Introduction
Chronic pancreatitis (CP) was first described in 1946 by Comfort et al.1; however, its definition, pathogenesis and clinical course are still under discussion2; also, there is no a consensus on the appropriate diagnostic techniques and management approaches3. Since it was first described, different scientific societies have sought to establish a mechanistic and taxonomic definition of CP encompassing risk factors, etiologies, symptoms and pancreatic morphological changes4. The definition of the Japan Pancreas Society4,5, which defines CP as the progressive inflammation, scarring and fibrosis of the pancreas that can lead to the irreversible loss of its endocrine and exocrine function in individuals with genetic, environmental or other types of predisposition, was taken into account4.
The initial clinical characteristics of CP are not specific, but at onset patients can present with dyspepsia in up to 85% of cases, diabetes mellitus (DM) and exocrine pancreatic insufficiency (EPI)6-10. One of the main causes of morbidity and mortality in CP is malabsorption, which leads to vitamin deficiency and metabolic bone disease in advanced stages of EPI6,7,11,12. In addition, a meta-analysis13 found that patients with CP had a risk 13 times higher of developing pancreatic cancer14, while other studies have shown higher mortality rates associated with CP in comparison with the general population15-17.
A patient with clinical manifestations of CP such as chronic abdominal pain, diarrhea or nutritional deficit must be approached by recognizing the possibility of the presence of the disease, performing an anamnesis and a physical examination aimed at detecting associated conditions, and administering risk scales, in order to look for changes in laboratory and images studies suggestive of the disease7,18. Instead of being caused by a single etiology, there are several situations that can lead to the development of CP, including chronic alcohol consumption, smoking, the use of certain medications, metabolic diseases such as hypercalcemia and hypertriglyceridemia, genetic predisposition and personal or family history of anatomical nature disease, lithiasis, and recurrent acute pancreatitis7,19,20.
Besides its clinical presentation, CP diagnosis is made based on morphological and histological changes in the pancreatic parenchyma and the pancreatic ducts7. Biopsy remains the gold standard, however it is an invasive and difficult to perform procedure7,21. Diagnosis is especially important in early stages of the disease in order to avoid its progression to symptomatic and irreversible pancreatic insufficiency, so a great technological progress has been made in terms of imaging studies in search of achieving an earlier diagnosis7,18. Initially, x-rays, where pancreatic calcifications can be observed, were used3,22. Then, ultrasound, endoscopic retrograde cholangiopancreatography (ERCP) and computed tomography (CT) emerged as diagnostic tests, given that these procedures provide a more detailed anatomy of the pancreas21. Currently, magnetic resonance imaging (MRI) and endoscopic ultrasound (EUS) allow detecting early and late changes in both the pancreatic parenchyma and the pancreatic ducts with high sensitivity and specificity for CP23-25.
Current knowledge about the epidemiology and local clinical characteristics of CP in Colombia is incomplete. Reaching a CP diagnosis can take several months or even years due to the long clinical course of the disease, the complexity the follow-up of these patients (especially those with chronic alcohol consumption) implies, and the multiple relapses and remissions typical of this condition26. This is why, currently this disease is underdiagnosed and patients remain outside the scope of gastroenterology. Knowing the epidemiology of a disease in every population is fundamental to establish clinical protocols aimed at achieving early diagnosis, timely provision of care and a reduced disease burden. Taking this into account, the aim of this study was to make a description of the patients with CP treated between 2011 and 2017 in a gastroenterology referral center in southwestern Colombia.
Methodology
A cross-sectional study was conducted based on the search of medical records of adult patients with CP assessed in a gastroenterology outpatient clinic. The medical records of patients with ICD-10 CP diagnosis (K86.0, K86.1, K86.8 and K86.9) treated between January 2011 and December 2017 were reviewed for identifying the individuals to be included in the study. Then, the occurrence of the disease was confirmed by reviewing the clinical and radiological characteristics of eligible patients.
The following patients were included: men and women older than 18 years with chronic abdominal pain, DM or steatorrhea, and radiological findings including gallbladder or bile duct stones, pancreatic parenchymal changes such as atrophy, calcifications, cysts, lobularity, stones, or pancreatic duct dilatation evident on x-rays, ultrasound, CT, MRI, magnetic resonance cholangiopancreatography (MRCP), or EUS. Patients with imaging studies in which a normal pancreas was reported were excluded.
The etiology of CP was established by the treating specialist depending on risk factors and abnormal findings in laboratory and imaging studies.
Stata v.14® (StataCorp. 2015. Stata Statistical Software: Version 14. College Station, TX: StataCorp LP) was used for data analysis. Data distribution in quantitative variables was evaluated by means of the Shapiro-Wilk test, and they were expressed using means or medians with their respective standard deviations (SD) or interquartile ranges, while proportions were used for qualitative variables. Results are shown in frequency tables and bar graphs.
