Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista colombiana de Gastroenterología
Print version ISSN 0120-9957On-line version ISSN 2500-7440
Rev. colomb. Gastroenterol. vol.35 no.4 Bogotá Oct./Dec. 2020 Epub July 12, 2021
https://doi.org/10.22516/25007440.429
Case report
Pulmonary cryptococcosis in a patient with ulcerative colitis treated with prednisolone and azathioprine
1Clínica Universitaria Colombia; Bogotá, Colombia.
2Seattle VA, Hospital Universitario de Washington; Seattle, Estados Unidos.
Inflammatory bowel disease comprises Crohn’s disease (CD) and ulcerative colitis (UC), the latter being a chronic disease characterized by diffuse inflammation of the colonic mucosa that affects the rectum and extends proximally. Its clinical course is intermittent with exacerbations and remissions and its treatment is generally pharmacological, with steroids, immunomodulators, and anti-tumor necrosis factor inhibitors (TNF), which cause the patient to be in a state of immunosuppression associated, in some cases, with opportunistic infections. The literature describes the occurrence of pulmonary cryptococcosis in patients with human immunodeficiency virus (HIV) infection, in cases associated with drug treatment of patients with CD, as well as with other opportunistic infections such as tuberculosis and herpes. This is one of the first cases of pulmonary cryptococcosis reported in a patient diagnosed with ulcerative colitis, who received step therapy with salicylates, immunomodulators, and biological therapy. The infection was documented clinically, radiologically, and histologically. The patient received the appropriate treatment and had a satisfactory evolution.
Keywords: Inflammatory bowel disease; Ulcerative colitis; Immunosuppression; Opportunistic infections; Pulmonary cryptococcosis
La enfermedad inflamatoria intestinal comprende la enfermedad de Crohn (EC) y la colitis ulcerativa (CU). Esta última es una patología crónica caracterizada por una inflamación difusa de la mucosa colónica, que afecta el recto y se extiende de forma proximal. Su curso clínico es intermitente, con exacerbaciones y remisiones. Su tratamiento, por lo general, es farmacológico, con corticoides, inmunomoduladores e inhibidor del factor de necrosis tumoral (anti tumor necrosis factor, TNF), los cuales causan un estado de inmunosupresión en el paciente, que puede asociarse en algunos casos a infecciones oportunistas. En la literatura se describe la aparición de la criptococosis pulmonar en pacientes con infección por el virus de inmunodeficiencia humana (VIH). En otros casos se asocia al tratamiento farmacológico de pacientes con EC, así como con otras infecciones oportunistas, tales como la tuberculosis y el herpes. Presentamos uno de los primeros casos de criptococosis pulmonar en un paciente con diagnóstico de colitis ulcerativa, quien recibió tratamiento escalonado con salicilatos, inmunomoduladores y terapia biológica. La infección fue documentada clínica, radiológica e histológicamente. El paciente recibió el tratamiento adecuado y presentó una evolución satisfactoria.
Palabras clave: Enfermedad inflamatoria intestinal; colitis ulcerativa; inmunosupresión; infecciones oportunistas; criptococosis pulmonar
Introduction
Ulcerative colitis (UC) is a chronic disease characterized by diffuse inflammation of the colonic mucosa that affects the rectum and proximally extends in a variable, symmetrical and circumferential manner throughout the colon. Its cardinal symptom is bloody diarrhea associated with fecal urgency and rectal tenesmus, and its clinical course is intermittent, with exacerbations and remissions1. Initial treatment is usually pharmacological, and surgery may be performed in only a few cases. The use of some drugs, such as corticosteroids, immunomodulators and antitumor necrosis factor (TNF) causes immunosuppression, which in some cases may be associated with opportunistic infections2.
The following is the case of a male patient diagnosed with UC, who received escalation therapy with salicylates, immunomodulators and biological therapy, without achieving adequate control of the disease. As a result, the patient was taken to surgery and had a successful postoperative recovery. However, during treatment, he presented with pulmonary cryptococcosis that was studied clinically, radiologically, and histologically, and appropriate treatment was provided, achieving a satisfactory response.
