Introduction
Foreign body ingestion is one of the reasons for consultation in the gastroenterology service, being fish bone ingestion the most frequent. Long and sharp-pointed fish bones can cause complications in 1 % to 5 % of cases, requiring endoscopic and, in some cases, surgical extraction1. The perforation of the gastrointestinal tract by fish bone occurs in less than 1% of cases. The mortality rate is unknown, but death due to fish bone ingestion-related complications has been rarely reported2-5. In adults, its incidence is higher in people with intellectual disability or psychiatric disorders.
Poor dentition or inadequate chewing of food are clear risk factors. Dental prostheses fail to replace dentition, which affects the discriminative touch sensitivity of the oral cavity. Bad eyesight becomes another risk factor that often coexists in these people3. Approximately 50 % of ingested fish bones remain stuck in the esophagus and about 26 % reach the stomach; once in the stomach, they are usually expelled spontaneously; a low percentage remains stuck in the gastrointestinal mucosa due to they being sharp or having a large size. Fish bone impaction occurs most frequently in the prepyloric region and the ileocecal valve, since they are areas with a greater physiological stenosis4.
Intestinal perforation by fish bone ingestion diagnosis is frequently confused with some of the most common diseases, such as acute appendicitis or acute diverticulitis. Likewise, failure to make a causal association is also frequent due to the time usually elapsed between fish bone ingestion and the onset of symptoms, which are usually non-specific, including fever, malaise and abdominal pain, and later worsen until localized peritonitis occurs5. Endoscopy is a rapid diagnostic and therapeutic method that allows reducing morbidity. The removal of foreign bodies through endoscopy allows identifying the object, assessing the condition of the underlying mucosa, and verifying if the foreign body has caused any complication5.
In the case of bowel perforation caused by a fish bone there are basically two outcome possibilities: the perforation is located and bowel adhesion formation is triggered by the defense mechanisms of the peritoneal cavity, or peritonitis secondary to perforation occurs. Escherichia coli, Streptococcus, Enterobacter spp, Klebsiella spp, Enterococcus spp, Pseudomonas aeruginosa, Proteus spp, Staphylococcus aureus and Staphylococcus epidermidis are germs frequently found. Antibiotic treatment must be started before performing the surgery or the endoscopic procedure, and must be continued after the procedure and modified according to the results of the cultures and the evolution of the patient’s clinical condition5.
The case of a patient in which fish bone ingestion led to intestinal perforation and a gastric abscess that were successfully managed endoscopically and with antibiotic therapy is presented in this paper.
Clinical case presentation
This is the case of a 67-year-old female patient, without any relevant history of disease, who was admitted to the emergency department due to having experienced upper left abdominal pain, chills, lack of appetite and an approximately 6 kg weight loss for nearly 16 days. The following diagnostic studies were performed: initially, an upper gastrointestinal endoscopy showing a lesion in the extrinsic slope of the greater curvature, with a suspected 5cm subepithelial lesion in front of the extrinsic compression, with normal adjacent mucosa; an abdominal ultrasound showing images of stomach bed thickening with echogenic images that invade the light and the posterior acoustic shadow; a colonoscopy in which diverticulosis and a suspected superinfected tumor were reported, and for which an abdominal CT scan was performed, where an apparently solid exophytic mass with soft tissue density was found in relation to the greater curvature of the stomach. Based on these findings, gastrointestinal stromal tumors (GISTs) and foreign body reaction (Figure 1) were considered as possible diagnoses. Tumor markers were negative; leukocytosis and anemia were not reported in the complete blood count test, and the patient had elevated CRP levels (172.9).
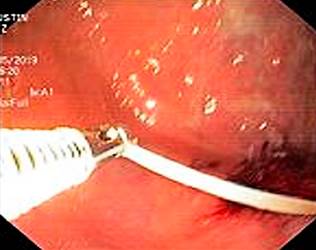
A second upper endoscopy was performed to determine the location of the mass and to take samples for performing biopsies. A severe thickening of the greater curvature mucosa with a large erythema was observed during the endoscopic procedure. Multiple samples for biopsy purposes were taken and, surprisingly, a 3.5 cm fish bone was extracted (Figures 2 and 3). Subsequently, antibiotic treatment for gastric abscess was started and the patient was asked again if she had eaten fish within the last month or months, however she denied it; a follow-up abdominal CT scan showed the size of the lesion had been reduced, as well as the presence of scarce fluid, thus drainage was not necessary (Figure 4). Antibiotic treatment was completed and there was no evidence of the abscess in a control abdominal ultrasound.