The project was approved by the ethics committee of the Fundación Valle del Lili as stated in Minutes n.° 09 of May 9, 2018. All researchers involved in the study stated they did not have any conflict of interest.
Results
Initially, 97 patients with PC were identified during the study period according to the ICD-10 diagnoses reported in the medical records. However, only 36 met the eligibility criteria and were included for analysis. Absence of the imaging study report in the medical record was the main reason for exclusion.
The demographic characteristics and medical history of the study population are shown in Table 1. Most patients were men (72.2 %) and the mean age was 56 ± 15.1 years. Most patients had a history of hypertension (HTA) (38.9 %), chronic alcohol consumption (25.0 %) and DM (22.2 %). First-degree family history was identified in 3 patients: 2 had PC (5.6%), and 1, pancreatic cancer (2.8%).
Table 1 Demographic characteristics and medical history of patients with PC*
| n (%) | |
|---|---|
| Age** | 56 ± 15.1 |
| Sex | |
| Male | 26 (72.2) |
| Female | 10 (27.8) |
| Personal medical history | |
| DM | 8 (22.2) |
| Insulin therapy | 5 (13.9) |
| HTA | 14 (38.9) |
| Dyslipidemia | 5 (13.9) |
| Chronic alcohol consumption | 9 (25.0) |
| Cigarette consumption | 4 (11.1) |
| Hypercalcemia | 0 |
| Chronic renal failure | 3 (8.3) |
| Acute necrotizing pancreatitis | 2 (5.6) |
| Pancreatic cancer | 1 (2.8) |
| Family history | |
| Pancreatic cancer | 1 (2.8) |
| PC | 2 (5.6) |
*n = 36. **Value expressed in mean (± SD).
Chronic abdominal pain was the most frequent clinical presentation of CP (83.3 %) (Table 2). Other less frequent symptoms included weight loss (30.6 %), chronic diarrhea (27.8 %), and nausea or vomiting (19.4 %). DM was reported in 8 of 36 patients (22.2%).
Table 2 Clinical presentation CP in the study population *
| Symptom | n (%) |
|---|---|
| Chronic abdominal pain | 30 (83.3) |
| Weight loss | 11 (30.6) |
| Chronic diarrhea | 10 (27.8) |
| DM | 8 (22.2) |
| Jaundice | 3 (8.3) |
| Nausea and vomiting | 7 (19.4) |
| Abdominal distension | 5 (13.9) |
| Dyspepsia | 5 (13.9) |
| Constipation | 3 (8.3) |
| Hyporexia | 2 (5.6) |
| Choluria | 1 (2.8) |
*n = 36.
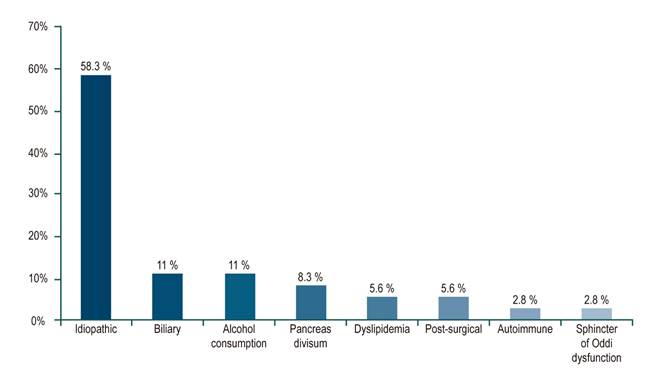
In more than half of patients (58.3 %) CP was idiopathic (Figure 1). Other etiologies that were identified included biliary disease (11.0 %) and chronic alcohol consumption (11.0 %). Regarding imaging studies, a total of 81 were performed in the 36 patients (Table 3). CT, MRI, and MRCP were performed in about two-thirds of the study population (60.5 %) and the main findings were atrophy (53.1 %), calcifications (34.7 %), and pancreatic duct dilatation (49.0 %). EUS was used in 14.8% of patients.