Clinical case
A 48-year-old male consulted in November 2011 due to an 8-month history of diarrhea with mucus and blood as well as a 10-kg weight loss; no other relevant symptoms were informed by the patient. On physical examination, mild tenderness over the colonic area was reported. A colonoscopy was performed, finding extensive colitis, and biopsies, which later confirmed the diagnosis of UC, were performed; thus, treatment with mesalazine 3 g/P.O./day and a corticosteroid cycle (prednisolone) of 40 m/P.O./day was started, achieving clinical improvement. The patient was discharged with a permanent prescription of mesalazine, as well as corticosteroids use, with a gradual decrease in their dose until suspension.
Three months later, and after an early and voluntary suspension of both drugs, the patient had a relapse. A colonoscopy revealed ulcerative pancolitis with a Mayo severity score of 2 and E3 S2 severity degree according to the Montreal classification. Mesalazine was restarted at 3 g/P.O./day, achieving symptoms resolution.
However, in October 2013, the patient had a new relapse. A stool test showed amebiasis, which was treated with metronidazole plus nifuroxazide every 12 hours, for 7 days, without any improvement. Therefore, considering the reactivation of the disease, azathioprine 150 g/P.O./day (2.5 mg/kg/day) was added to the prescription of mesalazine, achieving adequate remission.
The patient consulted again in November 2014 due to bloody diarrhea, malaise, asthenia and adynamia, and weight loss of 4 kg. He was taking mesalazine 3 g/P.O./day and azathioprine 50 mg/P.O./day (2.5 mg/kg/day). The patient was diagnosed with anemic heart disease, lower gastrointestinal tract bleeding and active steroid-dependent UC, with a Montreal classification S3 severity. Corticosteroid pulse treatment was initiated (prednisolone 40 mg/day). Moreover, 2 units of packed red blood cells and iron sucrose were transfused.
During an endoscopic check-up, ulcerative pancolitis and pseudopolyps were found, which, compared with the previous colonoscopy, showed a progression of the disease, thus the initiation of biological therapy was considered. Tests for tuberculin (purified protein derivative, PPD), hepatitis A, B, and C, and HIV were performed. A chest x-ray was also done, revealing a nodule in the left upper lobe and a nodule in the lower lobe, 6 mm each (Figure 1). A computed tomography of the chest confirmed these findings (Figure 2).
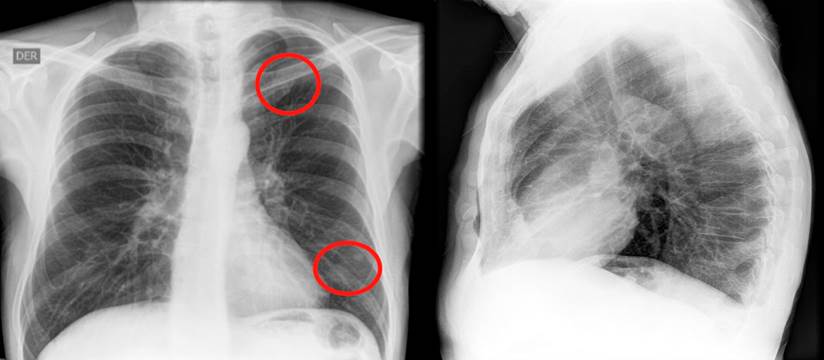
Figure 1 Nodular opacification with soft tissue density in the upper and lower left lobes on the chest x-ray. Source: Own elaboration.
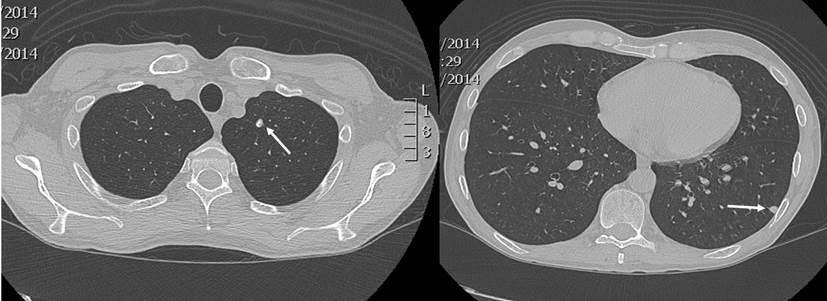
Figure 2 A pulmonary nodule with thick calcifications of 6 mm in diameter was observed in the left upper lobe apicoposterior segment, as well as another subpleural nodular image of 6 mm in diameter in the left lower lobe apical segment with soft tissue density. Source: Own elaboration.
