Introduction
Gastroesophageal reflux disease (GERD) refers to the abnormal transit of gastric contents into the esophagus due to an alteration in the antireflux barrier, causing symptoms or complications1. Traditionally, GERD has been diagnosed based on the presentation of symptoms, which have been classified as typical (heartburn, regurgitation) and atypical (chest pain, cough, among others). Response or not to treatment is evaluated with acid suppressants, specifically proton pump inhibitors (PPI)2,3. However, in addition to clinical manifestations, other studies, such as upper endoscopy, are required as part of complementary diagnostic studies to document findings that confirm the diagnosis (Barrett’s esophagus, peptic stenosis, and esophagitis grades C and D, according to the Los Angeles classification)4.
Endoscopy may be normal in up to 60% of patients with GERD and this condition is known as non-erosive GERD. Esophageal pH monitoring, with or without impedance, is considered the study of choice to confirm the diagnosis of GERD, even with normal endoscopic studies. This also makes it possible to establish if there is an adequate response to acid suppressive therapy in patients with persistent symptoms during their follow-up and to classify the type of reflux (acid and non-acid). It is indicated without suppressive therapy with PPIs during presurgical assessment of patients with GERD considered as candidates for antireflux surgery, confirmed GERD, atypical symptoms after antireflux surgery, and persistent symptoms despite PPI treatment. On the other hand, it should be performed with PPI therapy in patients with grade C and D esophagitis according to the Los Angeles classification, Barrett’s esophagus, peptic stricture, or previous positive pH-impedance measurement5,6.
Epidemiology
GERD affects people of all ages and genders, with an estimated global prevalence of 8-33%. Given the widespread use of over-the-counter PPIs and the high frequency of diagnostic tests, this disease comes at a tremendous cost to the health system5,7. A study conducted in 4 capital cities of Colombia using the GERDQ questionnaire (gastroesophageal reflux disease questionnaire) found that the prevalence of reflux symptoms is 11.98 %, as well as an association with comorbidities such as arterial hypertension8.
Medical indication
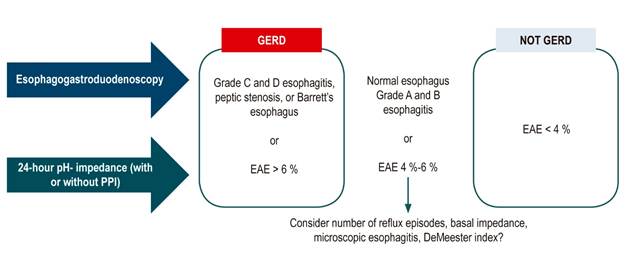
pH-impedance is useful to confirm the diagnosis of GERD in patients with normal esophagogastroduodenoscopy, atypical symptoms, when antireflux surgery is considered, and in the context of refractoriness to treatment with PPIs. Measurement with this test is indicated without acid suppressive therapy when GERD has not been confirmed, there is no previous pH measurement monitoring, and in patients undergoing antireflux surgery (so that surgical treatment is not offered to a patient who does not have the disease). However, in patients with proven GERD (Barrett’s esophagus, peptic stricture, esophagitis grades C and D according to the Los Angeles classification) or with a previous positive pH monitoring study, evaluation with a double dose of acid suppressive therapy is recommended to establish an association between refractory symptoms and reflux episodes. Impedance adds value to pH monitoring, as it allows establishing non-acidic reflux, given that most reflux episodes in patients receiving PPI suppression are weakly acidic. Figure 1 shows the indications for pH impedance with and without acid suppressor treatment9.

Figure 1 Indications of pH- impedance with and without treatment9. Taken from: Roman S et al. Neurogastroenterol Motil. 2017;29(10):1-15.
Technical aspects of the test
For the performance of pH-impedance without acid-suppressive therapy, it is recommended to suspend PPIs 7 days before the test; H2 antagonists, 3 days before; antacids, 6 to 12 hours before; and prokinetics, 5 to 7 days before. Prior to transnasal catheter placement for pH-impedance monitoring, the patient should have a 6-hour fast to avoid emesis and pulmonary aspiration. Patients must be instructed to eat their regular meals while being monitored, as well as to keep track of their intake, their periods in vertical and supine positions (including the time they go to bed), and symptoms9,10.
The pH-impedance catheter is made up of a pH sensor and 8 impedance sensors. Multichannel impedance measurement uses the inherent conductive properties of the intraluminal bolus (liquid, gaseous or mixed) to examine the presence and transit of the bolus in the esophageal lumen. There are devices available to allow for combined monitoring (monitoring of esophageal pH and impedance or esophageal manometry and impedance)10,11 (Figure 2).
