Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista colombiana de Gastroenterología
Print version ISSN 0120-9957On-line version ISSN 2500-7440
Rev. colomb. Gastroenterol. vol.35 no.4 Bogotá Oct./Dec. 2020 Epub July 12, 2021
https://doi.org/10.22516/25007440.557
Original article
Characterization of patients with liver cirrhosis and bacteremia treated at a university hospital in Medellín-Colombia
1Hepatología clínica, Universidad de Antioquia, Medellín, Colombia
2Unidad de epidemiología, Hospital Pablo Tobón Uribe. Profesor de la Universidad de Antioquia. Medellín, Colombia
3Hepatología clínica, Universidad de Antioquia. Unidad de hepatología y trasplante hepático, Hospital Pablo Tobón Uribe. Medellín, Colombia
4Unidad de hepatología y trasplante hepático, Hospital Pablo Tobón Uribe. Medellín, Colombia
Introduction:
Bacteremia in cirrhotic patients is frequent and associated with high mortality and prolonged hospital stays. This study describes the demographic, clinical, and laboratory characteristics of patients with liver cirrhosis and bacteremia treated at a quaternary care hospital.
Methodology:
Observational, retrospective cohort study. The sample consisted of patients with liver cirrhosis and bacteremia treated between January 1, 2010, and December 31, 2017, at the Hospital Pablo Tobon Uribe of Medellín, Colombia. Demographic, clinical, and laboratory variables were collected. Survival was estimated during the time of hospitalization and up to 30 days following the diagnosis of bacteremia.
Results:
78 patients had cirrhosis and bacteremia. The average age was 65 years; 66.7% were women. Cirrhosis was labeled cryptogenic in 30.8% of the cases and NASH in 19.3%. The main source of infection was the urinary tract (24%), followed by cholangitis (23%) and spontaneous bacteremia (19%). Gram-negative bacteria were observed in most of the isolates (67.9%). The prevalence of MDR was 25.6%, and the adequate use of empirical antibiotics was 80.8%. The 30-day mortality rate was 11.5%. The best mortality predictors were the Child-Pugh and MELD scores on admission with AUROC of 0.79 (P=0.008) and 0.72 (P=0.042), respectively.
Conclusions:
The findings allow describing the main characteristics of patients with cirrhosis who develop bacteremia in our environment. A considerable number of MDR infections were found. Patients with an advanced degree of cirrhosis are at the highest risk of mortality.
Keywords: Liver Cirrhosis; Bacteremia; Colombia
Introducción:
la bacteriemia en pacientes cirróticos es frecuente y se asocia con una alta mortalidad y hospitalización prolongada. Este estudio describe las características demográficas, clínicas y de laboratorio en pacientes con cirrosis hepática y bacteriemia en un hospital de cuarto nivel.
Métodos:
estudio observacional de cohorte retrospectiva. Incluyó pacientes con cirrosis hepática y bacteriemia entre el 1 de enero de 2010 y el 31 de diciembre de 2017 en el Hospital Pablo Tobón Uribe de Medellín, Colombia. Se recogieron variables demográficas, clínicas y de laboratorio. Se estimó la supervivencia durante el tiempo de hospitalización y hasta 30 días desde el diagnóstico de bacteriemia.
Resultados:
se hallaron 78 pacientes con cirrosis y bacteriemia. La media de edad fue de 65 años, 66,7 % fueron mujeres. Las principales etiologías de la cirrosis fueron: criptogénica (30,8 %) y esteatohepatitis no alcohólica (EHNA; 19,3 %). La principal fuente de infección fue la vía urinaria (24 %), seguida de colangitis (23 %) y la bacteriemia espontánea (19 %). Los bacilos gramnegativos (BGN) representaron la mayoría de los aislamientos (67,9 %). La prevalencia de multidrogorresistentes (MDR) fue de 25,6 % y el uso adecuado de antibiótico empírico fue de 80,8 %. La mortalidad a 30 días fue de 11,5 %. Como mejores predictores de mortalidad se encontraron la puntuación Child-Pugh y Model for End-stage Liver Disease (MELD) al ingreso con área bajo la curva ROC (AUROC) de 0,79 (p = 0,008) y 0.72 (p = 0,042), respectivamente.
Conclusiones:
los hallazgos permiten conocer las principales características de los pacientes con cirrosis que desarrollan bacteriemia en nuestro medio. Se encontró un número considerable de infecciones MDR. Los pacientes con un grado avanzado de la cirrosis son los que presentan un mayor riesgo de mortalidad.
Palabras clave: Cirrosis hepática; bacteriemia; Colombia
Introduction
Cirrhosis of the liver is the tenth leading cause of death in the western world1. Infections are major complications in cirrhotic patients in terms of incidence, severity, and overall outcomes2, and are the main cause of admission of these patients to the emergency department. About 20%-30% of hospital admissions due to decompensated cirrhosis cases are associated with an infection or are worsened by infection during hospitalization2-4. Moreover, the need for frequent hospitalizations due to the complications of cirrhosis makes this population vulnerable to nosocomial infections, characterized by multidrug-resistant organisms (MDROs)3,5,6.
