Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista colombiana de Gastroenterología
Print version ISSN 0120-9957On-line version ISSN 2500-7440
Rev. colomb. Gastroenterol. vol.35 no.4 Bogotá Oct./Dec. 2020 Epub July 12, 2021
https://doi.org/10.22516/25007440.410
Case report
Endoscopic ultrasound for the diagnosis of biliary ascariasis: case report and literature review
1Gastroenterólogo clínico quirúrgico. Profesor asociado, Universidad Surcolombiana; Neiva, Colombia.
2Especialista en Epidemiología Clínica. Cirujano General, Epidemiologo Universidad Surcolombiana. Hospital Universitario Hernando Moncaleano Perdomo; Neiva. Colombia.
3Médico General Universidad del Rosario; Bogotá, Colombia.
The following is a case of biliary ascariasis (BA), whose clinical presentation was obstructive jaundice, accompanied by abdominal pain due to acute pancreatitis. At first, clinical suspicion led to consider a stone etiology, for which diagnostic imaging studies were performed, evidencing BA as an incidental finding diagnosed by endoscopic biliopancreatic ultrasonography (EBU), which was confirmed and treated using endoscopic retrograde cholangiopancreatography (ERCP).
Keywords: Biliary ascariasis; Obstructive jaundice; Abdominal pain; Acute pancreatitis; Lithiasic etiology
Se presenta un caso de áscaris de la vía biliar (AB), cuya manifestación clínica fue ictericia obstructiva, acompañada de dolor abdominal causado por un cuadro de pancreatitis aguda. Inicialmente, se sospechó de etiología litiásica, por lo cual se realizaron estudios de imágenes diagnósticas y se evidenció la presencia de AB como hallazgo incidental, diagnosticado por ultrasonografía endoscópica biliopancreática (UEB), que fue confirmado y tratado mediante colangiopancreatografía retrógrada endoscópica (CPRE).
Palabras clave: Áscaris de la vía biliar; ictericia obstructiva; dolor abdominal; pancreatitis aguda; etiología litiásica
Introduction
Ascariasis is a common helminthic disease of the human gastrointestinal tract caused by the parasitic worm Ascaris lumbricoides (AL) that primarily affects developing tropical countries. Adult AL usually inhabit the intestinal lumen without causing any significant symptoms or health problems. Occasionally, adult worms can migrate to the biliary tract through the ampulla of Vater, causing symptoms similar to those of choledocholithiasis, or to the pancreatic duct, causing symptoms similar to the ones observed in pancreatitis cases.
Clinical case
A 47-year-old male from Leticia (Amazonas, Colombia) was referred due to experiencing severe (burning sensation) abdominal pain (8/10) in epigastrium and right hypocondrium, spasms, multiple emetic episodes of biliary characteristics and the presence of choluria for 2 weeks.
As a result, the patient was referred to a secondary care center, where he was diagnosed with hyperamylasemia (595 mg/dL) associated with hyperbilirubinemia (Table 1). Furthermore, positive acute phase reactants and imaging findings, using an enhanced computed tomography (CT) scan, were compatible with acute pancreatitis (Balthazar grade D) (Figure 1), which was classified as moderate to severe according to the clinical severity index, with an APACHE II (Acute Physiology and Chronic Health Evaluation II) score of 7. Consequently, management was initiated with fluid resuscitation, antibiotic treatment with ampicillin/sulbactam, and cessation of feeding.
Table 1 Patient’s lab tests results on admission and at discharge
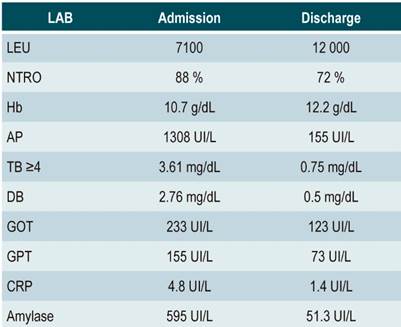
LAB: lab test; LEU: leukocytes; NTRO: neutrophils; Hb: hemoglobin; AP: alkaline phosphatase; TB: total bilirubin; BD: direct bilirubin; GOT: glutamic oxaloacetic transaminase; GPT: glutamic pyruvic transaminase; CRP: C-reactive protein; IU: international unit.
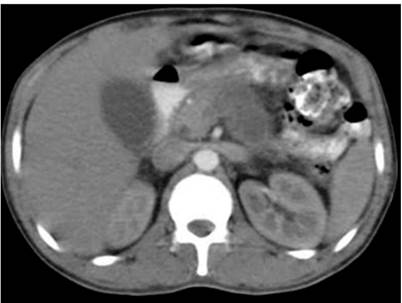
Figure 1 Abdominal CT scan: hepatomegaly and fat infiltration, pancreatitis (Balthazar D) with severity index score of 5, bilateral pleural effusion, and small amount of free fluid in the abdominal cavity. Source: Own elaboration.