Suspecting tuberculous granuloma, a wedge biopsy of the lower lobe nodule was performed. The pathology report showed lung parenchyma with chronic caseating granulomatous disease, compatible with cryptococcosis, and negative for acid-fast bacilli (AFB) (Figure 3). Fungal cultures confirmed a moderate growth of Cryptococcus neoformans, while negative PPD allowed ruling out latent tuberculosis.
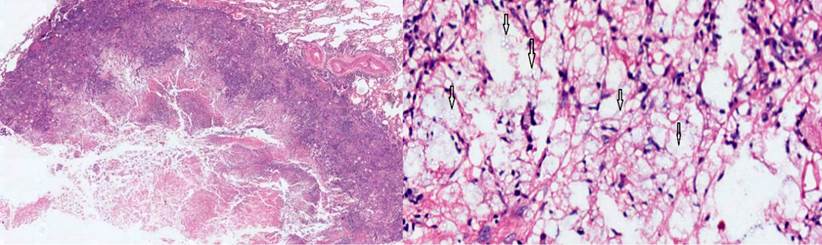
Figura 3 Using hematoxylin-eosin stain, a necrotizing granuloma with debris and histiocytes was observed in the lung parenchyma. Higher magnification (10 X) made it possible to appreciate in detail the cryptococcus spores, indicated with arrows. Source: Own elaboration.
Considering the diagnosis of pulmonary cryptococcosis without systemic involvement, the infectious disease service started treatment with fluconazole at 400 mg/P.O./day and contraindicated biologic therapy for at least the first eight weeks of fluconazole treatment. Furthermore, a monthly serum cryptolatex test was indicated during the first year, obtaining negative results.
Two months after starting treatment with fluconazole, adalimumab was added to the mesalazine and azathioprine treatment scheme. Initially, the patient had an adequate response, but after eight months, he was readmitted due to a new relapse. Reactivation of UC was then considered based on the disease progression (S3 type according to the Montreal severity scale) and the presence of severe colitis as measured with the Truelove and Witts severity index.
However, given the inadequate response to adalimumab, treatment with infliximab was started, achieving an initial improvement of symptoms. However, he had another relapse in October 2015, which was considered a failed response to biological treatment, so surgical treatment was decided.
Thus, total proctocolectomy, J-pouch surgery, ileoanal anastomosis, and protective ileostomy were performed. The ileostomy was closed during a second operation in February 2016. Currently, the patient is asymptomatic, has a good quality of life and does not require medication.
Discussion
In recent decades, the incidence of opportunistic infections, such as tuberculosis and cryptococcosis, has increased especially due to the emergence of diseases such as acquired immunodeficiency syndrome (AIDS), where cryptococcosis can occur in 5 to 10% of cases. These opportunistic infections have also been reported in patients undergoing immunosuppression following organ transplantation, in those with inflammatory diseases, and even in immunocompetent persons. It has been estimated that up to one million new cases of cryptococcosis are diagnosed worldwide, with about 650 000 deaths each year3,4.
Pulmonary cryptococcosis is caused by an encapsulated yeast that is acquired after inhaling spores from the environment5. There are several species, but the most common is neoformans, which can be found anywhere in the world; the gattii species is found in tropical and subtropical regions6.
In most cases, it is possible to establish exposure to pigeon, poultry, dog and cat droppings, or other environmental spores. However, the source of infection is not identified in up to 15 % of cases7. In our patient, exposure was not determined.
Patients may experience mild symptoms, such as headaches, coughs, and fevers, or systemic involvement manifested by chills, hemoptysis, and weight loss. Although the percentage may vary, according to several publications, individuals may be asymptomatic in 17-35% of cases. Diagnosis is often made incidentally through imaging findings of pulmonary nodules, which can be solitary or multiple, as well as of areas of consolidation or reticulonodular pattern8,9.
Our patient had no cryptococcosis-related symptoms. Therefore, diagnosis was incidental and based on the initial finding of pulmonary nodules, which were later confirmed through CT scan. This technique is one of the available diagnostic methods, and it usually shows few or multiple subpleural nodules or masses with or without halo. In addition, in a smaller number of cases, consolidation, pleural effusions, or an increase in the size of mediastinal nodes may be observed10,11.
