Introduction
Early gastric cancer is defined as a cancer in which invasion is limited to the submucosa of the stomach on microscopic examination, regardless of lymph node involvement. This definition was proposed in 1971 by the Japan Gastroenterological Endoscopy Society1. For nearly 3 decades, it has been known that patients with mucosal lesions and those with submucosal invasion have a 100% and 90% 5-year survival rate, respectively. Also, survival rates of 99% and 73% have been described in patients with N0 and N0 cancers. The 10-year survival data are identical in patients undergoing surgical or endoscopic management for early gastric cancer2,3.
In 2018, there were more than 1 million new gastric cancer cases and 783 000 deaths attributed to this type of cancer in 2018, which makes gastric cancer the third leading cause of cancer death4.
The Paris classification (2002) is one of the most widely used gastric cancer classifications. In this classification, each type of cancer is predictive of the degree of submucosal invasion, which correlates with the risk of lymph node metastasis in gastric lesions. Lesions classified as Paris 0-I, 0-IIc and 0-III are associated with a higher risk of invasion of the submucosa (57 %, 37 % and 40 %, respectively) compared to 0-IIa and 0-IIb lesions (29 % and 20 %, respectively) (Table 1)5.
In Colombia, performing white light upper gastrointestinal endoscopy in any patient with uninvestigated dyspepsia is recommended if they show warning signs and symptoms; this procedure is also carried out together with chromoendoscopy using indigo carmine type stains to screen and detect premalignant lesions and early gastric tumors. Sydney protocol for stomach mapping and OLGA (operative link for gastritis assessment) protocol for conducting histologic studies6 are also used.
Clinical case
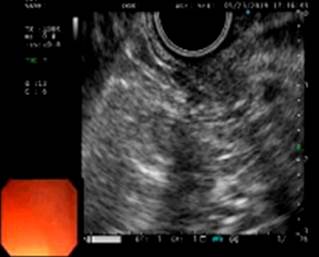
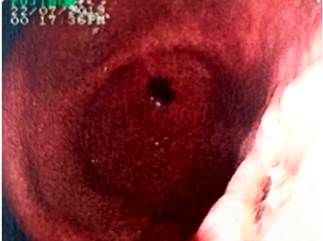
This is the case of a 54-year-old man from the rural area of the municipality of Socorro, Santander, who underwent an upper gastrointestinal endoscopy to assess the possible presence of a foreign body in the esophagus and in which an 8 mm diameter lesion in the antrum towards the greater curvature and highly compatible with a 0-Is early gastric neoplasia was incidentally found (Figure 1). According to the biopsies reports the lesion was compatible with well-differentiated adenocarcinoma. Taking these findings into account, the patient went to the Hospital Regional Manuela Beltrán, where he underwent a gastric endoscopic ultrasound in which involvement of layers I and II (up to the muscularis mucosae) was observed (Figure 2). Thus, the lesion was classified as uT1uN0, compatible with early gastric cancer. In addition, distant metastases or lymph node involvement were ruled out by means of an abdominal CT scan with contrast. Based on these findings, the patient was scheduled for endoscopic mucosal resection.
Description of the procedure and follow-up
A standard endoscopy tower with a single-channel esophagogastroduodenoscope was used. A sclerotherapy needle with 1:20 000 adrenaline solution was used to infiltrate the lesion at its base and an endoscopic resection was performed with a polygonal loop. A single complete piece (approximately 12 mm in greatest dimension) was resected (Figures 3 and 4).
The sample resected was sent for conducting a histopathological study. The pathology report read as follows: “Endoscopic resection of the lesion (stomach wall) with intestinal-type early gastric adenocarcinoma (early, superficial, well-differentiated) that extends up to the muscularis mucosae without running through it. Free lateral and middle edge margins” (Figures 5 and 6).
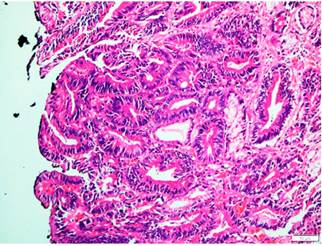
Figure 5 10x hematoxylin-eosin. The normal architecture of the gastric mucosa has been altered due to the presence of a malignant lesion made up of glandular and tubular elements, coated by high columnar epithelium focally pseudostratified with moderate pleomorphism and nuclear hyperchromaticism.
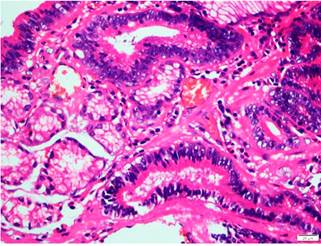
Figure 6 40x hematoxylin-eosin. Tubular glandular elements are seen in close proximity to smooth muscle fiber of the mucularis mucosae. Adjacent normal glandular components are observed.
The patient’s clinical condition successfully improved and he was discharged one day after the procedure was performed. In a follow-up upper endoscopy performed 2 months after endoscopic resection, scar tissue was found on the resection site and multiple samples were taken for biopsy purposes; there was no evidence of malignancy in any of these samples. The patient is currently asymptomatic and awaiting further endoscopic follow-up.
Discussion
Endoscopic mucosal resection is considered a safe alternative for the treatment of superficial lesions in which only the mucosa is involved; besides, it has a complete resection rate of more than 90%. Endoscopic submucosal dissection is also available, but this procedure is indicated for lesions larger than 20 mm and IIc and III deeper type lesions, since, despite being a more complex procedure, has a higher than 95% success rate. Endoscopic treatment-related complications are very rare, being bleeding and perforation the most frequent (up to 5%), while subcutaneous emphysema and pneumomediastinum are less frequent7-9.
The following endoscopic follow-up is recommended in patients treated for gastric cancer: performing an endoscopy every 3 to 6 months for 1 to 2 years, then every 6 to 12 months for 3 to 5 years, and finally, every year8.
Conclusions
The progress that has been made in terms of diagnostic and therapeutic endoscopy techniques, including endoscopic ultrasound and different endoscopic resection techniques, has made possible to treat early gastric cancer with low invasive intervention and high success rates. However, strict periodic endoscopic follow-up is required in order to monitor possible recurrences and reintroduce appropriate treatment plans.











 text in
text in