Infections in cirrhotic patients have been associated with a 30% mortality rate in the first 30 days and a 66% mortality rate one year after admission to the hospital, making them a significant prognostic factor in patients with end-stage liver disease7.
Bacteremia affects 4%-21% of cirrhotic patients and is up to 10 times more prevalent in this population compared to non-cirrhotic patients8,9. In cirrhosis cases, bacteremia is associated with a high mortality rate, prolonged hospital stays and worsening of liver disease10,11. Cirrhosis of the liver has been found to be an independent predictor of mortality in several studies conducted in patients with bacteremia or candidemia12-14.
However, few studies have addressed the specific characteristics and risk factors for mortality in patients with bacteremia and cirrhosis. The majority of the available data comes from single-center studies, and most of them have been conducted in Europe and Asia.
A research conducted in Argentina by Marciano et al. found that acute kidney failure and mortality rates in patients with spontaneous bacteremia were similar to those in patients with spontaneous peritonitis15. The behavior of this entity is unknown, especially in Colombia. The aim of this study is to describe the demographic, clinical and laboratory characteristics of a cohort of patients with liver cirrhosis and bacteremia treated at a university hospital in Medellín, Colombia. It also describes 30-day survival rates, factors associated with survival, and information of the pathogens that were isolated, their resistance profile, and susceptibility to empirical antibiotic treatment.
Methods
Observational, retrospective cohort study. Patients treated between January 1, 2010, and December 31, 2017, at the inpatient facility of the Hospital Pablo Tobón Uribe (HPTU) in Medellín, Colombia, were included.
Patients diagnosed with cirrhosis of the liver (codes K70.3, K74.3, K74.4, K74.5, K74.6, K71.7) and bacteremia (code A49.9) according to the International Classification of Diseases (ICD-10) were searched in the electronic medical record system of the hospital. The following inclusion criteria were considered: patients over 18 years of age diagnosed with cirrhosis and patients diagnosed with bacteremia during hospitalization. Patients without a clear diagnosis of cirrhosis and those without a report of blood cultures in their medical record were excluded.
Demographic, clinical and laboratory variables were measured. Cirrhosis of the liver diagnosis was established based on histology or clinical, biochemical, or imaging findings. Non-infectious complications of cirrhosis (ascites, esophageal varices, hepatorenal syndrome, hepatic encephalopathy, hepatocarcinoma) were defined using the criteria of the European Association for the Study of the Liver (EASL) and the International Club of Ascites16.
Bacteremia was defined based on the isolation of a non-contaminating microorganism of the skin in 1 or more blood cultures, or the isolation of a common skin contaminating microorganism (diphtheroids, Bacillus spp, Propionibacterium spp, coagulase-negative staphylococci, or micrococcus) in 2 or more blood cultures. Furthermore, it was classified as community-acquired infection, associated with the provision of health care, or nosocomial, according to Friedman’s criteria17. Spontaneous bacteremia was considered in the presence of positive blood cultures (with no contamination) in the absence of a source of infection.
The source of the infection was determined based on what was reported in the medical record. Spontaneous bacterial peritonitis (SBP) was diagnosed when there were 250 or more polymorphonuclear cells in ascitic fluid, with or without microbiological isolates. If the patient had this diagnosis, it was considered to be the source of bacteremia when no other focus of infection was identified.
Isolated microorganisms were classified according to their susceptibility as multidrug-resistant (MDR) or non-MDR based on the specifications of the European Society of Clinical Microbiology and Infectious Diseases (ESCMID), which defines MDR as the absence of susceptibility to at least one agent in 3 or more antibiotic categories18.
Data were collected by reviewing medical records with a previously designed collection instrument. To ensure data quality and reduce the risk of information bias, 10% of medical records were reviewed twice by the researchers. Patients were followed up on for 30 days after being diagnosed with bacteremia, or until the last date reported in their medical record.
Categorical variables are presented as absolute and relative frequencies. Continuous variables are expressed as means and standard deviations (SD) if they have a normal distribution, and medians interquartile ranges (IQR) if they do not have a normal distribution; data normality was determined using the Shapiro-Wilk test. The incidence density rate of mortality in patients with cirrhosis and bacteremia was estimated as follows: number of patients who died divided by the sum of follow-up time for all patients.
Survival was estimated using the Kaplan-Meier estimator during the time of hospitalization, considering the variables that have been associated with mortality due to biological plausibility (such as Child-Pugh score, Model for End-stage Liver Disease [MELD], acute-on-chronic liver failure [ACLF], among others) in several studies. In the exploratory analysis, the performance of different variables to predict mortality during hospitalization on admission, at the moment bacteremia was diagnosed, and at 24 and 48 hours. The statistical package SPSS version 20.0 of the Universidad de Antioquia was used for performing all statistical analysis.
