Introduction
Hemangiomas are rare benign vascular neoplasms that can occur anywhere in the body. They mainly affect the skin, the liver and the pancreas, and, less frequently, the gastrointestinal tract. In the case of GI tract involvement, the sigmoid rectum is the site most commonly affected by these neoplasms1-3. Hemangiomas account for approximately 5% of all gastrointestinal tumors4,5 and are the second most common vascular cause at the colorectal level6. The incidence of hemangiomas is 1 in 1500 patients1,7,8.
There are three types of hemangiomas: cavernous, capillary and mixed, and they can occur as a single or as multiple lesions in one or several organs, and are part of specific syndromes2,4,6,9. Intestinal hemangiomas are associated with syndromes with mucosal and cutaneous venous malformations such as Rendu-Osler-Weber syndrome and Klippel-Trenaunay-Weber syndrome1,6.
Little is known about this rare and misdiagnosed disease, provided that its clinical presentation is similar to those of other gastrointestinal diseases and many cases are not confirmed by means of pathology studies. In this sense, a high index of suspicion and ruling out other more common diseases are required for its diagnosis.
Case presentation
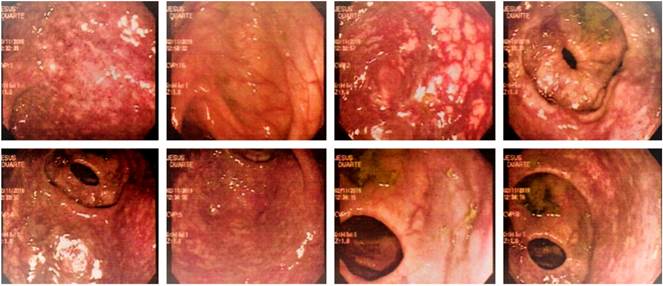
This is the case of an 18-year-old male patient who was brought to the emergency department for he had experienced abundant rectal bleeding (blood in stool), asthenia, adynamia and generalized pallor for approximately one month, but without presenting abdominal pain, fever or other associated symptoms. A marked paleness of the skin and of the mucous membranes, as well as stable vital signs were reported on his physical examination. A barium enema was performed and no abnormalities were observed. In addition, further paraclinical tests allowed identifying the patient was anemic based on his hemoglobin count (5.8) and hematocrit levels (18 %), which led to perform further studies to determine the cause of anemia. Then, an extensive violaceous lesion with a redundant vascular network located in the rectum and the sigmoid colon affecting the entire circumference of the rectum compatible with colonic hemangioma was identified on colonoscopy (Figure 1). The patient was taken to surgery and the diagnosis of cavernous hemangioma of the sigmoid colon was confirmed by means of the pathology report.
Pathology report
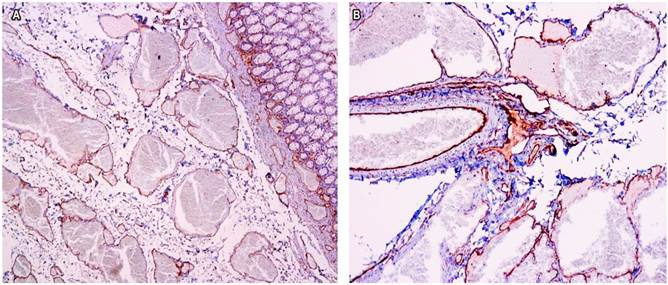
A 17 x 8 x 3 cm violaceous segment of the colon was sent to the pathology department. Multiple thickened vessels of hemorrhagic content occupying and occluding the lumen by 50% were identified in the section; the lesion was located 1.5 cm from the resection margins. Microscopic examination showed colonic mucosa with a multiple vascular lesion compromising the entire thickness of the wall and made up of a proliferation of medium and large caliber dilated vessels covered by endothelial cells without atypia and in its interior some were found to be thrombosed, with papillary endothelial hyperplasia and some areas with eosinophilic content in its interior (Figures 2 and 3).
