Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Revista colombiana de Gastroenterología
versión impresa ISSN 0120-9957versión On-line ISSN 2500-7440
Rev. colomb. Gastroenterol. vol.35 no.4 Bogotá oct./dic. 2020 Epub 12-Jul-2021
https://doi.org/10.22516/25007440.400
Case report
Endoscopic ultrasonography-guided cholecystogastrostomy in a patient with pancreatic cancer: the first case in Colombia (with video)
1Grupo de Gastroenterología, Fundación Santa Fe; Bogotá, Colombia.
2Grupo de Cirugía General, Fundación Santa Fe; Bogotá, Colombia.
3Residente de Cirugía General, Universidad El Bosque; Bogotá, Colombia.
The current treatment of malignant biliary obstruction is non-surgical biliary diversion with palliative intent. The surgery having specific indications in patients with malignant pathology with curative intent. However, duodenal obstruction and non-dilated intra- or extrahepatic bile duct make these surgical and endoscopic procedures guided by EUS difficult.
We present our experience with the first case in Colombia, a third-world country in Latin America, of a cholecystogastrostomy guided by endoscopic ultrasound (EUS) in a patient with unresectable pancreatic cancer and duodenal invasion with dilated common bile duct using a luminal stent (LAMS) (HOT AXIOS stent, Xlumena Inc.; Mountain View, CA, USA) 15 mm × 10 mm.
EUS-guided cholecystogastrostomy should be considered as an option for biliary decompression of greater importance than percutaneous drainage since it is superior in terms of technical feasibility, safety and efficacy in specific cases of ampullary stenosis and duodenal invasion. In addition, it can be done in third world countries when it has the appropriate training and implements. The fully covered metal stent applied to light (HOT AXIOS stent, Xlumena Inc.; Mountain View, CA, USA) is ideal for EUS guided cholecystogastrostomy to minimize complications such as bile leakage. Additional comparative studies are needed to validate the benefits of this technique.
Keywords: Endoscopic ultrasonography; cholecystogastrostomy; lumen apposing metal stent
El tratamiento actual para la obstrucción biliar maligna es la derivación biliar no quirúrgica con propósito paliativo. La cirugía tiene indicaciones específicas en pacientes con patología maligna con propósito curativo. Sin embargo, la obstrucción duodenal y del conducto biliar intra o extrahepático no dilatado hace que esta cirugía y el procedimiento endoscópico guiado por ultrasonografía endoscópica (USE) sean difíciles de realizar.
Presentamos nuestra experiencia con el primer caso en Colombia, un país latinoamericano del tercer mundo. Consistió en una colecistogastrostomía guiada por USE, a partir de la utilización de una endoprótesis luminal (Lumen-apposing metal stents, LAMS) (HOT AXIOS stent, Xlumena Inc.; Mountain View, CA, Estados Unidos) de 15 mm × 10 mm, en un paciente masculino con cáncer pancreático inoperable e invasión duodenal con conducto colédoco dilatado.
La colecistogastrostomía guiada por USE podría ser considerada como una opción de más importancia para la descompresión biliar que el drenaje percutáneo, ya que es superior en términos de viabilidad técnica, seguridad y eficacia en casos específicos de estenosis ampular e invasión duodenal. Además, puede ser realizada en países del tercer mundo, cuando se cuenta con el entrenamiento y los instrumentos adecuados. La endoprótesis metálica totalmente recubierta, aplicada a luz (HOT AXIOS stent, Xlumena Inc.; Mountain View, CA, Estados Unidos), es ideal para la colecistogastrostomía guiada por USE, a fin de minimizar complicaciones como fugas biliares. Se necesitan estudios comparativos adicionales para validar los beneficios de esta técnica.
Palabras clave: Ultrasonografía endoscópica; colecistogastrostomía; endoprótesis metálica de aposición luminal
Introduction
Echoendoscopies are very useful not only as gastrointestinal endoscopic ultrasound (EUS) diagnostic tools and to perform fine-needle aspiration biopsies (EUS-FNA), but also as therapeutic methods with EUS-guided drainage procedures, such as choledoduodenostomy and hepaticogastrostomy. The latter has been used as an alternative for biliary decompression due to malignant biliary obstruction1,2.
Current treatment for malignant biliary obstruction is a non-surgical biliary stenting for palliative purposes, and surgery has specific indications for curative purposes in patients with malignant disease. However, duodenal obstruction and the extrahepatic bile duct make EUS-guided surgical and endoscopic procedures difficult.
