Introduction
Malakoplakia is a rare, granulomatous, chronic inflammatory disease that affects many organs, including the skin, the lungs, the central nervous system (CNS) and those in the genitourinary tract and the gastrointestinal tract1. It occurs most commonly in the genitourinary tract (60%-80% of cases), followed by the gastrointestinal tract (15%), and less frequently in other organs such as the skin, the lungs and the CNS2. Its prevalence is unknown, but more than 700 cases have been reported. It may occur at any age, with a mean age of diagnosis at 50 years. Pediatric cases are rare. Malakoplakia incidence is higher in males and it does not have predilection for any race. It has been associated with other coexisting conditions such as sarcoidosis, tuberculosis, organ transplantation, allergic diseases, cytotoxic chemotherapy, acquired immunodeficiency syndrome (AIDS), neoplasms, steroid use and poorly controlled diabetes3,4. Its diagnosis is reached based on histological criteria when large Hansemann macrophages containing laminated calcific spherules known as Michaelis-Gutmann bodies are observed5,6. The prognosis of this disease depends on its extent, location and the underlying health status of the patient7.
Case presentation
This is the case of a 15-year-old patient without any significant history of disease who was referred to our hospital due to hematochezia. In addition, he had the following family history: type 2 diabetes (mother), scleroderma (maternal aunt), amyloidosis (maternal aunt), and gastric cancer (great-grandmother). According to the patient, he was 7 years at the time of disease onset, experiencing hematochezia and mild abdominal pain that improved after defecation. In 2011, he underwent a colonoscopy in which 3 to 4 mm raised pseudopolypoid lesions were observed in the sigmoid colon and rectum and malakoplakia was described in the biopsy report. At that time, he was treated with oral ciprofloxacin 500 mg for 14 days, experiencing an improvement of his symptoms. In 2016, another colonoscopy was performed due to proctorrhagia and mild abdominal pain. Again, nodular pseudopolypoid lesions were identified in the sigmoid colon and the rectum (Figure 1), and inflammatory polyps with aggravation foci, numerous histiocytes and reactive epithelial changes were described in the biopsy report. On this occasion, he was administered oral ciprofloxacin 500 mg every 12 hours for 14 days, experiencing symptomatology improvement. In July 2018, irregularly distributed pseudopolypoid lesions with normal colonic mucosa and flat areas of pearly appearance with irregular borders were observed on a new colonoscopy (Figure 2); in addition, the following findings were described in the biopsy report: inflammatory polyps, chronic colitis accentuated with periodic acid Schiff (PAS) staining, and absence of Michaelis-Gutmann bodies.
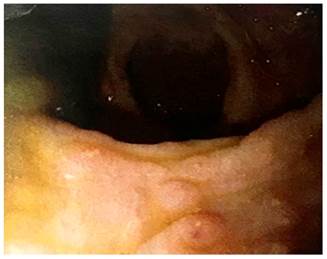
Figure 1 Videocolonoscopy showing nodular pseudopolypoid lesions on the mucosa of the sigmoid colon and the rectum.
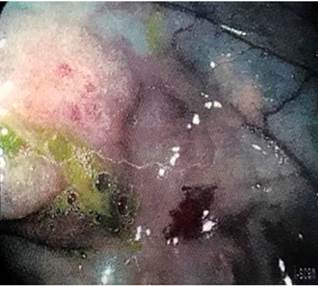
Figure 2 Irregularly distributed pseudopolypoid lesions with normal colonic mucosa, pearl-like flat areas with irregular borders.