No sample size was estimated a priori since all patients with liver cirrhosis and a diagnosis of bacteremia treated at the hospital during the study period were included.
This study was approved by the Ethics committee of HPTU. The ethical principles for conducting clinical research outlined in Resolution 8430 of 1993 issued by the Ministry of Social Protection of the Republic of Colombia, as well as the recommendations of the seventh revision (2013) of the Declaration of Helsinki for conducting biomedical research involving human beings, were followed. The final version of the manuscript adhered to the Strengthening the Reporting of Observational studies in Epidemiology (STROBE) recommendations for reporting observational studies19.
Results
A total of 78 patients with cirrhosis of the liver and bacteremia were included (Table 1). Their average age was 65 years, and 66.7 % of them were women. The main etiologies of cirrhosis were cryptogenic (30.8 %), non-alcoholic steatohepatitis (NASH; 19.2 %) and alcohol consumption (19.,2 %). 8 patients (10.3 %) had no other medical history or comorbidities other than cirrhosis, 19 % had at least one comorbidity, and 71 % had two or more, the most common being high blood pressure (HBP) in 44.9 % (35 cases), diabetes in 37.2 % (29 cases), and obesity or overweight in 14.1 % (11 cases). Regarding cirrhosis severity, 17.9 % (14 patients), 53.3 % (42 patients), and 28.2 % (22 patients) had Child-Pugh classes A, B, and C, respectively, with an average MELD score on admission of 15.1.
Table 1 Characteristics of the 78 patients with confirmed cirrhosis and bacteremia diagnosis
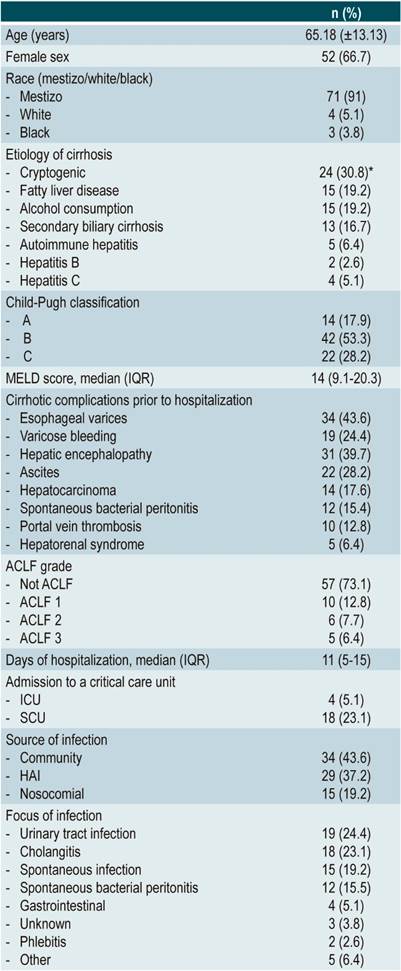
*The sum does not result in 100% since the cause is not clear in the other cases. ACLF: Acute-on-chronic liver failure; HAI: health care-associated infection; SCU: special care unit; ICU: intensive care unit.
The main foci of bacteremia were urinary tract infections in 24.4 % of patients (19 cases), cholangitis in 23.1 % (18 cases), spontaneous bacteremia in 19.2 % (15 cases) and SBP in 15.4 % (12 cases). Community-acquired infections were the main source of infection (43.6 %; 34 cases), followed by health care-associated infections (37.2 %; 29 cases), and nosocomial infections (19.2 %; 15 cases). The mean time for reporting a positive culture since hospital admission was 1.8 days (range: 0-34).
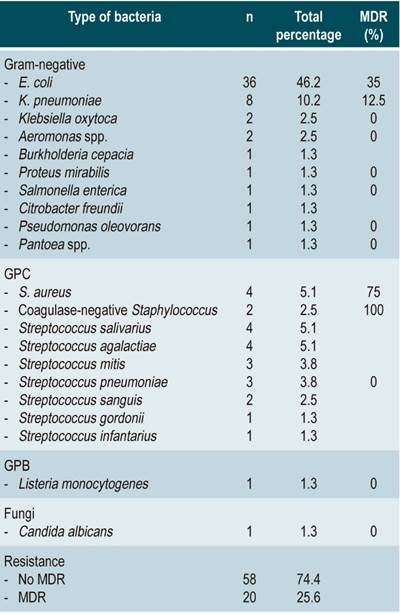
Gram-negative bacilli (GNB) were found in most cases (53; 67.9 %); of these, Escherichia coli was the most frequent, with 36 cases (46.2 %), followed by Klebsiella pneumoniae with 8 cases (10.3 %). Gram-positive cocci (GPC) accounted for 30.8 % of the cases (24), and streptococcus was the most frequent bacteria (24.4 %; 19 cases). In two cases (2.6%) 2 or more bacteria were found, both were survivors. In turn, BGN and Candida tropicalis were found in a patient who died. The prevalence of MDR was 25.6 % (20 cases), with five cases of extended-spectrum beta-lactamase (ESBL)-producing Escherichia coli, two AmpC betalactamase-producing E. coli, one ESBL- producing Klebsiella pneumoniae and three methicillin-resistant Staphylococcus aureus (Table 2).
