Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista colombiana de Gastroenterología
Print version ISSN 0120-9957On-line version ISSN 2500-7440
Rev. colomb. Gastroenterol. vol.35 no.4 Bogotá Oct./Dec. 2020 Epub July 12, 2021
https://doi.org/10.22516/25007440.404
Case report
Ball Valve syndrome caused by a colon polyp. Case report (with video)
1Médico internista y gastroenterólogo, Unidad de Gastroenterología y Ecoendoscopia (UGEC), Hospital Universitario Nacional. Profesor de Medicina, Universidad Nacional de Colombia. Gastroenterólogo adscrito, Hospital Universitario Fundación Santa Fe; Bogotá, Colombia.
2Médico internista, gastroenterólogo, Universidad Nacional de Colombia, Hospital Universitario Nacional de Colombia; Bogotá, Colombia.
Intestinal obstruction is a potentially lethal pathology, and its treatment is usually surgical. The following is the case of a patient with abdominal pain and recurrent intestinal obstruction, in whom a large pediculated polyp that caused partial obstruction by Ball valve effect was observed during a colonoscopy.
Keywords: Polyp; Ball Valve; Bowel obstruction; Polypectomy
La obstrucción intestinal es una patología potencialmente letal y cuyo tratamiento, por lo general, es quirúrgico. Presentamos el caso de un paciente con dolor abdominal y clínica de obstrucción intestinal recurrente, en quien se documenta, durante una colonoscopia, un gran pólipo pediculado que causaba obstrucciones parciales por el fenómeno de ball valve.
Palabras clave: Pólipo; ball valve; obstrucción intestinal; polipectomía
Introduction
Ball valve syndrome was first described in 1946 by Hobbs and Cohen1. Since then, it has been recognized as a rare but serious cause of recurrent abdominal pain2. It mostly affects the upper digestive tract3 and involves, in order of frequency, the duodenum and the pylorus due to prolapsing lesions4. Its etiology is variable and may be related to benign polyps, tumors, and subepithelial lesions, such as large lipomas5. Although colonic involvement has been reported, it is considered very rare6. This is, to the best of our knowledge, the first Ball Valve case reported in Colombia.
Clinical case
42-year-old patient with multiple hospital admissions due to a 3-month history of abdominal pain, vomiting, weight loss, and altered bowel habits that caused episodes of alternating constipation and diarrhea. During his last admissions to the emergency department, he was diagnosed with intestinal obstruction according to the information reported in the patient’s medical record. However, the patient had a rapid response to medical management, and biochemical tests results were normal, but a nonspecific ileus was identified in a non-contrast abdominal radiography (X-ray). In turn, a computed tomography (CT) scan of the abdomen was performed, showing an unspecific thickening of the sigmoid colon. Given the symptoms persistence, the general surgery service decided to hospitalize the patient and schedule a diagnostic laparoscopy.
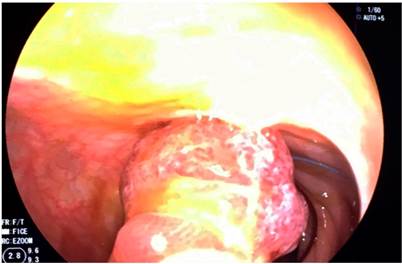
During his hospital stay, the patient presented an exacerbation of the symptoms, which was then worsened by hematochezia. For this reason, a total colonoscopy was requested. In the colonoscopy a large 40 mm pedunculated polyp was observed with a long pedicle of approximately 30 mm in the sigmoid colon, showing a prolapse caused by peristalsis that generated an obstruction of the colonic lumen (Figures 1,2,3y4). The polyp’s head was eroded, which was a possible cause of hematochezia.
Then, performing an endoscopic polypectomy was decided. In addition, because of the size of the pedicle, a hemostatic loop (endoloop) was inserted. The polypectomy loop was then used, and the polyp was resected (Video 1).
Video 1. Ball valve syndrome in the colon.
Consequently, the patient’s condition had a favorable progress, symptoms resolved, and the individual remained asymptomatic throughout a 5-month follow-up. An adenomatous polyp was identified in the pathology report.