Other diagnostic techniques, such as the serum measurement of capsular antigen, are also used. This technique has the advantage of being non-invasive, although false negative and positive results have been reported, so it is necessary to be cautious when using it7. Currently, molecular biology tests are also used, which have the advantage of being fast but take more time for proper assessment.
The diagnostic tools considered to be the most specific are culture and tissue biopsy; the latter is the most important and can be collected through puncture or surgically; also, Chinese ink, Gomory, periodic acid-Schiff (PAS) and mucicarmine are the stains used12. In the case of our patient, culture and biopsy were performed, both confirming the presence of the cryptococcal spores.
Treatment of cryptococcosis in immunocompromised patients with fluconazole was introduced in the 1990s, achieving a marked decrease in the presence of this disease13. Currently, in mild or moderate lung infections, treatment with fluconazole (400 m/day) is prescribed for 6-12 months, as it was the case of our patient.
On the other hand, in severe infections cases or when the central nervous system is involved, induction therapy with liposomal amphotericin B (3-4 mg/kg/day IV) or amphotericin B lipid complex (5 mg/kg/day, IV) is used for 2 weeks, followed by the administration of fluconazole (400 mg/day) for 8 weeks14,15.
Recently, resistance to fluconazole has been observed, especially in eastern countries. According to various reports, this resistance increased from 5.1 % to 22.6 % over a period of 7 years due to the excessive use of fluconazole for prophylaxis in immunocompromised patients or its administration in primary or maintenance treatments16.
Few cases of patients with inflammatory bowel disease and cryptococcosis have been reported. However, in all those cases, it has been associated with the administration of anti TNFα agents, whereas in most scenarios, it has been associated in patients with celiac disease17. So far, no cases of cryptococcosis have been reported in people with UC treated with corticosteroids and azathioprine.
Conclusions
To the best of our knowledge, this is the first case reported in the literature of a patient with UC treated with corticosteroids and azathioprine. The patient had pulmonary cryptococcosis, which is an opportunistic disease that particularly affects people with AIDS. However, it has also been observed in transplanted patients and in those who have undergone treatment for inflammatory diseases. Since these patients are considered immunocompromised and cryptococcal infection could be asymptomatic in them, further studies should be carried out prior to starting biologic therapy.
REFERENCES
1. Hani AC, Galiano MT, Albis R, Márquez JR, Juliao F. Consenso Colombiano de Enfermedad Inflamatoria Intestinal. Rev Col Gastroenterol. 2012;27(Supl. 1):S1-S44. [ Links ]
2. Chen LP, Li J, Huang MF, Chen QS, Xia B. Cryptococcus neoformans infection in ulcerative colitis with immunosuppressants. Inflamm Bowel Dis. 2011;17(9):2023-4. http://doi.org/10.1002/ibd.21619 [ Links ]
3. Pappas PG. Cryptococcal infections in non-HIV-infected patients. Trans Am Clin Climatol Assoc. 2013;124:61-79. [ Links ]
4. Ye F, Xie JX, Zeng QS, Chen GQ, Zhong SQ, Zhong NS. Retrospective analysis of 76 immunocompetent patients with primary pulmonary cryptococcosis. Lung. 2012;190(3):339-46. http://doi.org/10.1007/s00408-011-9362-8 [ Links ]
5. Goldman DL, Khine H, Abadi J, Lindenberg DJ, Pirofski La, Niang R, Casadevall A. Serologic evidence for Cryptococcus neoformans infection in early childhood. Pediatrics. 2001;107(5):E66. http://doi.org/10.1542/peds.107.5.e66 [ Links ]