Table 2 Microorganisms isolated in blood cultures of patients with cirrhosis of the liver and bacteremia.
Exploratory analysis of variables associated with mortality
The mortality rate was 11.5%. The median MELD score was 13 (IQR: 8.9-19.9) and 14.57 (IQR: 9.1-19.1) in survivors versus 21.06 (IQR: 12.5-27.2) and 20.26 (IQR: 11-23) in patients who died on admission and at the time of bacteremia diagnosis, respectively, with statistically significant differences on admission (p = 0.041) (Table 3, Figure 1). The mean length of hospital stay in the survivors group was 11 days (IQR: 1-21) versus 13 days (IQR: 1-24) in the non-survivors group, respectively, without significant differences (p = 0.573).
Table 3 Comparison of baseline conditions on admission: Survivors versus non-survivors
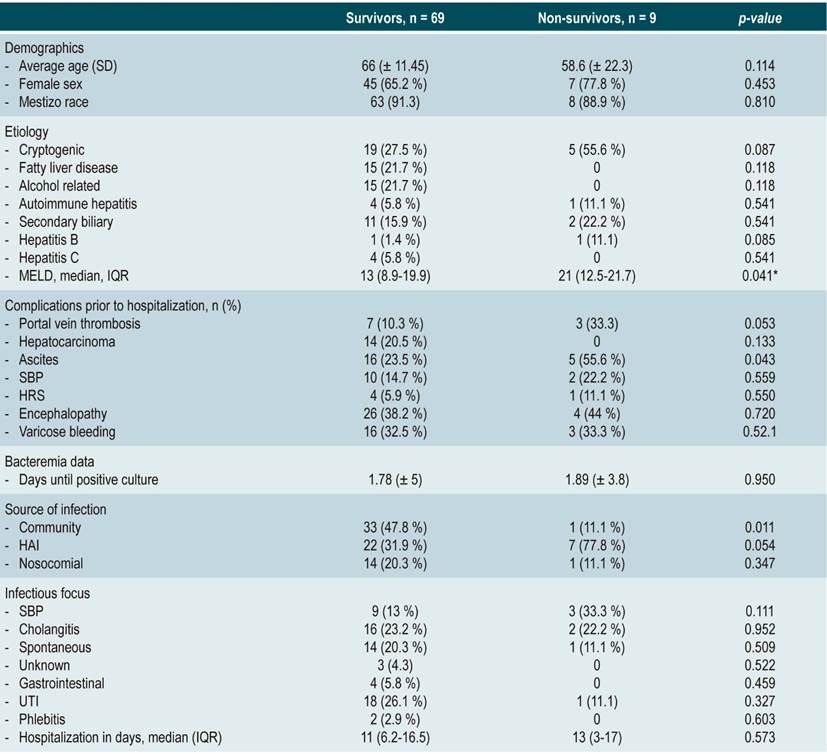
*Difference of medians. HAI: healthcare-associated infection; UTI: urinary tract infection; HRS: hepatorenal syndrome.
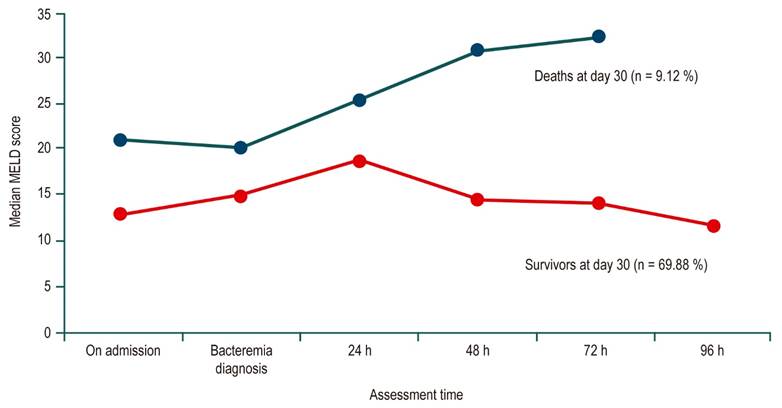
Figure 1 Median MELD score pattern of cirrhotic patients with bacteremia from hospital admission to 30 days after admission in survivors (red line) and non-survivors (blue line).