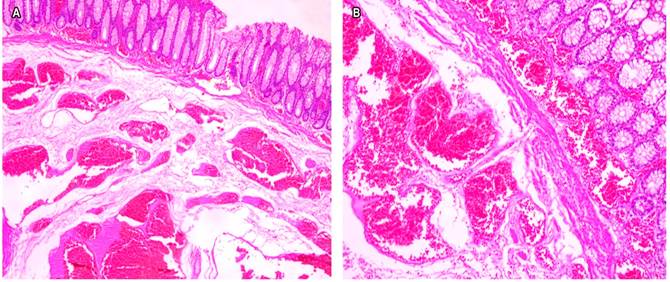
Figure 2 Image of the lesion in which blood vessels of different sizes are observed in the submucosa. The upper part shows healthy rectal mucosa. A. Hematoxylin-eosin (HE) 4x. B. HE 10x.
Discussion
Hemangiomas are hamartomatous lesions derived from mesodermal tissue that occur since birth1,2,10; however, some researchers consider them as true neoplasms due to their growth potential2. They are rare tumors, especially in the gastrointestinal tract, and they are most frequently located in the rectum and the sigmoid colon1-4. Approximately 120 cases have been reported in the literature since 183911,12. These lesions can occur at any age, although the average age of onset ranges from 5 to 25 years, and they are more frequent in young adults, especially those in their third decade of life4,6,10. No sex predominance has been demonstrated4,10. There are three types of hemangiomas based on their predominant component: cavernous, capillary and mixed hemangiomas. Cavernous hemangiomas are the most frequent2,10,11,13,14, since they account for approximately 80% of colorectal lesions; these are nonencapsulated, bluish lesions with dilated blood vessels of variable size that can compromise the entire thickness of the colon, invading it from the mucosa to the serosa; besides, there are two types: circumscribed and diffuse2,11. Thromboses frequently occur within the sinusoids resulting in subsequent calcification and then forming the so-called phleboliths, which are an important diagnostic feature1,10. Capillary hemangiomas constitute 10% of lesions; they are non-encapsulated, solitary and asymptomatic lesions. Finally, the remaining 10% are mixed hemangiomas, which are a combination of both cavernous and capillary hemangiomas2,11. They have different forms of presentation depending on their location.
Reasons for consultation in these patients usually include bleeding or symptoms of mechanical bowel obstruction. Gastrointestinal bleeding is the predominant symptom; it is generally painless, recurrent, sometimes massive, and it can evolve to shock with a mortality rate ranging from 40% to 50%1 and depends on the size and type of vascular malformation6,10. A high index of suspicion, an adequate anamnesis and a complete physical examination, together with further testing are necessary to reach this diagnosis6. Chronic intestinal bleeding along with anemia occur in 13 % to 33 % of patients with Rendu-Osler-Weber syndrome15. Likewise, it is frequently misdiagnosed because it is an infrequent disease and patients present with symptoms that may also occur in more common conditions6. In this regard, Jeffery et al. found that this condition had been misdiagnosed in 80% of patients (a high percentage), being hemorrhoidal disease the main diagnosis, and that most patients had undergone a hemorrhoidectomy before being diagnosed with hemangioma12. Videocolonoscopy is the gold standard for reaching a diagnosis of colon hemangiomas, provided that most of these lesions are located in the sigmoid colon and the rectum1,11,13. There are other diagnostic tools that complement videocolonoscopy in order to establish the exact location of lesions and determine resection margins. X-rays are an easily accessible diagnostic tool in which phleboliths, pathognomonic sign of these lesions, can be identified in 26% to 50% of cases1,6,10.
Computed axial tomography (CT) scan and magnetic resonance imaging (MRI) are used to establish the resection margins of the lesion and to rule out infiltration of pelvic organs11,16. According to Djourhi et al., compared to CT scan, MRI is the imaging test of choice to evaluate the extension of colon cavernous hemangiomas due to its resolution and the fact it is a non-invasive method, especially in young patients, since CT scan must be performed on multiple occasions for follow-up and control purposes, and requires the patient to be injected with contrast mediums or iodine17.
Conclusion
Gastrointestinal hemangiomas are an uncommon and misdiagnosed disease that must be considered in any patient presenting with recurrent intestinal bleeding and signs of bowel obstruction, especially if they are young.
There are several diagnostic tools; however, emphasis must be placed on a complete anamnesis and a high index of suspicion, since diagnostic and therapeutic errors are usually made, which results in the patient undergoing unnecessary surgeries. Videocolonoscopy, which is the gold standard, is the diagnostic method of choice, and it must be complemented with X-rays, CT scans or MRI, being the latter the most preferred in cases of cavernous hemangiomas located in the colon.











 text in
text in