Impedance analysis is a measure of total resistance to AC current flow, which depends on the properties of the material in contact with the electrodes and reflects the presence of esophageal contents during the test10,11.
With impedance measurement, it is possible to differentiate between liquid, gaseous or mixed boluses. It also allows the evaluation of esophageal bolus transit. The direction of the bolus is determined by the sequence time from bolus entrance to bolus exit through different measurement segments10,11 (Figure 3).

Figure 3 Representation of the bolus between 2 impedance electrodes, which initially records an increase in impedance due to the air that opens the way for the bolus in the esophagus, with a subsequent rapid decrease in impedance when the bolus is located between the two electrodes. Then, an increase in impedance is observed, which corresponds to the esophageal contraction caused by the bolus impulse, with a subsequent progressive return to baseline impedance as the bolus is cleared from the segment between the 2 electrodes10.
Impedance testing is generally used in combination with pH monitoring because this method provides additional information and allows for a better assessment of GERD. Impedance analysis combined with pH monitoring allows the detection of gastroesophageal reflux of various inconsistencies (acid, non-acid, liquid, and non-liquid events). These findings are relevant because a significant percentage of patients with GERD (45%) who do not respond to acid suppressive therapy have non-acid reflux, which can be diagnosed using impedance10,11.
The pH sensor is positioned 5cm above the lower esophageal sphincter, where the catheter does not move with swallowing into the stomach. Underreporting of reflux episodes has been demonstrated if it is placed at a greater distance. The location of the catheter should ideally be guided by esophageal manometry, thus establishing the position of the lower esophageal sphincter (LSS) for proper positioning. If this tool is not available, it can be found by verifying that the pH is alkaline, which allows establishing its location in the esophagus 5cm proximal to the LSS10.
The pH catheter must be properly calibrated prior to its placement in buffer solutions, with a pH between 4 and 7, following the manufacturer’s instructions.
Analysis and interpretation of ph measurement and impedance analysis
Throughout history, the method for diagnostic evaluation of GERD has been modified in accordance with several consensus. In 2006, the Montreal Consensus defined GERD as an esophageal disorder that occurs when reflux of stomach contents into the esophagus causes symptoms or complications. It also classified individuals with GERD into esophageal or extraesophageal syndromes based on their symptoms, which does not differentiate well from other esophageal and extraesophageal disorders; this situation calls into doubt the diagnosis of GERD considering only symptoms12,13.
The Lyon Consensus, the most recent on GERD, proposed that symptoms may be unreliable, and indicated an objective evaluation of patients with suspected GERD with a diagnosis based on endoscopic findings (severe esophagitis, peptic stenosis, long-segment Barrett’s esophagus) and 24-hour pH-impedance findings, which define GERD when esophageal acid exposure (EAE) is >6%. For this reason, this consensus provides most of the criteria for interpretation of pH-impedance described below5. An example of a pH-impedance plot is shown in Figure 4.

Source: Own elaboration.
Figure 4 24-hour pH- impedance monitoring study without treatment. UES: Upper esophageal sphincter; RIP: Respiratory inversion point.
The DeMeester score has been used for the past 50 years to diagnose GERD. It is a composite score that measures acid exposure during the 24-hour pH- impedance reflux monitoring. Acid reflux is defined whenever the pH of the esophagus measured 5cm above the upper edge of the LSS decreases to 4 or less. DeMeester parameters include the total number of reflux episodes, total esophageal pH time less than 4, upright esophageal pH time less than 4, supine esophageal pH less than 4, number of reflux episodes greater than 5 minutes, and longest reflux episode13.
For proper analysis and interpretation of pH-impedance, it is recommended to perform it in steps.
Step 1: Duration of pH-impedance monitoring
Evaluating the duration of pH- impedance monitoring, which should be at least 16 hours in order to establish an adequate analysis5,9.
Step 2: Determining EAE
EAE refers to the time the esophagus is exposed to pH less than 4 and correlates with the presence of GERD. If the EAE is less than 4 %, it is considered normal; if it is greater than 6 % within 24 hours, it is considered abnormal and establishes the diagnosis of GERD. If EAE between 4% and 6% is reported, it is classified as inconclusive or gray area and additional action is required to confirm the diagnosis (Figure 5)5,9,14.
