Introduction
The use of percutaneous endoscopic gastrostomy (PEG) as a strategy to ensure nutritional support has increased exponentially in the last two decades due to its simplicity and safety1. The group of patients with real indications for this procedure and who benefit from it is increasingly select. Recent studies have questioned its use in patients with severe cerebrovascular disease, poor prognosis and advanced dementia2. Although there is no evidence that PEG improves survival, quality of life, or nutritional status3, it continues to be used in up to 60% of patients in chronic care units4, 10% of patients in nursing homes5, and in 5% of patients over 85 years of age6. The overall complication rate of PEG ranges from 1% to 15%7. Serious complications are rare8, and minor complications occur in up to 10% of cases9; besides, procedure-related mortality is less than 1%10. Major complications include necrotizing fasciitis; intestinal, gastric or esophageal perforation; peritonitis; bleeding, and the occurrence of fistulas11. In this paper, the case of a patient with a serious, infrequent and often unsuspected complication that should be considered within the differential diagnosis of potential complications related to the use of a gastrostomy tube is presented.
Clinical case
This is the case of a 56-year-old woman diagnosed with dysphagia secondary to a central nervous system disease and who had undergone a gastrostomy one year ago. One week after the gastrostomy tube was replaced due to malfunction, she consulted due to experiencing severe abdominal pain, fever and vomiting. The patient was assessed by the general surgery department, where acute abdomen was suspected. Regarding laboratory tests, neutrophilic leukocytosis was reported in the complete blood count test, as well as elevated transaminases (10 times) and alkaline phosphatase (3 times) in the lipid panel. In addition, the following findings were observed in a contrast-enhanced abdominal CT scan: thickening of the duodenal bulb and the second portion of the duodenum, normal bile duct without presence of stones, and inflammatory changes of the body and tail of the pancreas without peripancreatic fat involvement. The radiologist’s conclusion was “nonspecific thickening of the duodenal bulb and the second portion of the duodenum “ and “Baltazar A edematous pancreatitis”. Serum amylase and lipase levels were 432 U/L and 229 U/L, respectively.
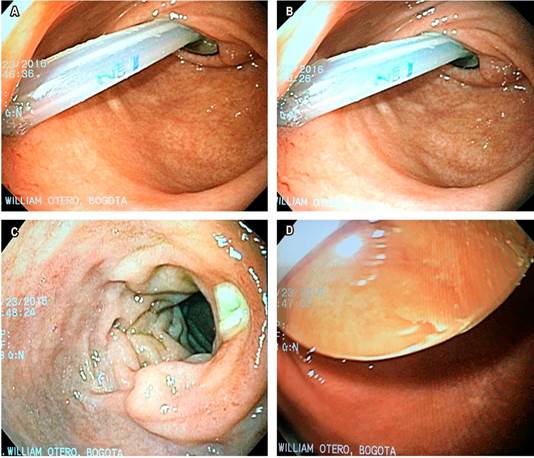
Due to suspicion of acute pancreatitis and the thickening of the duodenum evidenced on the abdominal CT scan, a magnetic resonance cholangiopancreatography (MRCP) and an esophagogastroduodenoscopy (EDG) were requested. Chronic gastritis and migration of the gastrostomy balloon to the duodenum were observed in the EDG (Figure 1). Furthermore, a 10 mm fibrin-covered ulcer was found in the posterior semicircle of the duodenal bulb, which was considered to be secondary to the trauma caused at that site by the tube. Upon reaching the second portion of the duodenum, the balloon was found to occupy 80% of the lumen and was immediately deflated, recovering a 30 mL volume; then, gastrostomy tube traction was performed and the balloon was correctly positioned and filled with only 4 mL of saline solution, as indicated by the manufacturer. After this maneuver was carried out the patient experienced a marked improvement of symptoms (constant moaning, restless movements and pain).
Treatment was modified and nutrition was started through the gastrostomy tube. The patient was diagnosed with acute pancreatitis secondary to compression of the major papilla by the gastrostomy balloon and with a traumatic duodenal ulcer caused by the gastrostomy tube. The elevation of transaminases was considered to be produced by the bile duct obstruction taking place in the papilla.
Taking these findings into account, the MRCP was not performed. The patient’s condition successfully improved and her caregivers once again received education regarding gastrostomy tube management and care according to the “family and caregiver education” protocol for “gastrostomy tube management” of the treating institution. On the fourth day after her admission she was discharged without experiencing any complication.
Discussion
PEG is currently the method of choice for long-term enteral tube feeding12. This technique was first described in 1980 by Gauderer et al13 and it is considered a safe procedure with few complications14. The potential complications of PEG, as well as their frequency15, are described in Table 1.
