Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista colombiana de Gastroenterología
Print version ISSN 0120-9957On-line version ISSN 2500-7440
Rev. colomb. Gastroenterol. vol.35 no.4 Bogotá Oct./Dec. 2020 Epub July 12, 2021
https://doi.org/10.22516/25007440.517
Original article
Presentation and outcome of conservative management of intestinal obstruction caused by adhesions in Cauca
1Cirujano General, Fellow de Cirugía Pediátrica, Universidad del Valle. Cali, Colombia.
2Médica docente, Especialista en Salud Familiar, Universidad del Cauca. Popayán, Colombia.
3Médica, Magíster en Salud Ocupacional, Clínica La Estancia. Popayán, Colombia.
4Médico, Hospital Susana López de Valencia, Popayán, Colombia.
5Médica docente, Magíster en Epidemiología Clínica, Universidad del Cauca. Popayán, Colombia.
Introduction:
Intestinal obstruction by adhesions accounts for 25% of consultations to the emergency department associated with acute abdominal pain, generating a high risk of iatrogenic injury by emergency reinterventions. An alternative to determine the need for surgical treatment is providing conservative medical management first and then assessing patients’ response within 12-72 hours.
Objective:
To describe the clinical outcomes of adult patients with bowel obstruction caused by adhesions treated at a tertiary care hospital who received non-surgical medical treatment on admission.
Methodology:
Observational, prospective cohort study on patients treated conservatively during the period 2012-2013 for intestinal obstruction. Socio-demographic and clinical information was collected from patients, and follow-up was done until discharge. The analysis was carried out using descriptive statistics in SPSS v15.
Results:
58.9% of the cases occurred in men, and the average age was 55.2 years. 57.1% of the patients had comorbidities predominantly associated with cardiovascular diseases, and 91.1% had previously undergone a surgical procedure, half of them due to inflammatory processes. The most common symptoms were emesis and abdominal distention. The response to conservative treatment was 80.4% of the 19.6% that required surgical management. In 81.8% of the cases, intestinal obstruction caused by adhesions was the main intraoperative finding. The average time of hospitalization was 5.5 days, and during the study only one patient died.
Conclusion:
Conservative medical management should be considered as the initial treatment for this entity due to its high response rate, reduction of postoperative complications, and shorter hospital stay.
Keywords: Intestinal obstruction; Peritoneum; Gastrointestinal motility; Signs and symptoms
Introducción:
la obstrucción intestinal por bridas es responsable del 25 % de las consultas a urgencias por dolor abdominal agudo, generando un alto riesgo de lesión iatrogénica por reintervenciones de urgencia. Una alternativa para determinar la necesidad de manejo quirúrgico sería el manejo médico conservador inicial y evaluar su respuesta en un período de 12-72 horas.
Objetivo:
describir los desenlaces clínicos de los pacientes adultos con obstrucción intestinal por bridas en un hospital de tercer nivel y que recibieron manejo médico no quirúrgico al ingreso.
Metodología:
estudio observacional tipo cohorte, prospectivo, de los pacientes atendidos con tratamiento conservador durante el período 2012-2013 por obstrucción intestinal. Se recogió información sociodemográfica y clínica de los pacientes, así como seguimiento hasta el alta hospitalaria. Para el análisis se empleó estadística descriptiva y se analizó con SPSS V.15.
Resultados:
el 58,9 % de los casos eran masculinos con edad media de 55,2 años, el 57,1 % tenía comorbilidades en las que predominaron las enfermedades cardiovasculares y 91,1 % tenía antecedentes quirúrgicos, la mitad de ellos por procesos inflamatorios. Los principales síntomas fueron emesis y distención abdominal. La respuesta al tratamiento conservador fue de 80,4 %; del 19,6 % que requirió manejo quirúrgico, en el 81,8 % de los casos el hallazgo intraoperatorio fue de obstrucción intestinal por bridas. El tiempo medio de hospitalización fue de 5,5 días y durante el estudio solo un paciente falleció.
Conclusión:
el manejo médico conservador debe ser considerado como el tratamiento inicial de esta entidad por su alta tasa de respuesta, disminución de complicaciones posoperatorias y estancia hospitalaria.
Palabras clave: Obstrucción intestinal; peritoneo; motilidad gastrointestinal; signos y síntomas
Introduction
Peritoneal adhesions are scar tissue that form between abdominal organs, the mesentery, and the abdominal wall as a result of trauma1, generally due to surgical procedures2-6. This condition accounts for 60%-70% of bowel obstruction cases2,6,7, which is defined as a mechanical obstruction that prevents the transit or progression of intestinal contents8-10.