Step 3: Evaluating the number of reflux episodes
Reflux episodes are classified as acidic and non-acidic (including weakly acidic). Less than 40 acid reflux episodes in 24 hours is considered normal, while a number greater than 80 is considered abnormal. When more than 80 acid reflux episodes occur, GERD is diagnosed even if the EAE is in an inconclusive range or gray area (between 4% and 6%). The number of non-acidic reflux episodes establishes the diagnosis of non-acid reflux disease when more than 27 episodes of this type occur without acid suppressor therapy, or when more than 44 occur while the test is performed in the presence of acid suppressor therapy. Both acidic and non-acidic reflux episodes should be reported if they occurred in a vertical, supine, or postprandial position5,9,10,15.
Step 4: Establishing the association of symptoms with reflux episodes
The association of symptoms with reflux episodes comprises the clinical manifestations of GERD reported by the patient that occur up to 2 minutes before recording the reflux episode. To consider the association of a symptom with reflux episodes, it must have been reported 3 times or more in the patient’s record. The association of symptoms with reflux episodes includes two evaluations: the symptom index (SI) and the symptom association probability (SAP). SI is the percentage of symptomatic events preceded by reflux episodes; it is considered positive when it is ≥ 50%. This index was defined as the number of times the symptom occurred when the pH was less than 4.0, divided by the total number of times the symptom was reported, multiplied by 100 %.
SAP takes into account the total number of symptom events, reflux episodes, and reflux-related symptoms; it is considered positive when it is >95%. These two assessments are complementary, measure different parameters and cannot be compared with each other. It is possible to have a positive SI and a negative SAP, or vice versa, indicating an uncertain area in which additional interpretation with other parameters is required to define the diagnosis; measurements that could be used are the EAE, number of reflux episodes, and baseline impedance. Interpretation of these indexes is also useful in determining differential diagnoses such as functional heartburn and reflux hypersensitivity. When there is a positive SAP and SI with EAE less than 4%, the diagnosis of reflux hypersensitivity is established.
The diagnosis of functional heartburn is defined as the presence of heartburn in a patient with normal pH impedance, in addition to negative SAP and SI, in whom other organic causes explaining the symptoms have been ruled out (eosinophilic esophagitis, rumination, and supragastric belching) (Figure 6)13,15.
Step 5: Evaluating the DeMeester score
The DeMeester score is used to diagnose GERD since 1974 with a performance very similar to EAE. It may play a decisive role in defining, in specific cases, when a patient has or does not have GERD, particularly in situations in which the other parameters are not defining5,9. In our unit, we use it to establish a diagnosis of GERD when the EAE and the total number of acid reflux episodes are indeterminate. In this particular case, a DeMeester score greater than 14.7 establishes the diagnosis of GERD.
Step 6: Mean nocturnal baseline impedance
The mean nocturnal baseline impedance is the expression of mucosal integrity and provides evidence of macroscopic and microscopic esophageal damage after exposure to reflux. It consists of measuring baseline impedance 3 to 5cm above the lower esophageal sphincter during sleep. Impedance measurements are taken in 3 periods of 10 minutes to obtain the measurement. Values less than 2292 Ohm suggest the presence of GERD and are correlated with patients with suspected GERD associated with typical symptoms that respond to treatment with PPIs or antireflux surgery5,9,16.
Step 7: Post-reflux swallow-induced peristaltic wave index
This index reflects the integrity of esophageal peristalsis, stimulated by reflux episodes, and clearance due to saliva, which contains a large amount of bicarbonate. It is abnormal when there is an anterograde 50% drop in impedance within 30 seconds after a reflux episode originating at the proximal impedance sites and reaching the distal impedance sites and followed by at least 50% return to baseline. The cut-off value set is 61%10,16.
Step 8: Evaluating the presence of nocturnal acid breakthrough
Rebound acid hypersecretion is defined as the increase in acid secretion after a period of acid suppression. It has been reported after treatment with histamine blockers as well as with PPIs. During sleep, the frequency of reflux episodes decreases; however, when patients receive PPIs and are on a prescription plan, they may present with nocturnal acid breakthrough, which is defined as an episode of acid reflux during the overnight period for at least 60 continuous minutes17-20.
Conclusion
The study and diagnosis of GERD requires the integration of clinical aspects, endoscopic findings, and confirmation with objective documentation of GERD with the performance of 24-hour pH-impedance monitoring, conditions that will allow patients to be classified into different phenotypic groups to better address their therapeutic needs. The stepwise interpretation of pH-impedance allows, in a logical order, to make an adequate reading of this digestive physiology study for its subsequent application in our patients. It is important to inform patients of all the technical details of the study to obtain the most reliable results with the best possible observation. To date, pH-impedance measurement is the gold standard in the diagnosis of GERD, with a sensitivity of 77-100 % and a specificity of 85-100 %.











 text in
text in