Table 1 Complications related to the use of PEG
| Complications | Frequency |
|---|---|
| Major | |
| Intestinal perforation | 1 %-2 % |
| Peritonitis | 1 % |
| Pulmonary aspirarion | 0.5 %-1 % |
| Bleeding | 1-5 % |
| Necrotizing fasciitis | 0.2 % |
| Death | 0.5 %-0.8 % |
| Minor | |
| Gastric Ulcer | 1 %-2 % |
| Peristomal infection | 5 %-20 % |
| Ileus | 1 %-2 % |
| Buried bumper syndrome | 1 %-3 % |
Acute pancreatitis is a rare complication of gastrostomy, but one of the most serious. The first case was described by Bui et al.16. more than three decades ago. These authors hypothesized that the migration of the gastrostomy balloon caused an obstruction and a direct mechanical trauma on both the major and minor papilla, causing edema and inflammation of the mucosa, which in turn prevents the flow through the pancreatic duct16. Since then, it has been accepted that this is probably the mechanism responsible for causing acute pancreatitis. After performing a literature search in PubMed we found that 14 of the cases have been published worldwide (Table 2).
Table 2 Cases of acute pancreatitis secondary to gastrostomy balloon migration published worldwide.
| Study | Type of tube | Insertion time |
|---|---|---|
| Bui et al., 1986 16 | Foley | 1 year |
| Panicek et al., 1988 17 | Foley | ND |
| Barthel et al., 1991 18 | Foley | 6 months |
| Duerksen et al., 2001 19 | PEG | 3 months |
| Miele et al., 2005 20 | Foley | ND |
| Imamura et al., 2007 21 | PEG | 1 mes |
| Shah et al., 2012 22 | Foley | 24 horas |
| Shah et al., 2012 22 | PEG | ND |
| Brauner E et al., 2014 15 | Foley | 1 year |
| Taylor et al., 2016 23 | PEG | ND |
| Hawatmeh et al., 2016 24 | PEG | 1 year |
| Hawatmeh et al., 2016 24 | PEG | 2 years |
| Sekmenli et al., 2018 25 | PEG | 2 months |
| Saleem S et al., 2018 26 | PEG | 1 year |
| Belat et al., 2019 27 | PEG | 2 years |
This complication never occurred after the initial placement of the device in the cases reported in the literature. After analyzing each of these cases, included the one presented here, a common triggering factor was found: recent manipulation of the gastrostomy tube after being replaced. In most cases a favorable outcome, with rapid improvement of symptoms and normalization of laboratory and imaging abnormalities, was reported. In half of the cases, the complication was caused by a Foley catheter. It should be noted that this type of catheter is not designed to be used as a gastrostomy tube, and the only indication for its use is when it is needed as a transitory measure to ensure the permeability of the gastrocutaneous route when the initial tube is dislodged, and the replacement gastrostomy tube can be inserted through it. Additionally, balloon migration is another problem that takes place when Foley catheter is used, since it does not have an external stop enabling it to remain fixed on the skin28. Due to these circumstances, we recommend using Foley catheter only as a temporary measure and not as a long-term solution.
If tube feeding needs to be maintained as the cause for its insertion persists, the replacement tube must be used and the temporary tube must be replaced as soon as possible. Gastrostomy tubes have an average life of 12-15 months depending on how they have been taken care of29. There are patients in which the gastrostomy tube remains functional up to two years. The most frequent causes for tube replacement include tube perforation, balloon rupture, leakage or local infectious complications30. In this regard, Atencio et al. reported that displacement, catheter deterioration, and balloon rupture were the cause of tube replacement in 12.5 %, 7.3 % and 4.1 % of cases31. Caregivers frequently express concern and discomfort about changes related to the color, appearance or deformity of the external device and “demand” replacing the tube. However, if it still works properly, replacement is not required, since its unnecessary replacement implies additional costs for the health system32. On other occasions, and in our personal experience, the relatives of the patient, motu proprio, use very hot food, which causes deterioration and porosity of the tube, and, over time, bad smell. Under these circumstances the gastrostomy tube must be replaced, but educational interventions regarding how to take care of the tube can be carried out in such cases.
In general, there is no good quality evidence about the benefit of periodically checking the location of the gastrostomy opening33. Besides, such verification must be performed only when doubts about its proper functioning arise, the adequate functioning of the tube is verified specific medical visit and the possibility of buried bumper syndrome is evaluated34. In said consultation, the location of the external button is observed, the gastrostomy tube is inserted by making sure it enters without any problem and the free rotation maneuver is performed, which consists of verifying that rotating the probe does not imply any difficulty. Likewise, the presence of microperforations in any part of the tube is also checked. Finally, if the gastrostomy tube has a balloon, it is deflated and, after confirming it does not have more than the recommended volume, it is filled again with the minimum volume recommended by the manufacturer and the external stop is moved over the desired mark35.
Conclusion
Acute pancreatitis is a rare but potentially serious complication of gastrostomy and it is mainly caused by the obstruction of the papilla secondary to migration of the balloon into the second portion of the duodenum. This complication usually occurs after incorrect tube replacement, in which the balloon is overfilled and is not fixed externally to prevent its displacement. There is a false belief among physicians and caregivers who think that using a larger volume to insufflate the balloon will reduce the risk of ostomy leak or voluntary or involuntary removal of the gastrostomy tube. On the contrary, we recommend insufflating the balloon with the minimum volume established by the manufacturer in order to avoid this and other serious complications. Thus, we reiterate that it needs to be handled exclusively by highly qualified persons that have been trained to use it properly.











 texto em
texto em