The patient was admitted to our hospital due to having experienced mild abdominal pain and 4-5 bloody diarrhea episodes without mucus, straining or tenesmus within 24 hours. Mucosal and skin paleness, no abdominal tenderness to palpation and mild pain in the left colon, as well as the following vital signs were reported on physical examination: blood pressure: 110/70 mm Hg and heart rate: 82 beats per minute. The mother of the patient was interviewed, but she denied knowing the condition her son had been diagnosed with, despite having endoscopic and histopathological reports confirming the diagnosis of malakoplakia. She also expressed that at the time he was not undergoing any treatment or following dietary indications at home. Anemia, hypoalbuminemia, cytomegalovirus (CMV), reactive herpes virus immunoglobulin G (IgG), decreased fecal calprotectin and positive Entamoeba coli and Entamoeba histolytica were reported in laboratory tests. Treatment consisting of the administration of intravenous ciprofloxacin and metronidazole was started, and performing an endoscopic procedure was considered.
The patient’s laboratory findings are presented in Table 1.
Table 1 Patient’s laboratory findings.
| Test | Value |
|---|---|
| Leukocytes | 10 300 |
| Neutrophils | 69,8 % |
| Lymphocytes | 18,50 % |
| Monocytes | 8,60 % |
| Eosinophils | 3 % |
| Basophils | 0,10 % |
| Erythrocytes | 3,80 |
| Hb | 9,60 g/dL |
| Hct | 30,20 % |
| MCV | 79 fL |
| Platelets | 260 000 |
| Albumin | 2,6 g/dL |
| Urea | 23 |
| Creatinine | 0,61 |
| Total bilirubin | 0,41 mg/L |
| ALT | 15 |
| AST | 19 |
| PT | 16,1 s |
| INR | 1,35 |
| CMV IgG | Reactive |
| CMV IgM | Nonreactive |
| Epstein BARR IgG | Negative |
| Epstein BARR IgM | Negative |
| Herpes I and II IgG | Reactive |
| Ferritin | 241 ng/mL |
| Vitamin B12 | 268 pg/mL |
| Serum iron | 19 µg/dL |
| Folic acid | 13 ng/mL |
| Transferrin | 166 mg/dL |
| Fecal calprotectin | 116 µg/dL |
| E. coli | Positive |
| E. histolytica | Positive |
| Stool culture | Negative |
| Aerobic and anaerobic blood cultures | Negative |
ALT: alanine aminotransferase; AST: aspartate aminotransferase; Hb: hemoglobin; Hct: hematocrit; INR: international normalized ratio; PT: prothrombin time; MCV: mean corpuscular volume.
Endoscopic studies and histological findings
A 2 cm lesion of submucosal appearance located on the mucosa of the antrum was visualized in the upper endoscopy (Figure 3). In addition, pseudopolypoid lesions with fibrin exudate on their surface were observed in the duodenum (Figure 4).
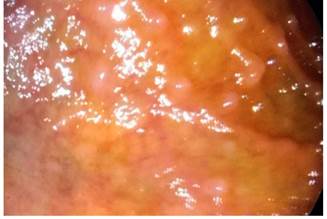
Figure 4 Pseudopolypoid lesions with fibrin exudate on their surface located on the mucosa of the duodenum as observed in the upper endoscopy.
In addition, multiple 5-15 cm sessile, soft, ulcerated and hemorrhagic pseudopolypoid lesions located in the sigmoid colon and rectum were observed on videocolonoscopy (Figures 5 and 6).

Figure 5 Small pseudopolypoid lesions resembling polyposis were observed on the mucosa of the sigmoid colon during videocolonoscopy.
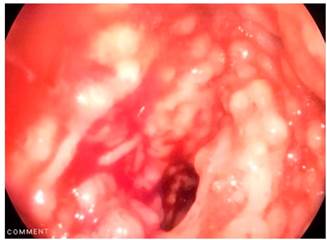
Figure 6 Multiple 5-15 cm sessile, soft, ulcerated and hemorrhagic pseudopolypoid lesions on the mucosa of the sigmoid colon and rectum as observed on videocolonoscopy.
Malakoplakia, characterized by of granular histiocytes, several of which contained intracytoplasmic Michaelis-Gutmann bodies, was described in the histology report. The diagnosis was confirmed by means of histochemistry using periodic acid Schiff (PAS) staining (Figure 7).