Table 3 Imaging studies used for the diagnosis of CP*
| Study | n (%) |
|---|---|
| Abdominal X-ray | 2 (2.5) |
| Pancreatic calcifications | 2 (100) |
| Abdominal ultrasound | 18 (22.2) |
| Gallstones in the gallbladder or the bile duct | 6 (33.3) |
| Pancreatic atrophy | 4 (22.2) |
| Pancreatic calcifications | 2 (11.1) |
| Pancreatic duct stones | 5 (27.8) |
| Pancreatic duct dilatation | 5 (27.8) |
| MRI or MRCP | 24 (29.6) |
| Gallstones in the bile duct | 4 (16.7) |
| Pancreatic atrophy | 14 (58.3) |
| Pancreatic calcifications | 5 (20.8) |
| Pancreatic duct stones | 8 (33.3) |
| Pancreatic duct dilatation | 14 (58.3) |
| Pancreatic cysts | 3 (12.5) |
| Pancreatic lobularity | 3 (12.5) |
| Abdominal CT scan | 25 (30.9) |
| Pancreatic atrophy | 12 (48.0) |
| Pancreatic calcifications | 12 (48.0) |
| Pancreatic duct stones | 4 (16.0) |
| Pancreatic duct dilatation | 10 (40.0) |
| Pancreatic cysts | 3 (12.0) |
| EUS | 12 (14.8) |
| Gallstones in the gallbladder or the bile duct | 2 (16.7) |
| Pancreatic atrophy | 5 (41.7) |
| Pancreatic calcifications | 8 (66.7) |
| Pancreatic duct stones | 6 (50.0) |
| Pancreatic duct dilatation | 12 (100) |
| Pancreatic cysts | 3 (25.0) |
| Pancreatic lobularity | 6 (50.0) |
| Rosemont criteria in EUS | 12 (14.8) |
| CP diagnosis | 4 (33.3) |
| Suggestive of CP | 7 (58.3) |
| Indeterminate criteria for CP | 1 (8.3) |
*n= 81.
Discussion
CP is a chronic inflammation of the pancreas and, according to certain scientific societies, the presence of pancreatic insufficiency was necessary for its diagnosis, which contributed to the late detection of the disease4,7. For this reason, the inclusion of risk factors and associated conditions with PC as part of its definition has been proposed as a need, since they allow its timely detection, which in turn will result in the prevention of a late diagnosis7. A wide margin of clinical suspicion is required to approach patients with CP. In the present study, most patients were male and the reasons for consultation were chronic abdominal pain, weight loss and diarrhea, which are also signs suggestive of EPI. Likewise, a considerable proportion of participants were diabetic and showed pancreatic atrophy, which suggests that, on the one hand, they were already in advanced stages of the disease and they had pancreatic insufficiency, both exocrine and endocrine, and, on the other, that their referral to gastroenterology services was delayed. This information is intended to complement the knowledge of physicians who provide care to similar populations, so that their clinical suspicion of CP is increased and early detection is achieved in order to make a timely diagnosis and, this way, improve the care provided to these patients.
In the present study, similar demographic characteristics to those reported in international studies1,17,27,28 were observed. Regarding the patients’ history of disease, hypertension and dyslipidemia, which are also considered risk factors for cardiovascular disease, were the most frequent. This is to be expected, since a higher risk of cardiovascular diseases such as heart failure29, acute myocardial infarction30 and hypertension31 has been found in patients with CP, and especially in those with EPI. Hypertriglyceridemia has also been associated with CP7,20,32. In this sense, in United States of America, the NASP group identified hypertriglyceridemia as a risk factor in 13% of patients33, which may explain the frequency of this condition found in our study. Despite the presence of family history of pancreatic disease has been described as a risk factor for CP20,34, this factor was not prevalent in the study population, probably due to lack of knowledge of the patients and the lack of genetic studies.
Chronic abdominal pain occurs in up to 85% of CP cases1, which is similar to the frequency found in this study. This pain is usually located in the epigastrium, it does not improve with the administration of antacids and significantly alters quality of life8-10. It can be easily interpreted as a functional disorder such as irritable bowel syndrome or dyspepsia. This group of patients should be placed under special observation, where semiologic characterization of pain, its study and follow-up are fundamental, since they will allow the clinician to suspect or dismiss a possible diagnosis of CP.
Between 41% and 86% of patients with CP develop DM during their lifetime11. It is worth noting that in our study, 22.2% of the patients already had DM, which is a significant finding due to the sample size and mean age. Other clinical manifestations of EPI, such as poor digestion, can cause chronic diarrhea or steatorrhea in 22.5 % of cases35 and weight loss36, which, after pain, were the most frequently reported characteristics in the present study. CP symptoms and signs in early stages of the disease can be nonspecific, including nausea, vomiting, constipation and abdominal distension22, symptoms that were present in about two thirds of the patients included in this study. The isolated occurrence of these clinical signs may be caused by different diseases, a situation that would delay CP diagnosis.