In this context, we present our experience with the first case of EUS-guided cholecystogastrostomy reported in Colombia, a developing Latin American country. The procedure was performed using a 15 mm × 10 mm lumen-apposing metal stent (LAMS) (HOT AXIOS stent, Xlumena Inc.; Mountain View, CA, United States) in a male patient with inoperable pancreatic cancer and duodenal invasion with dilated bile ducts.
Patient preparation
Starting broad-spectrum intravenous antibiotic therapy started before the carrying out the procedure, as well as performing pre-procedural magnetic resonance cholangiopancreatography and abdominal computed tomography (CT) in all patients in order to create a map of the biliary tree is recommended.
Patients who are eating need a light meal at noon, without vegetables, followed by a clear liquid diet. If pseudo-obstruction and functional gastric-organic or intestinal obstruction occurs, adding prokinetic drugs and inserting a nasogastric tube to keep the gastric and duodenal lumen clean during the procedure is recommended. Also, blood clotting status in individuals treated with non-steroidal anti-inflammatory drugs, antiplatelet drugs, or anticoagulants must be improved prior to the intervention.
EUS-guided cholecystogastrostomy using a lumen-apposing metal stent (HOT AXIOS) is a relatively long procedure and must be performed in patients under conscious sedation or general anesthesia. Pulse oximetry, electrocardiography and capnography must be available during the procedure, and intubation may be necessary. The procedure is performed with a patient placed in a left lateral decubitus position, using X-rays. In the end, however, it is preferable to place the patient in a supine position to obtain a good projectional radiography and locate the pneumoperitoneum1,3,4.
Accessories
Therapeutic ultrasound endoscope, which is a curvilinear array ultrasound gastrovideoscope, with a large diameter instrument channel, forceps elevators and Doppler (GF-UCT 180, Olympus America, Melville; NY, USA).
X-ray machines.
Electrosurgical unit.
0.025-inch, 450-cm-long guide wire (VisiGlide®, Olympus Medical Systems; Tokyo, Japan).
Injection needle catheter (endoscopic retrograde cholangiopancreatography $#91;ERCP] catheter, MTW Endoskopie; Düsseldorf, Germany).
15 mm X 10 mm lumen-apposing metal stent (LAMS) (HOT AXIOS stent, Xlumena Inc.; Mountain View, CA, USA).
Case report
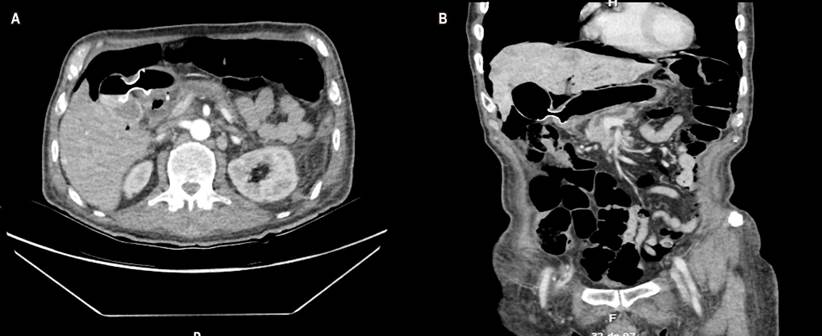
A 69-year-old male patient with a history of inoperable metastatic pancreatic neuroendocrine tumor and who had experienced abdominal pain, hyporexia, jaundice, and choluria for 15 days was admitted to the institution. A cholangioronance was performed in which a 5 cm mass in the head of the pancreas blocking the bile duct was observed. A dilated cystic duct was also identified (Figure 1).
The patient was taken to endoscopic retrograde cholangiopancreatography (ERCP), which could not be performed due to duodenal stenosis of neoplastic origin. Choledoduodenostomy or the use of a duodenal stent were not possible either due to neoplastic invasion of the duodenal bulb.
An EUS-guided cholecystogastrostomy was performed at the gastric antrum (Video 1).
Video 1. EUS-guided cholecystogastrostomy.
In addition, a 15 mm × 10 mm LAMS (HOT AXIOS stent, Xlumena Inc.; Mountain View, CA, USA) was used (Figures 2 and 3). The patient had no complications but was hospitalized for cancer treatment.