Although it has been extensively studied in gynecologic patients11, in whom it is a risk factor for infertility12-16, the factors that determine how this disease occurs remain unclear. The surgical technique, the area to be operated on and the number of previous surgical procedures have been suggested as associated factors5,17-20; however, no direct relationship has been found with the origin of peritoneal adhesions6.
Intestinal obstruction by adhesions (IOA) accounts for 25% of consultations to the emergency department associated with acute abdominal pain21, generating a high risk of iatrogenic injury by emergency reinterventions. Therefore, a conservative medical approach should be considered first, and the response to this management should be assessed within 72 hours in order to determine if surgery is needed24.
Since there are no data on the prevalence of IOA in Colombia, specifically in Cauca, the aim of this article is to describe the presentation and clinical outcomes of adult patients with this diagnosis treated at the Hospital Universitario San José (HUSJ) and who received non-surgical medical care on admission between 2012 and 2013.
Materials and methods
Descriptive, prospective cohort study that included patients with IOA who were admitted to HUSJ in Popayán, Colombia, and received medical treatment between October 2012 and September 2013.
The following inclusion criteria were considered: admission to the emergency department with symptoms suggestive of IOA, being a candidate for medical care for obstructive disease and signing an informed consent form to participate in the study. On the other hand, patients who were referred to another health care institution or who expressed their will to withdraw from the study during follow-up were excluded.
All patients who were treated at the hospital during the data collection period were recruited using non-probabilistic convenience sampling was used to select. Sociodemographic and clinical information related to the bowel obstruction and its response to treatment (surgical history, signs and symptoms, duration of the symptoms, response to medical treatment, need for surgery, and complications) was collected for all patients. Their medical records were reviewed and their clinical response to treatment was monitored at 12, 24 and 48 hours until discharge.
Descriptive statistics were used to analyze the variables, measures of central tendency and dispersion, and frequencies and proportions were calculated for quantitative and categorical variables, respectively. The chi-square test (χ2) was used to compare outcomes between patients who responded to conservative treatment and those who were ultimately taken to surgery. Data were recorded and processed in the statistical software SPSS V.15. This work was approved by the Ethics Committee HUSJ and followed the ethical principles for conducting biomedical research involving human subjects set forth in the Declaration of Helsinki and in Resolution No. 008430 of 1993 issued by the Ministry of Health of Colombia.
Results
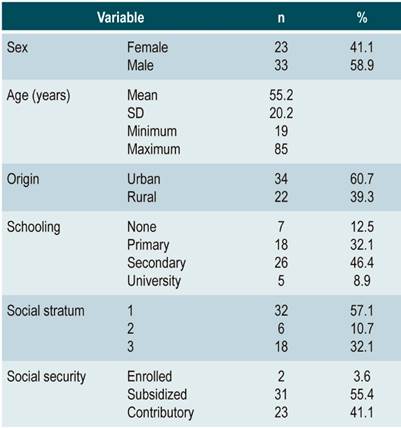
During the study period, 78 patients with a diagnosis of IOA were admitted to HUSJ, of which 15 were referred to other institutions and 7 declined to participate in the study, thus obtaining a final sample of 56 patients. Of the population included (n = 56), 58.9 % (n = 33) were males, and the mean age was 55.2 years (range: 19-85; standard deviation [SD]: 20.2). Regarding their origin, 60.7 % (n = 34) resided in urban areas; 46.4 % had finished high school (n = 26), 57.1 % (n = 32) were from low socio-economic households, and 55.4 % (n = 31) were enrolled in the subsidized health insurance scheme. The sociodemographic characteristics of the patients included in the study are described in Table 1.
Table 1 Sociodemographic characteristics of patients diagnosed with intestinal obstruction treated at HUSJ (2012-2013)
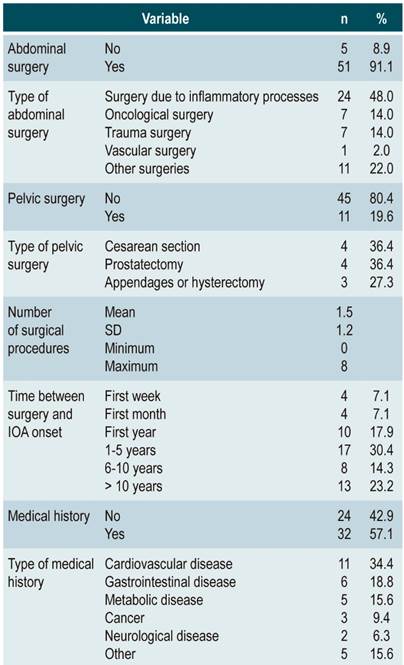
With respect to surgical history, it was found that 91.1 % (n = 51) had undergone abdominal surgery, of which 48 % (n = 24) were due to inflammatory processes. 19.6% (n = 11) had a history of pelvic surgery, including cesarean sections, prostatectomy, and appendages/hysterectomy. The mean number of surgical procedures was 1 surgery (range: 0-8; SD: 1.2) and the time span of this surgical history was 1 to 5 years in 30.4 % (n = 17), with a wide range from the first week to more than 10 years.
