view. B. Placement of a temporary plastic stent. C. Papillotomy with needle scalpel over the stent.
Most of the interventions (n=190) were performed in inpatients (74.51 %). Precut papillotomy was required during the intervention in only 13 procedures (5.1 %). Concerning stents, plastic stents (n = 127; 49.80 %) were used more frequently compared to and metal stents (n = 13; 5.10 %); only 7 pancreatic stents (2.75 %) were released. Gallstones were removed in 46 (18.04%) procedures, and mechanical lithotripsy was not used in any case, ampullectomy was performed during the procedure in 5 (1.9%) of the patients with periampullary tumors. Successful cannulation was achieved in 222 procedures (87.06 %), and of these, clinical efficacy was reported in 209 (81.96 %). During the procedure, 10 patients experienced complications, being pancreatitis and perforations the most frequent (Table 3).
ERCP-related mortality analysis was carried out based on 240 observations (15 patients were excluded from the analysis because no follow-up information was available). The total follow-up time for the 240 patients was 880.8 months (minimum follow-up time: 0.03 months; maximum follow-up time: 98.5 months). Two ERCP-related deaths were reported during this period, implying a procedure-related mortality rate of 2.3 deaths per 1 000 patients/month (95% CI: 0.57 to 9.1). Median survival time was not calculated due to the low occurrence of deaths.
Discussion
One of the most challenging procedures of digestive endoscopy is therapeutic ERCP with sphincterotomy to remove bile duct stones and place and replace biliary and pancreatic stents. Success depends on the endoscopist’s training, ability and experience, and the success rate ranges between 90 % and 95 % when performed by experts8.
The frequency of comorbidities and the sex distribution observed in our sample are similar to those reported in other studies8-12.
The most common indications for performing ERCP were pancreatic cancer and extrinsic bile duct compression. In contrast to what has been described in the literature, the prevalence of cholecystocoledocholithiasis was only 12.55 %13. All ERCPs were performed with therapeutic intent and successful bile duct cannulation was achieved in 87.06 % of the procedures, with adequate biliary drainage or stone extraction in 81.96 % of cases.
Five ampullectomies were performed in the study population. In patients in which a plastic stent was used, the median time to experience dysfunction was n 3 weeks, and the transition to self-expanding metal stents took 8 weeks. As mentioned above, the most frequent complications were post-ERCP pancreatitis and perforation; however, the first complication was less frequent than the incidence described in the relevant literature, which reaches up to 4 %8,10, and clinical symptoms resolved with medical management. Regarding the second complication, one of the cases was observed in the antrum and resolved immediately with the placement of an OVESCO clip and the subsequent completion of the procedure; while the other two cases, classified as extravasation of the contrast medium after papillotomy was performed and interpreted as bile duct lesions, were managed using a plastic biliary stent without the development of new symptoms. The frequency of this complication and the management reported in the present study are similar to what has been reported in the literature (0.08 % to 1.6 %)14. Bleeding occurred in a smaller number of patients, of which one died; however, the origin of the bleeding was attributed to esophageal varices. One patient presented post-ERCP pain that resolved the next day after ruling out pancreatitis and perforation, but, since this is a retrospective study, the probability of any of these variables being underreported in clinical reports cannot be disregarded15.
None of our patients experienced complications related to medications, cardiovascular events, or implanted devices; these complications are poorly reported in the literature15.
In our experience as a cancer treatment center in Colombia, the endoscopic approach to the bile duct of patients who not only have hepato-pancreato-biliary neoplasms has a success rate that coincides with global experience and the complications rate is similar to what is described in the literature, in studies conducted in centers with a larger number of patients. This is most likely explained by the number of procedures performed by each specialist in other institutions16. The main limitation of the present study is its retrospective nature, as well as the difficulty regarding the patients’ follow-up exclusively due to health insurance reasons, which may also explain the small number of cases even though the institution where the study was conducted is a health center in which only patients with cancer are treated. The fact that most variables are retrieved from medical records is a drawback of retrospective research since it can be a significant source of bias.
Conclusions
In a hospital where only cancer patients are treated, the most frequent reason for performing ERCP is digestive system neoplasms that cause biliary obstruction; similarly, lithiasis is uncommon. The frequency of successful cannulation and complications associated with the procedure are similar to those reported in populations with benign and malignant diseases.
Acknowledgments
To all the administrative and care staff of the Oncology Gastroenterology Service of the Instituto Nacional de Cancerología.