Urinary tract infections (26.5 %), spontaneous bacteremia (20.3 %) and cholangitis (23.5 %) were the most frequent infection foci among survivors, in contrast to non-survivors, in whom SBP (33.3 %) and cholangitis (22.2 %) were the most frequent, although no statistically significant differences were observed (Figure 2). Mortality rates in bacteremia caused by gram-negative bacteria and gram-positive bacteria were 13.5% and 7.7 %, however the difference was not statistically significant (p = 0.453). Proper use of empirical antibiotic was reported in 80.8 % of patients, with no difference between survivors and non-survivors (79.4 % and 88.9 %, respectively). There were no significant differences regarding the type of bacterial isolate or the MDR profile between survivors and non-survivors; however, in non-survivors, healthcare-associated infection as a source of infection was significantly higher (31.1 % vs 77.8 %; p = 0.007).
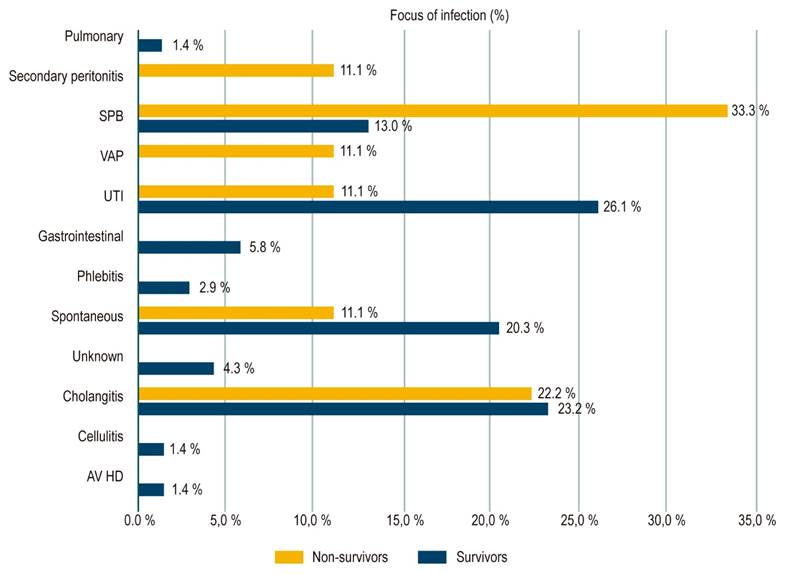
Figure 2 Frequency of clinical outbreaks of bacteremia in surviving and dead cirrhotic patients 30 days after infection. VA HD: vascular access for hemodialysis; VAP: ventilator-associated pneumonia.
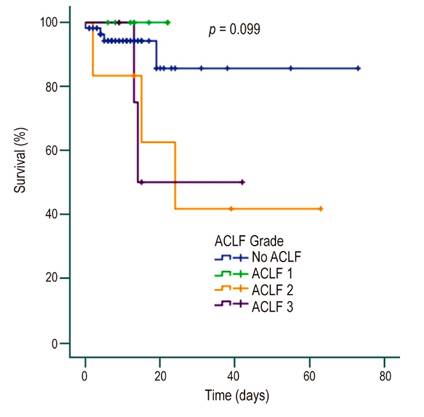
Regarding the degree of acute-on-chronic liver failure (ACLF), 10 (12.8 %), 6 (7.7 %) and 5 (6.4 %) patients had ACLF grades 1, 2 and 3, respectively, on admission, with mortality rates of 40 % and 50 % for the last two grades, 7 % in non-ACLF and no mortality in ACLF grade 1. There were statistically significant differences and a statistically significant association in mortality between non-ACLF and ACLF 1 vs. ACLF 2 and 3 (4/66 vs 5/11; p = 0.0001). Concerning the severity of cirrhosis, the higher the Child-Pugh class, the higher the mortality rate, with a statistically significant difference (p = 0.037) and, although there was also a trend according to the ACLF grade, this difference was not significant (p = 0.09) (Figures 3 and 4).
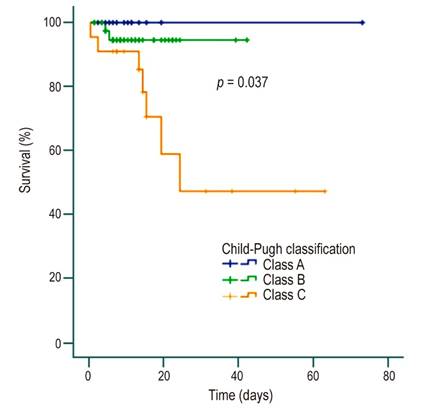
Figura 4 Survival curve in patients with cirrhosis and bacteremia according to Child-Pugh classification.