57.1 % (n = 32) of the patients had a history of disease, with cardiovascular diseases accounting for 34.4 % (n = 11) of them. Participants’ medical and surgical history is described in Table 2.
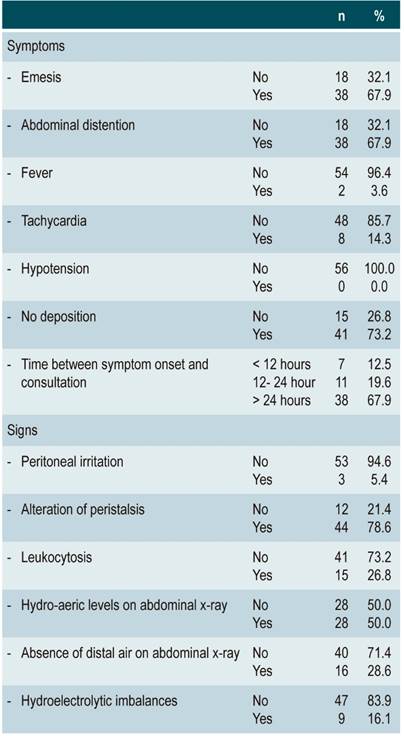
Intestinal obstruction was characterized by symptoms that included no deposition in 73.2 % (n = 41) and emesis and abdominal distension in 67.9 % (n = 38); the mean number of reported symptoms was 2 (range: 0-4; SD: 0.9). Physical examination revealed that 78.6 % (n = 44) of patients had peristalsis, while radiological signs showed that 50 % (n = 28) had hydro-aeric levels and 28.6 % (n = 16) had an absence of distal intestinal air. Laboratory tests reported leukocytosis in 26.8 % (n = 15) and hypokalemia in 16.1 % (n = 9). The period between symptom onset and consultation at the emergency department was greater than 24 hours in 67.9% (n = 38) of cases. Patients’ clinical characteristics are summarized in Table 3.
Table 3 Clinical characteristics of patients diagnosed with intestinal obstruction at HUSJ (2012-2013)
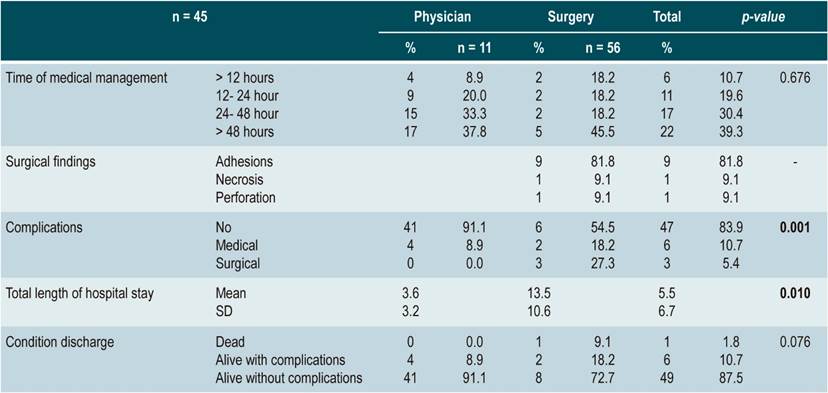
All patients received medical treatment, 39.3 % (n = 22) during a period exceeding 48 hours, and 80.4 % (n = 45) responded to such treatment. In the case of patients who required subsequent surgical management (n = 11), the procedure revealed adhesions in 81.8 % (n = 9), necrosis in 9.1 % (n = 1) and perforations in 9.1 % (n = 1). When outcomes were analyzed according to the type of treatment, it was found that the mean length of hospitalization was much longer in patients undergoing surgery (13.5 vs. 3.6 days); also, one patient in this group died, and there was a higher percentage of complications at discharge, mostly surgical, and this difference was statistically significant (p = 0.001 and p = 0.010, respectively). No association was found between the time elapsed since symptom onset and consultation or between observation time and the occurrence of complications (p = 0.528 and p = 0.410, respectively). The procedures performed and the outcomes are described in Table 4.