Regarding its etiology, idiopathic CP was reported in more than half of the study population. In China a census conducted in 2018 in 2037 CP patients found that 80.2 % of cases were idiopathic, while the remaining 19.8 % were caused by alcohol consumption35. These results are consistent with the findings of our study, where a quarter of patients reported chronic alcohol consumption, but alcohol consumption was considered to be the cause of CP in only 11.0% cases, which suggests that alcohol is a factor that contribute to the development of CP, but is not exclusive to it. The guidelines for the diagnosis and management of CP7 recommend taking into account scales such as TIGAR-O20 and M-ANNHEIM34, which describe risk factors and etiologies. CP is developed from the interaction of these factors7,19 and its clinical presentation is individual and different in each patient. According to several case series studies conducted worldwide, alcoholic and idiopathic etiologies are the most frequent1,27,33,35,37,38. Recent works have considered alcohol and tobacco use as the most influential factors for the development of CP1,19,27,39,40. This is consistent with the findings of the study by Wilcox et al38, where an alcoholic, idiopathic and genetic origin was determined for 41.9%, 27.8% and 10.2% of cases, respectively. However, these results vary widely according to the habits and lifestyle of each population group analyzed.
Currently, it is known that up to 50% of patients classified as having idiopathic CP show mutations in the trypsin inhibitor gene (SPINK1) or the cystic fibrosis transmembrane conductance regulator gene (CFTR), and that approximately 1% may have hereditary pancreatitis associated with cationic trypsinogen gene mutations (PRSS1)41-44. The mutations above described predispose to a state of chronic inflammation that leads to pancreatic fibrosis41,45,46. The presence of these mutations was not evaluated in the present study possibly due to their high cost and lack of availability, a frequent situation in many health institutions that contributes to the underdiagnosis of this etiology.
Imaging tests are sensitive in the presence of advanced stages of CP, but they are limited in terms of diagnosing during its early stages7,8,18. CT, MRI, and MRCP were the diagnostic imaging tests most commonly used in this study, which is consistent with the recommendations made in the latest guidelines of the ACC7. In addition, the frequency of imaging findings of atrophy (53.1 %), calcifications and pancreatic duct dilatation (49.0 %) reported when using these methods is similar to that what has been described in in international studies (54.0 % and 68.0 %, respectively)18,47. CT has a sensitivity of 75% for PC diagnosis (95% confidence interval [CI]: 66 %-83 %)7,8. Compared to MRI and MRCP, CT scan is the test of choice in patients with suspected PC due to its cost and availability.
MRI has a sensitivity of 78% (95% CI: 69%-85%)7. It can provide high quality images of both the pancreatic parenchyma and the pancreatic duct system. Recently, the intravenous administration of secretin has been used during MRCP, as it allows observing the highest number of pancreatic duct branches, as well as duodenal filling, which is considered a dynamic marker of exocrine pancreatic function8. According to the most recent guidelines, if normal findings are shown in the CT scan, but CP is highly suspected, a MRCP should be performed in order to evaluate changes in the pancreatic ducts48.
The use of EUS is also indicated when CT scan, MRI or MRCP findings are normal, but clinical suspicion of CP is high7. In the present study, EUS was used in 14.8% of patients; pancreatic duct dilatation was observed in all of them, and a suggestive diagnosis of CP, according to the Rosemont classification49, was reported in most of them. This classification system includes 5 parenchymal and 5 ductal criteria, and classifies CP as diagnosis, suggestive, indeterminate or normal49. Although it has the highest sensitivity compared to the other imaging studies (81%, 95% CI: 70%-89%), it is an invasive method, it is not readily available and there may be interobserver differences7.
The strength of this study is to highlight the clinical manifestations developed by patients with CP who visited a gastroenterology outpatient clinic at the local level: with advanced CP characterized by imaging findings, presence of comorbidities and symptoms. This information can be used when assessing patients in clinical practice in order to establish clinical protocols that allow optimizing resources, making an early diagnosis and a reducing the burden of this disease. Limitations of the study include its retrospective nature, which prevented carrying out a complete and real time evaluation of all patients and led to the exclusion of many participants. Also, genetic testing was not performed due to its high cost and lack of availability. This is a gap to be narrowed in the future as technological advances and new diagnostic methods allowing a more comprehensive evaluation of these patients are globalized.
Conclusion
The demographic characteristics of our study population are similar to those reported in international studies. Initial symptoms of CP are not specific, and they can be confused with functional disorders or, more frequently, with advanced stages of the disease such as EPI and DM, this makes CP diagnosis a challenging task in clinical practice. Sometimes it is difficult to prove the existence of risk factors and the appropriate imaging study is not always available, which further favors its underdiagnosis. Given the high frequency of idiopathic PC, prospective studies aimed at determining risk factors and genetic variants associated with CP, in particular in young patients with no evident cause, are needed. The results reported here may contribute to the creation of local clinical scales that guide early studies in order to classify PC properly and timely, and, this way, improve the prognosis and quality of life of our patients.











 text in
text in