An abdominal ultrasound was performed as a complementary study, revealing a gallbladder polyp and biliary sludge without alterations of the bile duct. Endoscopic ultrasonography was performed due to the intermediate risk of choledocholithiasis associated with an increase in bilirubin levels, alteration of the liver panel, clinical symptoms of biliary pancreatitis (Table 1), and greater sensitivity for microlithiasis. Imaging manifestations of cholelithiasis were observed, which were consistent with AL in the choledochal lumen, with an elongated hyperechogenic tubular structure that did not produce acoustic shadowing and railway track sign (Figure 2). Albendazole treatment was prescribed (400 mg orally, every 24 h for 3 days) and an ERCP was performed, along with papillotomy and removal of ascaris from the biliary tract. There were no postoperative complications (Figure 3).
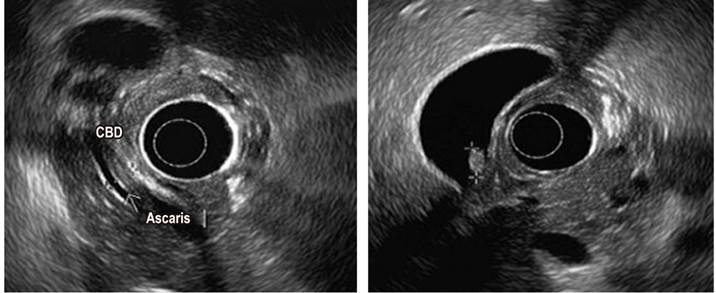
Figure 2 Pancreatobiliary endoscopic ultrasonography: cholelithiasis, biliary ascariasis. CBD: Common bile duct. Source: Own elaboration.
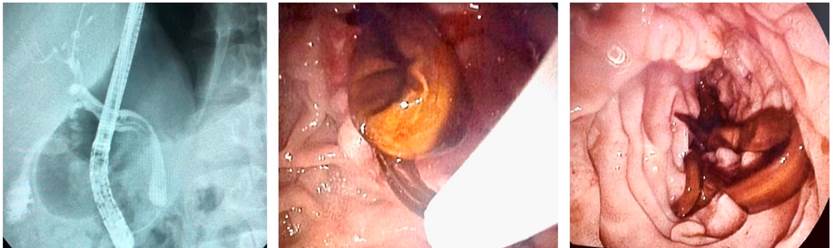
Figure 3 ERCP: biliary route slightly dilated from 7 to 8 mm, with delayed filling defect and railway track sign due to the presence of ascaris. Source: Own elaboration.
During his hospitalization, the patient’s condition improved, and complete remission of acute pancreatitis was achieved. Afterwards, he was referred to undergo laparoscopic cholecystectomy due to the cholelithiasis diagnosis made through endoscopic ultrasonography, and no complications were reported.
Discussion
Obstructive jaundice has several causes of both malignant and benign origin. One of them, which is also rare and difficult to diagnose, is obstruction of the common bile duct (CBD) due to AL infection, a nematode that parasitizes humans and can be between 10 and 30 cm in length1.
In general, about 30% of patients with AL in the CBD have undergone cholecystectomy. It has been concluded that this causes a dilatation of the CBD, which is associated with an increase in cholecystokinin production, resulting in the relaxation of the sphincter of Oddi and, this way, facilitating the migration of the parasite to the CBC2.
Epidemiology
Biliary ascariasis (BA) cases have been reported all over the world, particularly in tropical and subtropical regions (Africa, the Far East, Latin America, Southeast Asia, and some parts of the Middle East)3, where soil and climatic conditions favor the proliferation of intestinal worm larvae. BA accounts for 10-19% of ER admissions related to AL.
There is no reliable data on its incidence. However, an incidence rate ranging from 11% to 19% has been reported in patients with some CBC complications.
Clinical presentation
Biliary presentation
Endemic areas, associated with patients with risk factors for this condition, facilitate the diagnosis of BA. Some of the symptoms include nausea, vomiting, stomach pain, jaundice, and hives. Biliary colic of intensity >8-10 (VAS pain scale), associated with acalculous cholecystitis, occurs in 56-98% of cases.
The formation of gallstones in the CBC is another complication associated with BA. Cholangitis may occur in about 20 % of these patients4.
There is no clear relationship between BA and the risk of developing cholangiocarcinoma. Some papers, however, identify this malignant tumor as a risk factor to be considered.
Non-biliary presentation
Another form of presentation is ascaris-induced acute pancreatitis, which occurs after the parasite invades the lumen of the main pancreatic duct or the sphincter of Oddi (4-30 % of cases).
A non-systemic inflammatory response secondary to the development of intrahepatic abscesses can also occur as a result of a large number of worms in the liver. This situation occurs in 1 % of the cases5.
Diagnosis
With regard to laboratory tests, both leukocytosis associated with an increase in total eosinophil count, and a nonspecific increase in liver function tests levels may be found. However, alkaline phosphatase is a better indicator since it shows an early and progressive increase6 and may even be associated with hyperamylasemia, as it happened in the case reported here.