Discussion
The aim of this study was to describe the cases of IOA treated in our health care center between 2012 and 2013 and to quantify their clinical response to conservative medical management and its outcomes based on the Bologna guidelines for diagnosis and management of adhesive small bowel obstruction (ASBO)24. It was found that more than half of the cases occurred in males with a mean age of 55 years, which is similar to what has been reported in different studies conducted in the United States, Honduras, and Chile25-30, but differs from findings described in other countries in America and in Spain, where women are predominant, and their mean age was 60 years31-34. This difference can be explained by the demographic characteristics of each territory.
The most common cause of postoperative peritoneal adhesions is previous surgery35, plus the number and type of procedures. More than 90% of the patients included in our study had undergone an abdominal surgery, mainly due to inflammatory processes. These findings are consistent with what those reported in the thesis by Lopez conducted in a case series of 49 patients in Peru28 and other works28,32,36, but differ from what has been reported in Central America, where IOA occurred after undergoing 2 surgeries and the main cause (about 80%) was trauma laparotomy26,33.
In 30% of patients, the surgical procedures were performed 1 to 5 years before the onset of IOA, and one-fifth of participants had undergone the surgery more than 10 years before. Findings regarding this outcome are very diverse, with an average period between the time procedures are performed and IOA onset of 8 years in Central America33. However, in the United Kingdom, there is evidence of earlier occurrence of adhesions, with IOA being developed within 4 weeks in 21% of patients with a history of abdominal surgery37. These differences can be attributed to the etiology of initial symptoms, the type of previous surgery, or the surgeon’s expertise. However, the onset of this condition is difficult to predict, and it is thought that some patients have a stronger tendency to form adhesions than others, despite having undergone the same procedure. This may be due to the particular predisposition of each patient to fibrinolytic activity during adhesion pathogenesis and other factors35.
More than half of the patients included in this study had a history of disease, mainly associated with cardiovascular diseases, followed by gastrointestinal and metabolic disorders. These findings are inferior to those reported in Spain and the United States, where metabolic disorders were more frequent31,38, possibly due to lifestyle factors.
Regarding clinical presentation, predominant symptoms in our study population the absence of bowel movements and emesis, and their frequency is contrary to that reported in Honduras26. Other studies also describe a higher frequency of emesis (80 %), followed by abdominal distention25,28,32,39.
Concerning laboratory parameters, leukocytosis and hypokalemia were reported in almost 30 % and more than 15 % patients, proportions that exceed the findings reported by other authors26,31,34. Specific numbers of leukocytosis or band neutrophils cannot be informed because they varied greatly between patients, even among those who needed intestinal resection. However, high baseline leukocyte counts above 15 000 were the main marker for surgical treatment, as recommended by the ASBO guidelines24,40. Leukocytosis or leukopenia are defined as indicators of severity in intestinal obstruction, but this data was not comparable, possibly due to the short observation period of patients31. Moran reported a similar situation, stating that while the white blood cell count in patients with uncomplicated IOA might be normal or slightly elevated, high (more than 15 000 white blood cells) or very low (less than 4000) counts are suspicious and should alert physicians about the possibility of intestinal ischemia41.
The basic and diagnostic imaging test performed in all cases of intestinal obstruction included in our study was an abdominal x-ray, which revealed hydro-aeric levels in 50 % of patients and the absence of distal air in 28.6 %. This differs from other studies30,32,34 that report computed tomography (CT) was the imaging test most frequently used for determining the cause, detecting signs of complications, and defining treatment. In principle, non-contrast x-ray is the first-line diagnostic test method due to its low cost and high availability24,40; nevertheless, CT is the gold standard because of its high sensitivity and specificity (90%-96%)39,42.
Vital signs play an important role in both diagnostic and prognostic evaluation. In our study, only a few patients had tachycardia (14.3%) and fever (3.6%), proportions that are lower than those reported in studies conducted in Central and North America, where tachycardia has been found in 40% of patients26,34. These symptoms are not often reported in the relevant literature since most studies use these parameters as exclusion criteria because they suggest bowel strangulation or perforation, which require immediate surgical treatment. In Asia, simple obstruction is defined as only the presence of adhesions, while complicated obstruction involves gangrene or strangulation. In patients with complicated obstruction, fever, and leukocytosis (more than 15 000/mm) were observed in 18 (67 %) and 20 (74 %) cases, respectively. These results were not seen in any patient with simple obstruction43.
In the present study, the time elapsed between symptom onset and emergency department consultation exceeded 24 hours in two-thirds of patients, which is consistent with other studies reporting 2-3 days of symptom progression26. Our patients’ response to conservative treatment was effective in 80 % of cases, and out of these, 90 % were discharged without complications. These figures are higher than those described for other populations, where this outcome rate ranged between 20% and 60%27,29,31,32,34,36,43,44. These figures could be related to the type of surgery that caused IOA, in which inflammatory processes predominated, implying less invasive procedures and less abdominal cavity manipulation.