Technique
The procedure was started using a therapeutic linear echoendoscope because inflammation in the distal gastric antrum, pylorus, or duodenum is not uncommon. It was necessary to find the most stable position to place the tip of the echoendoscope in front of the gallbladder, in the prepyloric region. The wall between the intestinal lumen and the gallbladder was examined to measure its thickness and the presence of blood vessels with power Doppler.
A 0.025inch x 450cm guide wire (VisiGlide®, Olympus Medical Systems; Tokyo, Japan) was inserted into the gallbladder lumen and confirmed by means of an imaging control study. Cholecystogastrostomy was performed using a 15 mm × 10 mm LAMS (HOT AXIOS stent, Xlumena Inc.; Mountain View, CA, USA), without any complication and achieving active biliary drainage in the gastric lumen. The patient was hospitalized for cancer treatment1,5,6.
Discussion
Percutaneous cholecystostomy is the most common approach to malignant bile and duodenal obstructions in patients of advanced age, in those with a high and permanent risk of surgery, or who have an inoperable oncological disease and limited life expectancy. However, percutaneous biliary drainage catheter connected to a bag may cause infection at the puncture site. Since this procedure is associated with disfigurement and discomfort, usually affecting the patient’s quality of life, special care is needed, including irrigation and changes of dressings, bags, and catheters.
Similarly, significant complications may occur when performing percutaneous cholecystostomy, including tube separation. In addition, the procedure needs to be repeated in cases of intrahepatic bleeding and sepsis7-9.
On the other hand, percutaneous transhepatic biliary drainage (PTBD) is an alternative management approach with technical response rates of 56-100% and complications rates of up to 14.5%. PTBD is associated with bleeding, pneumothorax, pneumoperitoneum, bile leaks, or catheter migration. EUS-guided transmural gallbladder drainage (EUS-GBD) is another endoscopic alternative.
In retrospective studies, EUS-GBD can be performed and is comparable to PTBD in terms of technical feasibility, safety, and efficacy, with complication rates of 11-38%. The transgastric approach has been associated with higher rates of bile leaks and distal stent migration as a result of the distance between the gallbladder and the gastric wall. The main disadvantages of placing a plastic stent are small diameter and the risk of bile leak into the peritoneal space, but this problem may be solved using the HOT AXIS stent (Xlumena Inc.; Mountain View, CA, USA).
A fully covered lumen-apposing metal stent can cover the space between the stent and the fistula, preventing bile leaks, while promoting better drainage, as reported by Widmer et al., who used fully covered metal stents with anti-migratory anchoring fins (Gore VIABIL®, Gore; Utica, NY, USA)8-11.
EUS-guided transluminal drainage methods are gaining acceptance as an effective management approach to a variety of conditions such as pseudocyst drainage, abscess drainage, pancreaticogastrostomy, and hepaticogastrostomy. In turn, EUS-guided biliary drainage is an option for biliary decompression. It is divided into ultrasound-guided choledoduodenostomy for extrahepatic bile duct drainage and hepato-gastrostomy for intrahepatic bile duct drainage.
In our case, EUS-guided choledoduodenostomy could not be performed due to duodenal invasion. Furthermore, magnetic resonance cholangiopancreatography showed that the gallbladder was distended (Courvoisier-Terrier sign) and communicated well with the extrahepatic bile duct. Therefore, EUS-guided cholecystogastrostomy was chosen instead of EUS-guided hepaticogastrostomy9,12-14.
Kwan et al., along with the Lee et al. and Baron et al., reported that EUS-guided cholecystogastrostomy was successfully performed in 13 patients. All of them showed rapid clinical improvement and had only minor complications without clinical significance: an intraprocedural biliary leak and a pneumoperitoneum.
On the other hand, EUS-guided gallbladder drainage using pigtail plastic stents is associated with bile leaks, as reported by Itoi et al. in 2011. Likewise, Súbtil et al. reported the migration of the stent into the gallbladder in a one-step procedure, so the procedure cannot be safely recommended. However, devices such as the HOT AXIOS stent (Xlumena Inc.; Mountain View, CA, USA) allow safe and effective EUS-guided therapeutic drainage.
In the case reported here, no bile or gastric content leaks after stent deployment were observed, although the gallbladder and stomach did not adhere to each other since the HOT AXIOS stent (Xlumena Inc.; Mountain View, CA, USA) made a lumen-to-lumen apposition provided by the flanges and created an airtight seal for the whole silicone cover, avoiding the need for tissue fulguration for adequate inflammatory adhesion between the gallbladder and the gastric duct.