Discussion
Foreign body ingestion is a frequent reason for consultation in emergency departments, and the second most common indication for urgent upper endoscopy4-9. It has been described that 80-90% of foreign bodies can pass through the gastrointestinal tract without causing any complications3, and that only 1% can generate abscesses or perforations, being fish bones the main cause of such complications2-5. Unlike in the pediatric population, in which the ingestion of foreign bodies such as coins, buttons, batteries and plastic objects is frequent, in adults, the ingestion of organic bodies such as food pellets, fish bones and bones is more common6-10; this is due to the fact that most of foreign body ingestion cases in adults occur in those with dental prostheses, which alter the discriminative touch sensitivity of their oral cavities; besides, bad eyesight increases the risk of involuntary ingestion of a foreign body3.
The highest percentage of gastrointestinal perforations caused by fish bones occurs in the esophagus (approximately 50 % of cases); despite this, aortic rupture is a rare complication. Benítez11 reported two aortic rupture cases in which the patients died due to an aortoesophageal fistula, which reaches 22%; this is why making a timely diagnosis and identifying the location of the lesion is important, as this will contribute to improving the prognosis of these patients. Only 26% of ingested foreign bodies remain impacted in the gastric mucosa, and more frequently they can lead to complications such as abscesses, perforation and fistulas4,6,7,10. In children, ingested foreign bodies are usually located in the airway; besides, according to the location of the foreign body, symptoms may range from cough until respiratory distress. In these cases, bronchoscopy is indicated as it is a diagnostic, therapeutic, and safe procedure; this way, bronchoscopy has become the gold standard to extract foreign bodies in children, and delaying this procedure could increase the risk of complications12-14.
Reaching a timely diagnosis decreases the morbidity and mortality; in some cases, patients may present with atypical and non-specific symptoms that hinder the identification of the lesion, especially when there is no a clear history of foreign body ingestion. In the case reported here, symptoms were not very specific and the patient did not report having eaten fish within the last months prior to the onset of the symptoms, which led to a wrong diagnosis; furthermore, the time of onset of the symptoms was not immediate, since the patient had been experiencing them during approximately 16 days, but the time elapsed between fish consumption and symptoms onset was unknown. Garrido1 reported a similar case of gastric perforation caused by a foreign body of long permanence in a patient who presented with acute abdomen as initial symptom and in which the foreign body had been stuck for approximately 14 years and who subsequently required surgical management. In the first case reported by Benítez11, symptom onset occurred 12 days after the involuntary ingestion of a fish bone.
Using diagnostic aids is indispensable in any patient with suspected foreign body ingestion; plain X-rays are useful in cases of radiopaque objects ingestion to identify signs of perforation, such as the presence of free air under the diaphragm, in the mediastinum, the retroperitoneum or in cervical subcutaneous areas15. However, in fish bone ingestion cases, plain X-ray are not very useful, sincer fish bones are not radiopaque and they are hidden by soft tissues and the edema produced around the foreign body. CT, besides allowing the observation of non-radiopaque bodies, is very useful to identify the segment where the body is located. Due to its high sensitivity (100%) and specificity (93.7%) using it as the initial diagnostic test is recommended8,11,16.
Endoscopic procedures, both upper and lower endoscopies, are absolutely contraindicated when the occurrence of perforation is confirmed, as these are challenging and high risk procedures, especially when foreign bodies are sharp and can cause perforation and bleeding; another risk factor is the lack of fasting, which can lead to complications such as pulmonary aspiration, which in turn worsens the patient’s condition12. Somehow, conservative management of small perforations is well documented, as long as there are no open perforations or peritonitis. Endoscopic techniques have been perfected over time and, in this sense, these procedures have become more important in these cases, as they allow both the diagnosis and the removal of the foreign body. In general, these cases have been traditionally managed through surgery, which has been associated with very high morbidity and mortality rates (55% to 78%). However, the publication of cases in which endoscopy has been used has increased, as this procedure is less aggressive and has a high efficacy in solving this health problem4,9-11,15-18. According to Rosón et al.4, several cases of esophageal, gastric and, occasionally, bowel perforations were properly treated using conservative management. The type of antibiotic therapy is also important, in particular when abscesses occur. In the case reported here, the patient underwent gram-positive and gram-negative germs antibiotic therapy during 14 days, showing an adequate clinical response5.
Finally, in fish bone ingestion cases, conservative management by means of endoscopic extraction is frequent, since it is the treatment option with the lowest risk of morbidity and mortality. In the case abscesses and peritonitis are developed, establishing an antibiotic therapy regimen is necessary.











 text in
text in