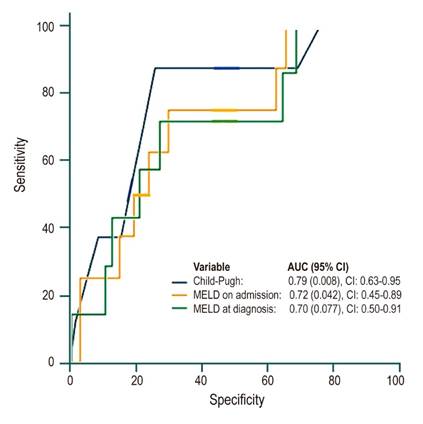
The best predictors of mortality were Child-Pugh and MELD scores on admission with areas under the ROC curve of 0.79 (p = 0.008; 95% confidence interval [CI]: 0.63-0.95) and 0.72 (p = 0.042; 95% CI: 0.45-0.89), respectively (Figure 5).
Discussion
To the best of our knowledge, this study is the largest of its kind published in Latin America. Most of studies addressing infection in cirrhotic patients have been conducted in patients with SBP, but only a few have described the epidemiological characteristics of bacteremia in this population. In fact, two of the largest studies on incidence, etiological distribution, and outcomes of bacteremia in cirrhotic patients were published more than a decade ago9,20. In Latin America, a study carried out in Chile described the characteristics of 59 patients with bacteremia associated with chronic liver disease, with a predominance of GPC infections and with a mortality rate of 37 %21. Another study conducted in Argentina found that patients with spontaneous bacteremia had similar mortality and kidney failure rates to those with spontaneous peritonitis15.
The present study found a high percentage of cryptogenic and NASH cirrhosis, associated with a high rate of comorbidities related to metabolic syndrome, suggesting that some of the patients listed as cryptogenic cirrhosis actually had NASH; however, liver biopsy would not be recommended as it would not change the therapeutic approach or improve liver prognosis. Most events occurred in Child-Pugh class B cirrhosis patients, and up to 20% of cases required admission to the intensive care unit (ICU) for the management and monitoring of their condition. The main source of infection was the urinary tract, followed by the biliary tract, SBP and spontaneous cirrhotic bacteremia, which is consistent with the main infectious complications described in patients with end-stage liver disease, favored by immunosuppression caused by liver failure, among other factors22.
The 30-day mortality rate was 11.5%, which is much lower than mortality rates reported in other studies15,22-26, probably because the patients included in this study had less liver failure (28% were classified as Child-Pugh class C) and 73% did not develop ACLF. Median MELD score on admission and at the time of diagnosis of bacteremia was much higher in non-survivors than in survivors, with a statistically significant difference. In the group of patients who died, a greater liver failure according to the Child-Pugh classification was found, and as well as a higher degree of ACLF with a statistically significant difference when grades 2 and 3 were compared with grade 1 and the non-ACLF group. Child-Pugh and MELD scores were the best predictors of mortality in the study population. Other authors have reported that variables such as Delta MELD (24, 48, and 72 hours), SBP as a source of infection, inappropriate empirical antibiotic therapy, and the presence of severe sepsis or septic shock are associated with a higher mortality at 30 days23. We believe that this relationship cannot be established in the present study because of the small number of patients who died at 30 days and the lack of data for calculating Delta MELD.
GNB infections accounted for more than 66% of cases, and E. coli was the main pathogen with 46% and a MDR rate of 35%. Strikingly, 75% and 100% of S. aureus and coagulase-negative staphylococci infections, respectively, were caused by a MDR bacteria (methicillin-resistant). In our healthcare institution, empirical antibiotic coverage of cirrhotic patients with community-acquired infections includes the use of piperacillin/tazobactam and meropenem for healthcare-associated or nosocomial infections (+/- vancomycin depending on the suspicion of resistant GPC), which translates into the large percentage of appropriate empirical coverage reported here (more than 80%).
The present study has some limitations. It is a single-center study; therefore, data presented here may not be representative of other institutions. However, our hospital is a referral center for patients with liver disease coming from different regions of the country. Also, the development of acute renal failure, which has been shown to have a short-term impact on this group of patients, was not evaluated15. Finally, the number of events is small, mainly mortality cases at 30 days, which makes it difficult to create greater predictors of fatal outcomes in this population.
Conclusion
This research does not provide information on the key characteristics of patients with liver cirrhosis who experience bacteremia in Colombia. The etiological study revealed the main bacteria that affect this population with a considerable amount of MDR infections that are on the rise, not only in our country but also worldwide, progressively limiting the way we treat our patients. Patients with advanced chronic liver disease at the time of hospitalization and diagnosis of bacteremia, as well as a high ACLF grade (2 or 3), are at a higher risk of a fatal outcome and, therefore, require more attention.