6. Baddley JW, Dismukes WE. Cryptococcosis. En: Kauffman CA, Pappas PG, Sobel JD, Dismukes WE. Essentials of Clinical Mycology. Nueva York: Springer; 2011. p. 207-226. [ Links ]
7. Zhang Y, Li N, Zhang Y, Li H, Chen X, Wang S, Zhang X, Zhang R, Xu J, Shi J, Yung RC. Clinical analysis of 76 patients pathologically diagnosed with pulmonary cryptococcosis. Eur Respir J. 2012;40(5):1191-200. http://doi.org/10.1183/09031936.00168011 [ Links ]
8. Suwatanapongched T, Sangsatra W, Boonsarngsuk V, Watcharananan SP, Incharoen P. Clinical and radiologic manifestations of pulmonary cryptococcosis in immunocompetent patients and their outcomes after treatment. Diagn Interv Radiol. 2013;19(6):438-46. http://doi.org/10.5152/dir.2013.13049 [ Links ]
9. Chang YS, Chou KC, Wang PC, Yang HB, Chen CH. Primary pulmonary cryptococcosis presenting as endobronchial tumor with left upper lobe collapse. J Chin Med Assoc. 2005;68(1):33-6. http://doi.org/10.1016/S1726-4901(09)70129-7 [ Links ]
10. Lindell RM, Hartman TE, Nadrous HF, Ryu JH. Pulmonary cryptococcosis: CT findings in immunocompetent patients. Radiology. 2005;236(1):326-331. http://doi.org/10.1148/radiol.2361040460 [ Links ]
11. Yu JQ, Tang KJ, Xu BL, Xie CM, Light RW. Pulmonary cryptococcosis in non-AIDS patients. Braz J Infect Dis. 2012;16(6):531-539. http://doi.org/10.1016/j.bjid.2012.07.004 [ Links ]
12. Singh N, Alexander BD, Lortholary O, Dromer F, Gupta KL, John GT, del Busto R, Klintmalm GB, Somani J, Lyon GM, Pursell K, Stosor V, Muñoz P, Limaye AP, Kalil AC, Pruett TL, Garcia-Diaz J, Humar A, Houston S, House AA, Wray D, Orloff S, Dowdy LA, Fisher RA, Heitman J, Wagener MM, Husain S. Pulmonary cryptococcosis in solid organ transplant recipients: clinical relevance of serum cryptococcal antigen. Clin Infect Dis. 2008;46(2):e12-8. http://doi.org/10.1086/524738 [ Links ]
13. Rohatgi S, Pirofski LA. Host immunity to Cryptococcus neoformans. Future Microbiol. 2015;10(4):565-581. http://doi.org/10.2217/fmb.14.132 [ Links ]
14. Ali T, Kaitha S, Mahmood S, Ftesi A, Stone J, Bronze MS. Clinical use of anti-TNF therapy and increased risk of infections. Drug Healthc Patient Saf. 2013;5:79-99. http://doi.org/10.2147/DHPS.S28801 [ Links ]
15. Zhou Q, Hu B, Shao C, Zhou C, Zhang X, Yang D, Li C. A case report of pulmonary cryptococcosis presenting as endobronchial obstruction. J Thorac Dis. 2013;5(4):E170-3. http://doi.org/10.3978/j.issn.2072-1439.2013.08.40 [ Links ]
16. Pfaller MA, Diekema DJ, Gibbs DL, Newell VA, Bijie H, Dzierzanowska D, Klimko NN, Letscher-Bru V, Lisalova M, Muehlethaler K, Rennison C, Zaidi M; Global Antifungal Surveillance Group. Results from the ARTEMIS DISK Global Antifungal Surveillance Study, 1997 to 2007: 10.5-year analysis of susceptibilities of noncandidal yeast species to fluconazole and voriconazole determined by CLSI standardized disk diffusion testing. J Clin Microbiol. 2009;47(1):117-23. http://doi.org/10.1128/JCM.01747-08 [ Links ]
17. Fraison JB, Guilpain P, Schiffmann A, Veyrac M, Le Moing V, Rispail P, Le Quellec A. Pulmonary cryptococcosis in a patient with Crohn’s disease treated with prednisone, azathioprine and adalimumab: exposure to chicken manure as a source of contamination. J Crohns Colitis. 2013;7(1):e11-4. http://doi.org/10.1016/j.crohns.2012.04.016 [ Links ]
Citation: Prieto-Ortiz R, Reyes G, Carvajal G, Figueredo E. Pulmonary cryptococcosis in a patient with ulcerative colitis treated with prednisolone and azathioprine. Rev Colomb Gastroenterol. 2020;35(4):545-550. https://doi.org/10.22516/25007440.429
Received: July 15, 2019; Accepted: August 13, 2019











 text in
text in 