As described by Itoi et al., these results show that gallbladder drainage, including EUS-guided cholecystogastrostomy, is an alternative procedure for bile duct drainage, only if the cystic duct is above the obstruction and both the bile duct and the gallbladder are well communicated11-16.
In 2013, Itoi et al. proposed that EUS-guided cholecystogastrostomy for bile duct decompression is indicated in the following situations: 1) distal biliary obstruction; 2) the cystic duct takes off above the strictures and the bile duct and gallbladder communicate well with each other; 3) duodenal obstruction that requires a duodenal stent, and 4) inappropriate EUS-guided hepaticogastrostomy as a result of a non-dilated intrahepatic bile duct and/or acute angulation of needle puncture for the placement of the metal stent.
This procedure can be performed in developing countries when appropriate training and implements are available. However, an important question to be answered is when the stent can be removed. According to the experience reported in the literature, removing them in most cases is not necessary. This was also reported by Itoi et al.1-3,17,18.
Conclusions
EUS-guided cholecystogastrostomy should be considered as a preferred option for biliary decompression and should be combined with percutaneous drainage when a patient has ampullary stenosis, duodenal invasion, and dilated bile ducts.
In addition, this procedure can be performed in developing countries, where appropriate training and implements are available. A LAMS (HOT AXIOS stent, Xlumena Inc.; Mountain View, CA, USA) is also required for EUS-guided cholecystogastrostomy to avoid complications such as biliary leak. Further comparative studies are needed to validate the benefits of this technique.
Acknowledgments
To Professor Marc Giovannini, Head of Endoscopy, Endoscopic Ultrasound and Gastroenterology at the Institut Paoli-Calmettes, for his editorial review of the manuscript.
REFERENCES
1. Itoi T, Binmoeller K, Itokawa F, Umeda J, Tanaka R. Endoscopic ultrasonography-guided cholecystogastrostomy using a lumen-apposing metal stent as an alternative to extrahepatic bile duct drainage in pancreatic cancer with duodenal invasion. Dig Endosc. 2013;25 Suppl 2:137-41. http://doi.org/10.1111/den.12084 [ Links ]
2. Seewald S, Ang TL, Richter H, Teng KY, Zhong Y, Groth S, Omar S, Soehendra N. Long-term results after endoscopic drainage and necrosectomy of symptomatic pancreatic fluid collections. Dig Endosc. 2012;24(1):36-41. http://doi.org/10.1111/j.1443-1661.2011.01162.x [ Links ]
3. Itoi T, Itokawa F, Kurihara T. Endoscopic ultrasonography-guided gallbladder drainage: actual technical presentations and review of the literature (with videos). J Hepatobiliary Pancreat Sci. 2011;18(2):282-286. http://doi.org/10.1007/s00534-010-0310-4 [ Links ]
4. Itoi T, Binmoeller KF, Shah J, Sofuni A, Itokawa F, Kurihara T, Tsuchiya T, Ishii K, Tsuji S, Ikeuchi N, Moriyasu F. Clinical evaluation of a novel lumen-apposing metal stent for endosonography-guided pancreatic pseudocyst and gallbladder drainage (with videos). Gastrointest Endosc. 2012;75(4):870-6. http://doi.org/10.1016/j.gie.2011.10.020 [ Links ]
5. Itoi T, Coelho-Prabhu N, Baron TH. Endoscopic gallbladder drainage for management of acute cholecystitis. Gastrointest Endosc. 2010;71(6):1038-1045. http://doi.org/10.1016/j.gie.2010.01.026 [ Links ]
6. Itoi T, Isayama H, Sofuni A, Itokawa F, Kurihara T, Tsuchiya T, Tsuji S, Ishii K, Ikeuchi N, Tanaka R, Umeda J, Moriyasu F, Kawakami H. Stent selection and tips on placement technique of EUS-guided biliary drainage: transduodenal and transgastric stenting. J Hepatobiliary Pancreat Sci. 2011;18(5):664-72. http://doi.org/10.1007/s00534-011-0410-9 [ Links ]