REFERENCES
1. Leon DA, McCambridge J. Liver cirrhosis mortality rates in Britain from 1950 to 2002: an analysis of routine data. Lancet. 2006;367(9504):52-6. http://dx.doi. org/10.1016/S0140-6736(06)67924-5 [ Links ]
2. Fernandez J, Gustot T. Management of bacterial infections in cirrhosis. J Hepatol. 2012;56 Suppl 1:S1-12. http://dx.doi.org/10.1016/S0168-8278 (12)60002-6 [ Links ]
3. Fernandez J, Acevedo J, Castro M, Garcia O, de Lope CR, Roca D, Pavesi M, Sola E, Moreira L, Silva A, Seva-Pereira T, Corradi F, Mensa J, Ginès P, Arroyo V. Prevalence and risk factors of infections by multiresistant bacteria in cirrhosis: a prospective study. Hepatology. 2012;55(5):1551-61. http://dx.doi.org/10.1002/hep.25532 [ Links ]
4. Pant C, Olyaee M, Gilroy R, Pandya PK, Olson JC, Oropeza-Vail M, Rai T, Deshpande A. Emergency department visits related to cirrhosis: a retrospective study of the nationwide emergency department sample 2006 to 2011. Medicine (Baltimore). 2015;94(1):e308. http://dx.doi.org/10.1097/MD.0000000000000308 [ Links ]
5. Merli M, Lucidi C, Giannelli V, Giusto M, Riggio O, Falcone M, Ridola L, Attili AF, Venditti M. Cirrhotic patients are at risk for health care-associated bacterial infections. Clin Gastroenterol Hepatol. 2010;8(11):979-85. http://dx.doi.org/10.1016/j.cgh.2010.06.024 [ Links ]
6. DeRosa FG, Corcione S, Filippini C, Raviolo S, Fossati L, Montrucchio C, Aldieri C, Petrolo A, Cavallo R, Di Perri G. The Effect on mortality of fluconazole or echinocandins treatment in candidemia in internal medicine wards [corrected]. PLoS One. 2015;10(5):e0125149. http://dx.doi.org/10.1371/journal.pone.0125149 [ Links ]
7. Arvaniti V, D’Amico G, Fede G, Manousou P,Tsochatzis E, Pleguezuelo M, Burroughs AK. Infections in patients with cirrhosis increase mortality fourfold and should be used in determining prognosis. Gastroenterology. 2010;139(4):1246-56, 1256.e1-5. http://dx.doi.org/10.1053/j.gastro.2010.06.019 [ Links ]
8. Leber B, Spindelboeck W, Stadlbauer V. Infectious complications of acute and chronic liver disease. Semin Respir Crit Care Med. 2012;33(1):80-95. http://dx.doi.org/10.1055/s-0032-1301737 [ Links ]
9. Thulstrup AM, Sorensen HT, Schonheyder HC, Moller JK, Tage-Jensen U. Population-based study of the risk and short-term prognosis for bacteremia in patients with liver cirrhosis. Clin Infect Dis. 2000;31(6):1357-61. http://dx.doi.org/10.1086/317494 [ Links ]
10. Aggarwal A, Ong JP, Younossi ZM, Nelson DR, Hoffman-Hogg L, Arroliga AC. Predictors of mortality and resource utilization in cirrhotic patients admitted to the medical ICU. Chest. 2001;119(5):1489-97. http://dx.doi.org/10.1378/chest.119.5.1489 [ Links ]
11. Jalan R, Fernandez J, Wiest R, Schnabl B, Moreau R, Angeli P, Stadlbauer V, Gustot T, Bernardi M, Canton R, Albillos A, Lammert F, Wilmer A, Mookerjee R, Vila J, Garcia-Martinez R, Wendon J, Such J, Cordoba J, Sanyal A, Garcia-Tsao G, Arroyo V, Burroughs A, Ginès P. Bacterial infections in cirrhosis: a position statement based on the EASL Special Conference 2013. J Hepatol. 2014;60(6):1310-24. http://dx.doi.org/10.1016/j.jhep.2014.01.024 [ Links ]
12. Al-Hasan MN, Lahr BD, Eckel-Passow JE, Baddour LM. Predictive scoring model of mortality in Gram-negative bloodstream infection. Clin Microbiol Infect. 2013;19(10):948-54. http://dx.doi.org/10.1111/14690691.12085 [ Links ]
13. De Rosa FG, Corcione S, Raviolo S, Montrucchio C, Aldieri C, Pagani N, Di Perri G. Candidemia, and infections by Clostridium difficile and carbapenemase-producing Enterobacteriaceae: new enteropathogenetic opportunistic syndromes? Infez Med. 2015;23(2):105-16. [ Links ]
14. Kang CI, Song JH, Chung DR, Peck KR, Yeom JS, Ki HK, Son JS, Lee JS, Kim YS, Jung SI, Kim SW, Chang HH, Ryu SY, Kwon KT, Lee H, Jung DS, Moon C, Heo ST, Kim ES, Rhee JY; Korean Network for Study on Infectious Diseases. Liver cirrhosis as a risk factor for mortality in a national cohort of patients with bacteremia. J Infect. 2011;63(5):336-43. http://dx.doi.org/10.1016/j.jinf.2011.07.012 [ Links ]