REFERENCES
1. McCune WS, Shorb PE, Moscovitz H. Endoscopic cannulation of the ampulla of vater: a preliminary report. Ann Surg. 1968;167(5):752-6. https://doi.org/10.1097/00000658-196805000-00013 [ Links ]
2. National Institutes of Health. NIH state of the science statement on endoscopic retrograde cholangiopancreatography (ERCP) for diagnosis and therapy. NIH Consens State Sci Statements. 2002;19(1):1-26. [ Links ]
3. Kutty RS, Westaby D, Martin JP, Vlavianos P, Andreyev HJN. What are the Gastrointestinal Endoscopic Requirements of a Cancer Centre? Clin Oncol (R Coll Radiol). 2007;19(5):330-2. https://doi.org/10.1016/j.clon.2007.03.008 [ Links ]
4. Freeman ML. Adverse outcomes of endoscopic retrograde cholangiopancreatography: avoidance and management. Gastrointest Endosc Clin N Am. 2003;13(4):775-98, xi. https://doi.org/10.1016/S1052-5157(03)00107-7 [ Links ]
5. Baillie J. Endoscopic therapy in acute recurrent pancreatitis. World J Gastroenterol. 2008;14(7):1034-7. https://doi.org/10.3748/wjg.14.1034 [ Links ]
6. Donnellan F, Byrne MF. Prevention of Post-ERCP Pancreatitis. Gastroenterol Res Pract. 2012;2012:796751. https://doi.org/10.1155/2012/796751 [ Links ]
7. Kawai K, Akasaka Y, Murakami K, Tada M, Koli Y. Endoscopic sphincterotomy of the ampulla of Vater. Gastrointest Endosc. 1974;20(4):148-51. https://doi.org/10.1016/S0016-5107(74)73914-1 [ Links ]
8. Baillie J. ERCP training: for the few, not for all. Gut. 1999;45(1):9-10. https://doi.org/10.1136/gut.45.1.9 [ Links ]
9. Vandervoort J, Soetikno RM, Tham TC, Wong RC, Ferrari AP Jr, Montes H, Roston AD, Slivka A, Lichtenstein DR, Ruymann FW, Van Dam J, Hughes M, Carr-Locke DL. Risk factors for complications after performance of ERCP. Gastrointest Endosc. 2002;56(5):652-6. https://doi.org/10.1067/mge.2002.129086 [ Links ]
10. ASGE Standards of Practice Committee, Chandrasekhara V, Khashab MA, Muthusamy VR, Acosta RD, Agrawal D, Bruining DH, Eloubeidi MA, Fanelli RD, Faulx AL, Gurudu SR, Kothari S, Lightdale JR, Qumseya BJ, Shaukat A, Wang A, Wani SB, Yang J, DeWitt JM. Adverse events associated with ERCP. Gastrointest Endosc. 2017;85(1):32-47. https://doi.org/10.1016/j.gie.2016.06.051 [ Links ]
11. Kochar B, Akshintala VS, Afghani E, Elmunzer BJ, Kim KJ, Lennon AM, Khashab MA, Kalloo AN, Singh VK. Incidence, severity, and mortality of post-ERCP pancreatitis: a systematic review by using randomized, controlled trials. Gastrointest Endosc. 2015;81(1):143-149.e9. https://doi.org/10.1016/j.gie.2014.06.045 [ Links ]
12. Shanmugarajah I, Solhaug M, Aslam O, Reiertsen O. Efficacy and safety assessment of ERCP in patients with malignant biliary obstruction. Acta Gastroenterol Belg. 2017;80(4):487-91. [ Links ]
13. Cohen ME, Slezak L, Wells CK, Andersen DK, Topazian M. Prediction of bile duct stones and complications in gallstone pancreatitis using early laboratory trends. Am J Gastroenterol. 2001;96(12):3305-11. https://doi.org/10.1111/j.1572-0241.2001.05330.x [ Links ]
14. Stapfer M, Selby RR, Stain SC, Katkhouda N, Parekh D, Jabbour N, Garry D. Management of duodenal perforation after endoscopic retrograde cholangiopancreatography and sphincterotomy. Ann Surg. 2000;232(2):191-8. https://doi.org/10.1097/00000658-200008000-00007 [ Links ]
15. Penaloza-Ramirez A, Leal-Buitrago C, Rodriguez-Hernandez A. Adverse events of ERCP at San Jose Hospital of Bogota (Colombia). Rev Esp Enferm Dig. 2009;101(12):837-49. https://doi.org/10.4321/S1130-01082009001200003 [ Links ]
16. Peng C, Nietert PJ, Cotton PB, Lackland DT, Romagnuolo J. Predicting native papilla biliary cannulation success using a multinational Endoscopic Retrograde Cholangiopancreatography (ERCP) Quality Network. BMC Gastroenterol. 2013;13:147. https://doi.org/10.1186/1471-230X-13-147 [ Links ]
Citation: Pinilla-Morales R, Jaime Montoya-Botero J, Ricardo Oliveros-Wilches R, María Eugenia Manrique-Acevedo ME, Mario Rey-Ferro M, Mario Abadía-Díaz M, Ricardo Sánchez-Pedraza R, Garrido-Bohórquez AJ. Endoscopic retrograde cholangiopancreatography at a leading cancer center. Rev Colomb Gastroenterol. 2020;35(4):430-435. https://doi.org/10.22516/25007440.512
Received: February 12, 2020; Accepted: September 30, 2020











 texto em
texto em