Intestinal obstruction accounts for 30%-41% of all cases requiring additional surgery7, which is more than double of the frequency observed in this study (< 20%). Adhesions are the most common surgical finding (44), which is consistent with what was found in our study population (> 80%), however this proportion exceeds those reported in other studies. (< 50%)27,29,31,32,34,44. The average length of hospital stay of patients treated conservatively was 3 days, yet in patients who were treated with surgery, hospital stay length was four times higher, being this difference statistically significant (p = 0.010). This hospitalization time is consistent with the findings of other authors who report that patients undergoing surgery to treat IOA spend on average 10 days in the hospital32-34,40,45. This may be due to the high prevalence of complications (> 40%) described in this population, which was also significant (p = 0.010). In general, the mortality rate of IOA is 2% in both our population and several studies, occurring only in patients undergoing surgery32,44.
One of the limitations of the present study was that in the healthcare center where it was conducted, CT scans to establish the diagnosis with more reliability were not available. However, available resources at the context and period of time in which this work was carried out should be considered, as well as the fact that prioritization of this type of imaging study was suggested in the 2017 ASBO guidelines42. Similarly, the 1-year data collection period restricted the number of patients to establish statistical significance and no post-discharge follow-up was done to determine recurrence or mortality. On the other hand, its strengths include the fact that this is the first study of its kind to be performed in southwestern Colombia, that it follows international clinical practice guidelines, and that it obtained positive outcomes that exceeded world reports for this event.
In conclusion, it can be said that postoperative IOA mostly affects males and that for its diagnosis, surgical history, symptoms, lab tests results and radiological imaging findings must be taken into account. Initial treatment of this condition should be conservative medical management. This translates into a higher response rate, less postoperative complications, and shorter hospital stay times.
REFERENCES
1. Duron JJ. Postoperative intraperitoneal adhesion pathophysiology. Colorectal Dis. 2007;9(s2):14-24. https://doi.org/10.1111/j.1463-1318.2007.01343.x [ Links ]
2. Ellis H. The magnitude of adhesion related problems. Ann Chir Gynaecol. 1998;87(1):9-11. [ Links ]
3. Al-Jaroudi D, Tulandi T. Adhesion prevention in gynecologic surgery. Obstet Gynecol Surv. 2004;59(5):360-7. https://doi.org/10.1097/00006254-200405000-00024 [ Links ]
4. Ozel H, Avsar FM, Topaloglu S, Sahin M. Induction and assessment methods used in experimental adhesion studies. Wound Repair Regen. 2005;13(4):358-64. https://doi.org/10.1111/j.1067-1927.2005.130402.x [ Links ]
5. Boland GM, Weigel RJ. Formation and prevention of postoperative abdominal adhesions. J Surg Res. 2006;132(1):3-12. https://doi.org/10.1016/j.jss.2005.12.002 [ Links ]
6. Ouaïssi M, Gaujoux S, Veyrie N, Denève E, Brigand C, Castel B, Duron JJ, Rault A, Slim K, Nocca D. Post-operative adhesions after digestive surgery: their incidence and prevention: review of the literature. J Visc Surg. 2012;149(2):e104-14. https://doi.org/10.1016/j.jviscsurg.2011.11.006 [ Links ]
7. Parker MC, Ellis H, Moran BJ, Thompson JN, Wilson MS, Menzies D, McGuire A, Lower AM, Hawthorn RJ, O’Briena F, Buchan S, Crowe AM. Postoperative adhesions: ten-year follow-up of 12,584 patients undergoing lower abdominal surgery. Colon Rectum. 2001;44(6):822-9. https://doi.org/10.1007/BF02234701 [ Links ]