7. Jang JW, Lee SS, Park DH, Seo DW, Lee SK, Kim MH. Feasibility and safety of EUS-guided transgastric/transduodenal gallbladder drainage with single-step placement of a modified covered self-expandable metal stent in patients unsuitable for cholecystectomy. Gastrointest Endosc. 2011;74(1):176-181. http://doi.org/10.1016/j.gie.2011.03.1120 [ Links ]
8. Súbtil JC, Betes M, Muñoz-Navas M. Gallbladder drainage guided by endoscopic ultrasound. World J Gastrointest Endosc. 2010;2(6):203-209. http://doi.org/10.4253/wjge.v2.i6.203 [ Links ]
9. Widmer J, Alvarez P, Gaidhane M, Paddu N, Umrania H, Sharaiha R, Kahaleh M. Endoscopic ultrasonography-guided cholecystogastrostomy in patients with unresectable pancreatic cancer using anti-migratory metal stents: a new approach. Dig Endosc. 2014;26(4):599-602. http://doi.org/10.1111/den.12163 [ Links ]
10. Bakkaloglu H, Yanar H, Guloglu R, Taviloglu K, Tunca F, Aksoy M, Ertekin C, Poyanli A. Ultrasound guided percutaneous cholecystostomy in high-risk patients for surgical intervention. World J Gastroenterol. 2006;12(44):7179-82. http://doi.org/10.3748/wjg.v12.i44.7179 [ Links ]
11. Kwan V, Eisendrath P, Antaki F, Le Moine O, Devière J. EUS-guided cholecystenterostomy: a new technique (with videos). Gastrointest Endosc. 2007;66(3):582-586. http://doi.org/10.1016/j.gie.2007.02.065 [ Links ]
12. Lee SS, Park DH, Hwang CY, Ahn CS, Lee TY, Seo DW, Lee SK, Kim MW. EUS-guided transmural cholecystostomy as rescue management for acute cholecystitis in elderly or high-risk patients: a prospective feasibility study. Gastrointest Endosc. 2007;66(5):1008-12. http://doi.org/10.1016/j.gie.2007.03.1080 [ Links ]
13. Baron TH, Topazian MD. Endoscopic transduodenal drainage of the gallbladder: implications for endoluminal treatment of gallbladder disease. Gastrointest Endosc. 2007;65(4):735-737. http://doi.org/10.1016/j.gie.2006.07.041 [ Links ]
14. Lopes CV, Pesenti C, Bories E, Caillol F, Giovannini M. Endoscopic-ultrasound-guided endoscopic transmural drainage of pancreatic pseudocysts and abscesses. Scand J Gastroenterol. 2007;42(4):524-529. http://doi.org/10.1080/00365520601065093 [ Links ]
15. Seewald S, Ang TL, Teng KY, Groth S, Zhong Y, Richter H, Imazu H, Omar S, Polese L, Seitz U, Bertschinger P, Altorfer J, Soehendra N. Endoscopic ultrasound-guided drainage of abdominal abscesses and infected necrosis. Endoscopy. 2009;41(2):166-74. http://doi.org/10.1055/s-0028-1119501 [ Links ]
16. Seewald S, Imazu H, Omar S, Groth S, Seitz U, Brand B, Zhong Y, Sikka S, Thonke F, Soehendra N. EUS-guided drainage of hepatic abscess. Gastrointest Endosc. 2005;61(3):495-8. http://doi.org/10.1016/s0016-5107(04)02848-2 [ Links ]
17. Itoi T, Sofuni A, Itokawa F, Tsuchiya T, Kurihara T, Ishii K, Tsuji S, Ikeuchi N, Umeda J, Moriyasu F, Tsuchida A. Endoscopic ultrasonography-guided biliary drainage. J Hepatobiliary Pancreat Sci. 2010;17(5):611-6. http://doi.org/10.1007/s00534-009-0196-1 [ Links ]
18. Varadarajulu S, Drelichman ER. EUS-guided drainage of pelvic abscess (with video). Gastrointest Endosc. 2007;66(2):372-376. http://doi.org/10.1016/j.gie.2007.02.054 [ Links ]
Citation: Pinto R, Solano J, Cabrera LF, Benito E. Endoscopic ultrasonography-guided cholecystogastrostomy in a patient with pancreatic cancer: the first case in Colombia (with video). Rev Colomb Gastroenterol. 2020;35(4):527-532. https://doi.org/10.22516/25007440.400
Received: May 03, 2019; Accepted: August 20, 2019











 texto en
texto en