15. Marciano S, Dirchwolf M, Bermudez CS, Sobenko N, Haddad L, Genre F, Barcán L, Smud A, Posadas-Martínez ML, Giunta D, Gadano A. Spontaneous bacteremia and spontaneous bacterial peritonitis share similar prognosis in patients with cirrhosis: a cohort study. Hepatol Int. 2018;12(2):181-190. http://dx.doi.org/10.1007/s12072-017-9837-7 [ Links ]
16. European Association for the Study of the Liver. EASL clinical practice guidelines on the management of ascites, spontaneous bacterial peritonitis, and hepatorenal syndrome in cirrhosis. J Hepatol. 2010;53(3):397-417. http://dx.doi.org/10.1016/j.jhep.2010.05.004 [ Links ]
17. Friedman ND, Kaye KS, Stout JE, McGarry SA, Trivette SL, Briggs JP, Lamm W, Clark C, MacFarquhar J, Walton AL, Reller LB, Sexton DJ. Health care--associated bloodstream infections in adults: a reason to change the accepted definition of community-acquired infections. Ann Intern Med. 2002;137(10):791-7. http://dx.doi.org/10.7326/0003-4819-137-10-200211190-00007 [ Links ]
18. Magiorakos AP, Srinivasan A, Carey RB, Carmeli Y, Falagas ME, Giske CG, Harbarth S, Hindler JF, Kahlmeter G, Olsson-Liljequist B, Paterson DL, Rice LB, Stelling J, Struelens MJ, Vatopoulos A, Weber JT, Monnet DL. Multidrug-resistant, extensively drug-resistant and pandrug-resistant bacteria: an international expert proposal for interim standard definitions for acquired resistance. Clin Microbiol Infect. 2012;18(3):268-81. http://dx.doi.org/10.1111/j.1469-0691.2011.03570.x [ Links ]
19. von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP; STROBE Initiative. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Ann Intern Med. 2007;147(8):573-7. http://dx.doi.org/10.7326/0003-4819-147-8-200710160-00010 [ Links ]
20. Campillo B, Dupeyron C, Richardet JP. Epidemiology of hospital-acquired infections in cirrhotic patients: effect of carriage of methicillin-resistant Staphylococcus aureus and influence of previous antibiotic therapy and norfloxacin prophylaxis. Epidemiol Infect. 2001 Dec;127(3):443-50. http://dx.doi.org/10.1017/s0950268801006288 [ Links ]
21. Munita JM, Araos R, Pérez J, Álvarez A, Canals M, Conteras J, Marcotti A, Thompson L, Noriega LM. Bacteriemia en daño hepático crónico. Rev. chil. infectol. 2011;28(1):35-9. http://dx.doi.org/10.4067/S0716-10182011000100006 [ Links ]
22. Albillos A, Lario M, Alvarez-Mon M. Cirrhosis-associated immune dysfunction: distinctive features and clinical relevance. J Hepatol 2014;61(6):1385-96. http://dx.doi.org/10.1016/j.jhep.2014.08.010 [ Links ]
23. Bartoletti M, Giannella M, Caraceni P, Domenicali M, Ambretti S, Tedeschi S, Verucchi G, Badia L, Lewis RE, Bernardi M, Viale P. Epidemiology and outcomes of blood- stream infection in patients with cirrhosis. J Hepatol. 2014;61(1):51-8. http://dx.doi.org/10.1016/j.jhep.2014.03.021 [ Links ]
24. Hsieh CC, Lee CC, Chan TY, Hong MY, Chi CH, Ko WC. Clinical features and impact of empirical therapy in cirrhotic adults with community-onset bacteremia. Am J Emergency Med. 2015;33(2):222-8. http://dx.doi.org/10.1016/j.ajem.2014.11.024 [ Links ]
25. Park H, Jang KJ, Jang W, Park SH, Park JY, Jeon TJ, Oh TH, Shin WC, Choi WC, Sinn DH. Appropriate empirical antibiotic use and 30-d mortality in cirrhotic patients with bacteremia. World J Gastroenterol. 2015;21(12):3587-92. http://dx.doi.org/10.3748/wjg.v21.i12.3587 [ Links ]
26. Brandolini M, Corbella M, De Silvestri A, Tinelli C, Albonico G, Albertini R, Ludovisi S, Bruno R, Marone P, Minoli L, Seminari E. Epidemiological characteristics of bloodstream infections in patients with different degrees of liver disease. Infection. 2015;43(5):561-7. http://dx.doi.org/10.1007/s15010-015-0794-6 [ Links ]
Citation: Luján-Ramos MA, Díaz-Ramírez GS, Martínez-Casas OY, Morales-Ortiz AF, Donado-Gómez JH, Restrepo-Gutiérrez JC, Marín-Zuluaga JI. Characterization of patients with liver cirrhosis and bacteremia treated at a university hospital in Medellín-Colombia. Rev Colomb Gastroenterol. 2020;35(4):455-464. https://doi.org/10.22516/25007440.557
Received: May 30, 2020; Accepted: July 08, 2020











 text in
text in