Introducction
According to the World Health Organization (WHO), tuberculosis continues to be a public health problem. It is estimated that, by 2015, there were 10.4 million new cases of tuberculosis (regardless of the type) worldwide, while only 6.1 million cases were reported. In the case of Colombia, 13 626 tuberculosis cases were reported in the Colombian Public Health Surveillance System (Sivigila for its acronym in Spanish) in 2016, of which 2147 were tuberculosis and human immunodeficiency virus (HIV) coinfection cases and the reported incidence in the country was 27.9 cases per 100 000 inhabitants1. By the end of 2015, there were already 36.7 million people with HIV, 2.1 million had been infected with HIV, and 1.1 had died from acquired immunodeficiency syndrome (AIDS)-related diseases2,3.
Extrapulmonary tuberculosis diagnosis is confirmed when the infection occurs in organs other than the lungs (pleura, lymph nodes, abdomen, genitourinary tract, skin, joints, bones, esophagus, or meninges)4,5. Esophageal tuberculosis is a rare condition (accounting for only 2.8 % of all gastrointestinal tuberculosis cases). It usually occurs as a result of the direct spread of the infection from mediastinal lymph nodes (rarely from the lungs or the bloodstream)6. Primary esophageal tuberculosis rarely occurs due to protective mechanisms such as multilayered stratified squamous epithelium, mucus, saliva, peristalsis, and upright posture, which cause Mycobacterium tuberculosis bacteria to remain only temporarily in the esophagus7. Esophageal tuberculosis has no clinical, laboratory, radiological or endoscopic characteristics. Its definitive diagnosis requires isolating the tubercle bacilli, which is rarely achieved in clinical practice8; even so, clinically speaking, patients present with dysphagia, odynophagia and weight loss. These clinical findings, together with endoscopic findings, may mimic an esophageal carcinoma diagnosis9. In this paper, the case of a patient with esophageal tuberculosis associated with immunosuppression caused by HIV infection is presented.
Case presentation
This is the case of a 40-year-old male with a 30-year history of chronic guarapo (a fermented alcoholic drink produced from sugarcane) consumption and who was diagnosed with HIV infection one week prior to being admitted to the emergency department due to having experienced the following symptoms for six months: progressive weight loss (approximately 40 kg) associated with progressive dysphagia and worsened by dysphagia to liquids, asthenia, adynamia, hyporexia, pleuritic pain, blood in stools and epigastric pain, the latter being present within the last 10 days before his admission to the emergency service. In addition, he reported having coughed up whitish mucus on several occasions.
The following vital signs were reported on his physical examination on admission to the emergency department: blood pressure (BP): 80/60 mm Hg; mean arterial pressure (MAP): 80 mm Hg; heart rate (HR): 90 beats per minute (bpm); respiratory rate (RR): 22 breaths per minute (rpm); body temperature (°C): 36.5; oxygen saturation (O2Sat): 93%. The patient was alert, had a distant and hostile attitude, with evident signs of attention deficit and expressing thoughts of helplessness and hopelessness. In addition, he was hypotymic with signs of irritability, as well as introspective, showing impaired judgment and suicidal tendencies and thoughts. Physically, he was cachectic and oral mucosa with whitish plaques was found in the palate and the cheeks. Enophthalmia, abdominal distension, and tenderness to palpation in the left hypochondrium, without signs of peritoneal irritation, were also reported. Finally, marked muscle atrophy in the limbs, protein-calorie malnutrition, shiny and scaly skin were also described.
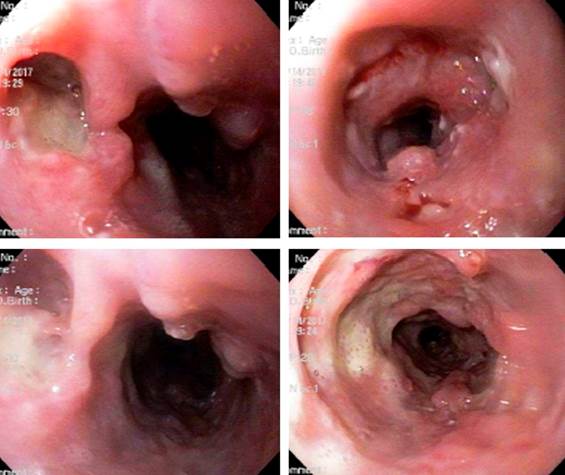
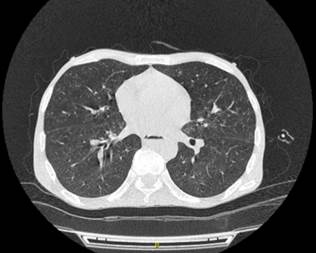
An Acid-Fast Bacillus (AFB) smear and an upper gastrointestinal endoscopy were performed as diagnostic support tests. The AFB smear was positive and the following findings were observed in the upper endoscopy: severely inflamed mucosa with irregular ulcerations up to 2 cm deep, dirty and covered with fibrin, up to 1 cm size irregular elevated lesions, suggestive of gastrointestinal tuberculosis. This was later confirmed by the histopathology report: chronic granulomatous esophagitis suggestive of tuberculosis infection (Figure 1), and a chest CT scan showing centrilobular nodules with tree-in-bud opacity pattern and characteristics suggestive of atypical or typical mycobacteria, and an infiltrate-like space-occupying lesion in the right upper lobe (Figure 2). Additionally, the following findings were reported in the complete blood count tests: leukocytes: 5040/mm3, neutrophils: 70 %, lymphocytes: 19 %, hemoglobin: 9.6 %, platelets: 271 000/mm3, prothrombin time: 18 seconds, international normalized ratio (INR): 1.45, blood urea nitrogen (BUN): 12 mg/dL, creatinine: 0.6 mg/dL, aspartate aminotransferase (AST): 123 IU/L, alanine aminotransferase (ALT): 44 IU/L, lactate dehydrogenase (LDH): 129 IU/L, CRP: 2.07. Complementary tests: HIV 191 (positive), HCV (non-reactive), HBV 0.4 (negative), treponema (negative), toxoplasma immunoglobulin M (IgM) 0.2 (negative).