8. Sykes PA, Schofield PF. Early postoperative small bowel obstruction. Br J Surg. 1974;61(8):594-600. https://doi.org/10.1002/bjs.1800610803 [ Links ]
9. Köveker GB, Coerper S, Gottwald T, Flesch I, Becker H-D. The role of wound healing in the formation of peritoneal adhesions. En: Treutner KH, Schumpelick V (editores). Peritoneal adhesions. Springer; 1997. p. 23-8. https://doi.org/10.1007/978-3-642-60433-1_3 [ Links ]
10. Ansari P. Intestinal Obstruction - Gastrointestinal Disorders [Internet]. Merck Manuals Professional Edition. 2020 [citado 13 de diciembre de 2020]. Disponible en: Disponible en: https://www.merckmanuals.com/professional/gastrointestinal-disorders/acute-abdomen-and-surgical-gastroenterology/intestinal-obstruction [ Links ]
11. Schnüriger B, Barmparas G, Branco BC, Lustenberger T, Inaba K, Demetriades D. Prevention of postoperative peritoneal adhesions: a review of the literature. Am J Surg. 2011;201(1):111-21. https://doi.org/10.1016/j.amjsurg.2010.02.008 [ Links ]
12. Tulandi T, Collins JA, Burrows E, Jarrell JF, McInnes RA, Wrixon W, Simpson CW. Treatment-dependent and treatment-independent pregnancy among women with periadnexal adhesions. Am J Obstet Gynecol. 1990;162(2):354-7. https://doi.org/10.1016/0002-9378(90)90384-J [ Links ]
13. Marana R, Rizzi M, Muzii L, Catalano GF, Caruana P, Mancuso S. Correlation between the American Fertility Society classifications of adnexal adhesions and distal tubal occlusion, salpingoscopy, and reproductive outcome in tubal surgery. Fertil Steril. 1995;64(5):924-9. https://doi.org/10.1016/S0015-0282(16)57903-5 [ Links ]
14. Marana R, Catalano GF, Muzii L, Caruana P, Margutti F, Mancuso S. The prognostic role of salpingoscopy in laparoscopic tubal surgery. Hum Reprod. 1999;14(12):2991-5. https://doi.org/10.1093/humrep/14.12.2991 [ Links ]
15. Milingos S, Kallipolitis G, Loutradis D, Liapi A, Mavrommatis K, Drakakis P, Tourikis J, Creatsas G, Michalas S. Adhesions: laparoscopic surgery versus laparotomy. Ann N Acad Sci. 2000;900(1):272-85. https://doi.org/10.1111/j.1749-6632.2000.tb06239.x [ Links ]
16. Vrijland W, Jeekel J, Van Geldorp H, Swank D, Bonjer H. Abdominal adhesions: intestinal obstruction, pain, and infertility. Surg Endosc. 2003;17(7):1017-22. https://doi.org/10.1007/s00464-002-9208-9 [ Links ]
17. Luijendijk RW, de Lange DC, Wauters CC, Hop WC, Duron JJ, Pailler JL, Camprodon BR, Holmdahl L, van Geldorp HJ, Jeekel J. Foreign material in postoperative adhesions. Ann Surg. 1996;223(3):242-8. https://doi.org/10.1097/00000658-199603000-00003 [ Links ]
18. Parker MC, Wilson MS, Menzies D, Sunderland G, Clark DN, Knight AD, Crowe AM; Surgical and Clinical Adhesions Research (SCAR) Group. The SCAR‐3 study: 5‐year adhesion‐related readmission risk following lower abdominal surgical procedures. Colorectal Dis. 2005;7(6):551-8. https://doi.org/10.1111/j.1463-1318.2005.00857.x [ Links ]
19. Nunobe S, Hiki N, Fukunaga T, Tokunaga M, Ohyama S, Seto Y, Yamaguchi T. Previous laparotomy is not a contraindication to laparoscopy-assisted gastrectomy for early gastric cancer. World J Surg. 2008;32(7):1466-72. https://doi.org/10.1007/s00268-008-9542-8 [ Links ]
20. Ward BC, Panitch A. Abdominal adhesions: current and novel therapies. J Surg Res. 2011;165(1):91-111. https://doi.org/10.1016/j.jss.2009.09.015 [ Links ]
21. Glancy DG. Intestinal obstruction. Surg Oxf. 2014;32(4):204-11. https://doi.org/10.1016/j.mpsur.2014.01.004 [ Links ]
22. Coleman MG, McLain AD, Moran MB. Impact of previous surgery on time taken for incision and division of adhesions during laparotomy. Colon Rectum. 2000;43(9):1297-9. https://doi.org/10.1007/BF02237441 [ Links ]
23. Van Der Krabben AA, Dijkstra FR, Nieuwenhuijzen M, Reijnen M, Schaapveld M, Van Goor H. Morbidity and mortality of inadvertent enterotomy during adhesiotomy. Br J Surg. 2000;87(4):467-71. https://doi.org/10.1046/j.1365-2168.2000.01394.x [ Links ]