Some immunological tests do not confirm the diagnosis of BA (poor sensitivity and specificity) and are only useful for confirming exposure to the parasite.
Hepatobiliary ultrasound is a useful tool for an initial diagnostic approach, with the typical railway track sign (CBC with anechoic chamber inside). However, its sensitivity ranges from 25 to 86 %7 and decreases when cholelithiasis and pancreatitis are included, as well as when the study is carried out during the worm’s migratory phase to the outside of the CBC.
Magnetic resonance cholangiopancreatography has a performance of less than 50 % in these cases due to inadequate delimitation at the CBC lumen. However, in the T2 sequence, the parasite can be visualized as a hypointense structure, with a hyperintense CBC signal around it8.
On the other hand, several studies recommend the diagnostic and therapeutic use of ERCP because it achieves sensitivity rates higher than 80 %. In spite of this, in recent years, due to the risk of postoperative complications associated with this procedure (pancreatitis, bleeding, intestinal perforation), several authors have instead proposed the use of endoscopic ultrasonography as an efficient test for the diagnosis of BA. In fact, endoscopic ultrasonography has demonstrated a sensitivity close to 100% when used together with ERCP8,9.
In this regard, a hepatobiliary ultrasound was initially performed in the case reported here, but it did not provide conclusive evidence about the characteristics of the bile duct. Because of the intermediate risk of choledocholithiasis10, an endoscopic ultrasonography was performed, which revealed that the BA had been successfully treated through ERCP.
Conclusions
Biliopancreatic endoscopic ultrasonography is a useful diagnostic tool, with high sensitivity and specificity rates to detect CBC diseases. Interventions associated with morbidity must be avoided in cases of suspected biliary obstruction of unknown etiology, while biliopancreatic endoscopic ultrasonography is the diagnostic tool of preference if there are symptoms of BA.
Since combined use of ERCP and anthelmintics is an efficient therapy, it is considered the first-line treatment of BA
REFERENCES
1. Greenstein AJ, Sachar DB, Gibas A, Schrag D, Heimann T, Janowitz HD, Aufses AH Jr. Outcome of toxic dilatation in ulcerative and Crohn’s colitis. J Clin Gastroenterol. 1985;7(2):137-43. http://doi.org/10.1097/00004836-198504000-00007 [ Links ]
2. Gupta R, Agarwal DK, Choudhuri GD, Saraswat VA, Baijal SS. Biliary ascariasis complicating endoscopic sphincterotomy for choledocholithiasis in India. J Gastroenterol Hepatol. 1998;13(10):1072-1073. http://doi.org/10.1111/j.1440-1746.1998.tb00573.x [ Links ]
3. Leung JW, Chung SC. Endoscopic management of biliary ascariasis. Gastrointest Endosc. 1988;34(4):318-20. http://doi.org/10.1016/s0016-5107(88)71364-4 [ Links ]
4. Kamiya T, Morishita T, Reredo R, Marancenbaum C, Montaño C. Duodenoscopic Management in Biliary Ascariasis. Dig Endosc. 1993;5(2):179-182. http://doi.org/10.1111/j.1443-1661.1993.tb00614.x [ Links ]
5. Pawlowski ZS. Ascariasis. En: Warren KS, Mahmoud AA. Tropical and geographical medicine. Nueva York: Mc Graw-Hill, 2ª edición; 1990. p. 369-378. [ Links ]
6. Khuroo MS, Zargar SA, Mahajan R. Hepatobiliary and pancreatic ascariasis in India. Lancet. 1990;335(8704):1503-1506. http://doi.org/10.1016/0140-6736(90)93037-p [ Links ]
7. Khuroo MS, Zargar SA, Mahajan R, Bhat RL, Javid G. Sonographic appearances in biliary ascariasis. Gastroenterology. 1987;93(2):267-272. http://doi.org/10.1016/0016-5085(87)91013-4 [ Links ]
8. Nasa M, Patil G, Sharma ZD, Puri R. Biliary Ascariasis Mimicking as Choledocholithiasis on Endoscopic Ultrasound. J Assoc Physicians India. 2019;67(1):81-82. [ Links ]
9. Sandouk F, Haffar S, Zada MM, Graham DY, Anand BS. Pancreatic-biliary ascariasis: experience of 300 cases. Am J Gastroenterol. 1997;92(12):2264-2267. [ Links ]
10. Aleknaite A, Simutis G, Stanaitis J, Valantinas J, Strupas K. Risk assessment of choledocholithiasis prior to laparoscopic cholecystectomy and its management options. United European Gastroenterol J. 2018;6(3):428-438. http://doi.org/10.1177/2050640617731262 [ Links ]
Citation: Polanía-Liscano HA, Jiménez-Sánchez HC, Polanía-Galindo DJ. Endoscopic ultrasound for the diagnosis of biliary ascariasis: case report and literature review. Rev Colomb Gastroenterol. 2020;35(4):537-541. https://doi.org/10.22516/25007440.410
Received: May 19, 2019; Accepted: August 15, 2019











 text in
text in 