Based on these findings, treatment consisting in the administration of rifampicin (150 mg) + isoniazid (75 mg) + pyrazinamide (400 mg) + ethambutol (275 mg) every 24 hours was started. Somehow, on the sixth day of treatment the patient experienced systemic deterioration and died.
Discussion
Regarding clinical manifestations, 10 to 20% of all tuberculosis cases are extrapulmonary; somehow, this percentage increases considerably (45%-75%) in patients with HIV infection10. The high frequency of extrapulmonary tuberculosis in HIV-infected patients is caused by their compromised immune system and the absence of immune response to Mycobacterium tuberculosis, which allows hematogenous spread of the bacteria and the subsequent bacterial invasion of one or multiple extrapulmonary tissues.
The clinical presentation of esophageal tuberculosis has not yet been determined, in fact it can be described as a spectrum of diffuse clinical features; however, a large proportion of esophageal tuberculosis cases reported in the scientific literature coincide in describing the presence of dysphagia and odynophagia, together with decreased appetite and involuntary weight loss, as shown in the cases reported by Garg R & Carter S in 201711 and Martins M et al. in 20169. Even so, the occurrence of such manifestations is not always well defined, resulting in misdiagnosis, as the cases in which the presentation occurs along retrosternal pain, epigastric pain and vomiting, according to Kumar et al., 201612. Due to its gastrointestinal location, the clinical manifestations of esophageal tuberculosis are frequently related to this system, such as purulent rectal discharge and hematemesis, as reported by Zuleta et al., 201213 and Manrique et al., 201414, respectively, although they are non-specific for its detection and diagnosis.
With regard to paraclinical tests, in general terms, reaching an extrapulmonary tuberculosis diagnosis is difficult due to the fact that this is a rare disease and there is little familiarity with its clinical presentation. In addition, inaccessibility to the infection sites and the low bacterial load also make even more difficult its diagnosis10. Upper endoscopy and the collection of biopsy samples during the procedure is the most useful diagnostic tool, even though there are no characteristic findings and pathological anatomy is often inconclusive9.
Usually, a solitary crater-like ulcer with raised edges located in the middle third of the esophagus is observed in upper GI endoscopy9,15; however, as shown above, there is no classic or typical lesion of esophageal tuberculosis. According to the scientific literature, esophageal endoscopic findings vary from superficial ulcers to raised lesions suggestive of neoplastic lesions, as well as strictures and fistulas(16, 17). In contrast, Hun Seo et al. reported that endoscopic findings of esophageal tuberculosis include ulcerative, granular or hypertrophied lesions, being linear ulceration with irregular margins and a grayish base with an irregular infiltrated edge in the mid-esophagus the most common finding7.
Furthermore, endosonography, also known as endoscopic ultrasound, is currently a test with a high impact as it allows observing characteristic findings of this disease, such as the subcarinal or periesophageal presence of heterogeneous matted lymph nodes adjacent to the esophageal pathology8,25 with a predominantly hypoechogenic26 or anechoic echotexture, particularly in the center and some hyperechogenic threads and foci (spots)7,8,25. Other typical findings include the thickening of the esophageal wall and the formation of masses disrupting the adventitia7,27.
Regarding treatment, the standard pharmacological regimen recommended for treating esophageal tuberculosis is the same than the preferred regimen for treating tuberculosis, that is, an intensive phase of four anti-tuberculosis drugs (rifampicin, isoniazid, pyrazinamide and ethambutol)10,13,14,22, plus a 4-month continuation phase of isoniazid and rifampicin14; however, streptomycin can be used instead of ethambutol23. Some authors affirm the use of a treatment regimen based on three drugs21: isoniazid, rifampicin and pyrazinamide17, and some others decide to add pyridoxine9. Generally, these patients have a good prognosis if an early diagnosis is made21,23 with treatment success rates of 90%14; somehow, immunocompromised patients, particularly those with AIDS17,21,23, fail to respond adequately to antituberculosis treatment regimens and may die due to the severity of the infection21,23. This is why it has been described that the efficacy of treatment depends on the status of the patient’s immune system13. In the case reported here, despite the patient received timely pharmacological treatment (rifampicin 150 mg + isoniazid 75 mg + pyrazinamide 400 mg + ethambutol 275 mg), his health condition worsened progressively and systemically resulting in his death.
Conclusion
Esophageal tuberculosis is a rare type of extrapulmonary tuberculosis. Despite its wide spectrum of clinical manifestations, dysphagia is one of the most representative. Coinfection with HIV has been frequent in recent years. Timely use of upper gastrointestinal endoscopy and esophageal ultrasound is very useful to suspect its diagnosis, which is confirmed through the histopathological analysis of the lesions.











 text in
text in