24. Catena F, Di Saverio S, Kelly MD, Biffl WL, Ansaloni L, Mandalà V, Velmahos GC, Sartelli M, Tugnoli G, Lupo M, Mandalà S, Pinna AD, Sugarbaker PH, Van Goor H, Moore EE, Jeekel J. Bologna Guidelines for Diagnosis and Management of Adhesive Small Bowel Obstruction (ASBO): 2010 Evidence-Based Guidelines of the World Society of Emergency Surgery. World J Emerg Surg. 2011 Jan 21;6:5. https://doi.org/10.1186/1749-7922-6-5 [ Links ]
25. Luque García MJ. Factores pronósticos relacionados con la cirugía de la oclusión intestinal [Internet]. Madrid: Universidad Complutense de Madrid; 2014 [citado el 14 de enero de 2019]. Disponible en: Disponible en: https://eprints.ucm.es/33035/1/T36359.pdf [ Links ]
26. Canales Peña RC, Cortés Cardona CM, Cabrera Interiano H. Obstrucción Intestinal por Bridas/Adherencias: Proporción y Evolución del Manejo Conservador. Arch Med. 2017;13(3):1-6. [ Links ]
27. Quezada S Nicolás, León F Felipe, Llera K Juan de la, Funke H Ricardo, Gabrielli N Mauricio, Crovari E Fernando et al. Tratamiento laparoscópico de la obstrucción intestinal por bridas. Rev Chil Cir [Internet]. 2014 Sep [citado 2020 Dic 13] ; 66( 5 ): 437-442. Disponible en: Disponible en: https://scielo.conicyt.cl/scielo.php?script=sci_arttext&pid=S0718-40262014000500007&lng=es . Disponible en: https://scielo.conicyt.cl/scielo.php?script=sci_arttext&pid=S0718-40262014000500007&lng=es. http://dx.doi.org/10.4067/S0718-40262014000500007 . [ Links ]
28. López Lorenzo RE. Características clínico epidemiológicas de pacientes intervenidos por obstrucción intestinal por bridas y adherencias en el hospital regional docente clínico quirúrgico Daniel Alcides Carrión Huancayo, durante el año 2016 [Internet]. Perú: Universidad Nacional del Centro del Perú; 2017 [citado el 14 de enero de 2019]. Disponible en: Disponible en: http://repositorio.uncp.edu.pe/bitstream/handle/uncp/1548/caracter%c3%8dsticas%20cl%c3%8dnico%20epidemiol%c3%93gicas%20de%20pacientes%20intervenidos%20por%20obstrucci%c3%93n%20intestinal%20por%20.pdf?sequence=1&isAllowed=y [ Links ]
29. García Rengifo REO. Obstrucción intestinal asociada a cirugía de urgencia en el adulto mayor, Hospital II-2 Tarapoto 2015-2016. [Internet]. Perú: Universidad Nacional de San Martín-Tarapoto; 2018 [citado el 14 de enero de 2019]. Disponible en: Disponible en: http://repositorio.unsm.edu.pe/handle/11458/2611 [ Links ]
30. Weaver JL, Barnett RE, Patterson DE, Ramjee VG, Riedinger E, Younga J, Sepulveda EA, Keskey RC, Cheadle WG. Large-bowel disease presenting as small-bowel obstruction is associated with a poor prognosis. Am J Emerg Med. 2016;34(3):477-9. https://doi.org/10.1016/j.ajem.2015.12.008 [ Links ]
31. Enríquez Sánchez S. Análisis de la obstrucción intestinal en pacientes mayores de 50 años [Internet]. Granada: Universidad de Granada; 2007[citado el 14 de enero de 2019]. Disponible en: Disponible en: http://digibug.ugr.es/bitstream/handle/10481/1725/17243750.pdf;jsessionid=876792E294C9233B7366CF4F5BBC8D71?sequence=1 [ Links ]
32. Csendes A, Pereira P, Zamorano M, Arratia I, Gonzalez J, Carriel F. Tratamiento médico o quirúrgico de la obstrucción intestinal alta. Rev Chil Cir. 2016;68(3):227-32. https://doi.org/10.1016/j.rchic.2014.08.001 [ Links ]
33. Garibay-González F, Navarrete-Arellano M, Moreno-Delgado F, Salinas-Hernández EL, Rodríguez-Ayala E, Cleva-Villanueva G. Incidencia de la obstrucción intestinal por adherencias postoperatorias en el Hospital Central Militar. Factores de riesgo asociados. Rev Sanid Milit Mex. 2017;71(6):534-44. [ Links ]
34. Zielinski MD, Eiken PW, Bannon MP, Heller SF, Lohse CM, Huebner M, Sarr MG. Small bowel obstruction-who needs an operation? A multivariate prediction model. World J Surg. 2010;34(5):910-9. https://doi.org/10.1007/s00268-010-0479-3 [ Links ]