Discussion
Ball valve syndrome is a mechanical complication of large endoluminal lesions7. They can cause pseudo-obstruction due to intermittent prolapses facilitated by peristalsis, which temporarily occupy the lumen8. Symptoms will depend on the location of the lesion.
Since it is considered a dynamic phenomenon, symptoms are usually self-limiting9, which is why this condition also tends to become chronic4 due to significant nutritional repercussions, unexplained weight loss and symptomatic manifestations that can easily be mistaken for a neoplastic disease10. This scenario implies the performance of multiple studies and interventions (in some cases unnecessary), as well as unacceptable repercussions on the patient’s quality of life11.
Endoscopic treatment is widely recommended; however, depending on the nature of the lesion, complementary surgical management may be required2
REFERENCES
1. de la Plaza R, Picardo AL, Cuberes R, Jara A, Martínez-Peñalver I, Villanueva MC, Medina M, Alías D, Osorio S, Pacheco E, Suárez A. Inflammatory fibroid polyps of the large intestine. Dig Dis Sci. 1999;44(9):1810-6. http://doi.org/10.1023/a:1018886421409 [ Links ]
2. Macedo G, Lopes S, Albuquerque A. Ball valve syndrome: gastric polypectomy as a safe endoscopic treatment of a potentially troublesome condition. Gastrointest Endosc. 2012;76(5):1080-1. http://doi.org/10.1016/j.gie.2012.06.018 [ Links ]
3. Akbulut S. Intussusception due to inflammatory fibroid polyp: a case report and comprehensive literature review. World J Gastroenterol. 2012;18(40):5745-5752. http://doi.org/10.3748/wjg.v18.i40.5745 [ Links ]
4. Martins CR, Gamito É, Oliveira AP. Ball valve syndrome caused by a giant gastric Vanek’s tumor. Rev Esp Enferm Dig. 2017;109(3):237-238. http://doi.org/10.17235/reed.2017.4526/2016 [ Links ]
5. Sun CK, Yang KC, Liao CS. Endoscopic Management of Gastric Polyp with Outlet Obstruction without Polypectomy. Case Rep Gastroenterol. 2011;5(2):267-271. http://doi.org/10.1159/000328443 [ Links ]
6. Kimura H, Yoshida T, Takahashi I. Ball valve syndrome. Gastrointest Endosc. 2003;58(1):99. [ Links ]
7. Sebastian S, Addley J, Crotty P, Buckley M. Giant gastric polyp. Gastrointest Endosc. 2004;59(3):398-9. http://doi.org/10.1016/s0016-5107(03)02595-1 [ Links ]
8. Ozturk O, Koklu S, Sokmensuer C, Uner H. A giant benign polyp of the stomach. Gastroenterol Nurs. 2016;39(6):478-480. http://doi.org/10.1097/SGA.0000000000000239 [ Links ]
9. Yriberry Ureña S, Vila Guitérrez S, Salazar Muente F. Polypectomy and endoscopic management of a giant gastric polyp. Rev Gastroenterol Perú. 2010;30(2):167-71. [ Links ]
10. Iso Y, Sawada T, Rokkaku K, Shimoda M, Kubota K. Ball-valve gastric tumor associated with anomalous junction of the pancreatico-biliary ductal system and a right-sided round ligament: report of a case. Surg Today. 2008;38(5):458-62. http://doi.org/10.1007/s00595-007-3635-0 [ Links ]
11. Pinto-Pais T, Fernandes S, Proença L, Fernandes C, Ribeiro I, Sanches A, Carvalho J, Fraga J. A Large Gastric Inflammatory Fibroid Polyp. GE Port J Gastroenterol. 2015;22(2):61-64. http://doi.org/10.1016/j.jpge.2014.07.006 [ Links ]
Citation: Gómez MA, Ruiz OF, Marulanda-Fernández H. Ball Valve syndrome caused by a colon polyp. Case report (with video). Rev Colomb Gastroenterol. 2020;35(4):519-521. https://doi.org/10.22516/25007440.404
Received: January 30, 2018; Accepted: March 30, 2018











 text in
text in