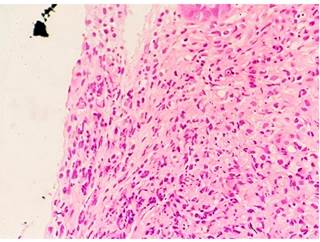
Figure 7 Histological finding consisting of histiocyte aggregates inclusions and Michaelis-Gutmann bodies with pathognomonic features of malakoplakia.
Abdominal pain and diarrhea disappeared one week after the intravenous administration of ciprofloxacin 200 mg every 12 hours was started, and therefore the patient was discharged with outpatient follow-up indication. Six months later, in a follow-up consultation, he was asymptomatic and had gained weight as he was complying with nutritional indications consisting of the consumption of ascorbic acid and multivitamins. The patient’s parents were informed of the clinical course, diagnosis and prognosis of the disease, since their son had been diagnosed with malakoplakia for 7 years, but none of his relatives were aware of it. The patient has been healthy in all his outpatient follow-up consultations.
Discussion
Malakoplakia is a rare, granulomatous, chronic inflammatory disease. It is mainly diagnosed based on characteristic features of histiocyte aggregates containing cytoplasmic inclusions known as Michaelis-Gutmann bodies8,9. The second site most frequently affected is the gastrointestinal tract, with 11% of cases, specifically in the rectum, followed by the sigmoid colon10,11. Its clinical manifestations are widely variable, ranging from being asymptomatic to experiencing diarrhea, abdominal pain, rectal bleeding, bowel obstruction, vomiting, malaise and fever12,13. Its pathogenesis is still unknown, but three possible pathogenic mechanisms have been suggested: an unusual causative organism, an abnormal or altered immune response, and an abnormal macrophage response due to lysosomal function defects11. Malakoplakia occurrence is reported more frequently in patients with coexisting conditions such as organ transplantation, tuberculosis, immunosuppressive therapy, acquired immunodeficiency syndrome, neoplasms and poorly controlled diabetes2,14.
The association between malakoplakia and colon adenocarcinoma is rare. Most cases reported in the literature occur in the rectum and the sigmoid colon, and predominantly in males; besides, it seems that the presence of malakoplakia does not alter the prognosis of the tumor, as shown in a meta-analysis of cases associated with colon adenocarcinoma6,15. In the case reported here, the etiology of malakoplakia was unclear, because, on the one hand, he did not have any specific history of disease and, on the other, he did not have a malignancy or a chronic disease, nor he was in the age group in which malakoplakia occurs most frequently. As it was stated before, the patient was a healthy adolescent male without associated diseases, with pseudopolypoid lesions and in which inflammatory bowel disease (IBD) was considered as a differential diagnosis due to the age onset of malakoplakia16. In addition, symptom improvement was achieved after he underwent antibiotic therapy (ciprofloxacin for 14 days), since it has been demonstrated that ciprofloxacin easily penetrates macrophages and that all granulomatous lesions disappear in the long term when this treatment is implemented. Malakoplakia can be cured with the correct antibiotic therapy7,17.
Due to its rarity, there are no standard treatment guidelines. However, antibiotics and follow-up consultations focused on monitoring adherence to nutritional indications related to the consumption of multivitamins and ascorbic acid are currently the mainstays of malakoplakia treatment, for they have been shown to be effective for this purpose. This is why, the patient’s relatives must be informed of the characteristics of this disease, including its clinical course, diagnosis and prognosis, since it is curable18.
Conclusions
Malakoplakia is a very rare disease in young people without any underlying disease. This exemplifies the rarity of the case presented here and the need for a high level of clinical suspicion to diagnose this disease, as it has a nonspecific presentation. Antibiotics are the mainstay of malakoplakia treatment.











 texto em
texto em 