35. Correa-Rovelo JM, Villanueva-López GC, Medina-Santillan R, Carrillo-Esper R, Díaz-Girón-Gidi A. Obstrucción intestinal secundaria a formación de adherencias postoperatorias en cirugía abdominal. Revisión de la literatura. Cir Cir. 2015;83(4):345-51. https://doi.org/10.1016/j.circir.2015.05.024 [ Links ]
36. Millet I, Ruyer A, Alili C, Curros Doyon F, Molinari N, Pages E, Zins M, Taourel P. Adhesive small-bowel obstruction: value of CT in identifying findings associated with the effectiveness of nonsurgical treatment. Radiology. 2014;273(2):425-32. https://doi.org/10.1148/radiol.14132872 [ Links ]
37. Menzies D, Ellis H. Intestinal obstruction from adhesions--how big is the problem? Ann R Coll Surg Engl. 1990;72(1):60-3. [ Links ]
38. Mavros MN, Velmahos GC, Lee J, Larentzakis A, Kaafarani HM. Morbidity related to concomitant adhesions in abdominal surgery. J Surg Res. 2014;192(2):286-92. https://doi.org/10.1016/j.jss.2014.07.044 [ Links ]
39. Rosero Vallejos YL. Factores predictores en tomografía computarizada de necesidad de cirugía en pacientes con obstrucción del intestino delgado: Estudio de cohorte (mayo de 2016 hasta mayo de 2018) [Internet]. Bogotá: Universidad Nacional de Colombia; 2018 [citado el 14 de enero de 2019]. Disponible en: Disponible en: https://repositorio.unal.edu.co/bitstream/handle/unal/68650/53009551.2018.pdf?sequence=1&isAllowed=y [ Links ]
40. Di Saverio S, Coccolini F, Galati M, Smerieri N, Biffl WL, Ansaloni L, Tugnoli G, Velmahos GC, Sartelli M, Bendinelli C, Fraga GP, Kelly MD, Moore FA, Mandalà V, Mandalà S, Masetti M, Jovine E, Pinna AD, Peitzman AB, Leppaniemi A, Sugarbaker PH, Goor HV, Moore EE, Jeekel J, Catena F. Bologna guidelines for diagnosis and management of adhesive small bowel obstruction (ASBO): 2013 update of the evidence-based guidelines from the world society of emergency surgery ASBO working group. World J Emerg Surg. 2013;8(1):42. https://doi.org/10.1186/1749-7922-8-42 [ Links ]
41. Moran BJ. Adhesion‐related small bowel obstruction. Colorectal Dis. 2007;9(2):39-44. https://doi.org/10.1111/j.1463-1318.2007.01347.x [ Links ]
42. Ten Broek RPG, Krielen P, Di Saverio S, Coccolini F, Biffl WL, Ansaloni L, Velmahos GC, Sartelli M, Fraga GP, Kelly MD, Moore FA, Peitzman AB, Leppaniemi A, Moore EE, Jeekel J, Kluger Y, Sugrue M, Balogh ZJ, Bendinelli C, Civil I, Coimbra R, De Moya M, Ferrada P, Inaba K, Ivatury R, Latifi R, Kashuk JL, Kirkpatrick AW, Maier R, Rizoli S, Sakakushev B, Scalea T, Søreide K, Weber D, Wani I, Abu-Zidan FM, De’Angelis N, Piscioneri F, Galante JM, Catena F, van Goor H. Bologna guidelines for diagnosis and management of adhesive small bowel obstruction (ASBO): 2017 update of the evidence-based guidelines from the world society of emergency surgery ASBO working group. World J Emerg Surg. 2018;13:24. https://doi.org/10.1186/s13017-018-0185-2 [ Links ]
43. Shih S-C, Jeng K-S, Lin S-C, Kao C-R, Chou S-Y, Wang H-Y, Chang WH, Chu CH, Wang TE. Adhesive small bowel obstruction: how long can patients tolerate conservative treatment? World J Gastroenterol. 2003;9(3):603-5. https://doi.org/10.3748/wjg.v9.i3.603 [ Links ]
44. Springer JE, Bailey JG, Davis PJ, Johnson PM. Management and outcomes of small bowel obstruction in older adult patients: a prospective cohort study. Can J Surg. 2014;57(6):379-84. https://doi.org/10.1503/cjs.029513 [ Links ]
45. Tavangari FR, Batech M, Collins JC, Tejirian T. Small bowel obstructions in a virgin abdomen: is an operation mandatory? Am Surg. 2016;82(10):1038-42. https://doi.org/10.1177/000313481608201040 [ Links ]
Citation: Idrobo AA, Bastidas BE, Yasno LM, Vargas AL, Merchán-Galvis AM. Presentation and outcome of conservative management of intestinal obstruction caused by adhesions in Cauca. Rev Colomb Gastroenterol. 2020;35(4):447-454. https://doi.org/10.22516/25007440.517
Received: February 29, 2020; Accepted: August 10, 2020











 text in
text in