Introduction
Hemorrhoidal cushions or pads are structures composed of mucosal and submucosal tissue, rectal venous plexus, elastic connective tissue, and some smooth muscle fibers (corrugator cutis ani as a terminal part of the longitudinal muscle fibers of the rectum) that are inserted into the skin1-3. Their functions include maintaining fine-tuning of fecal continence, hermetic closure of the resting anal canal, and protecting the sphincter during defecation1,4,5. Although they are anatomically normal structures, the term hemorrhoidal disease (HD) refers to the symptomatic disease process6.
HD is a very prevalent clinical condition in the adult population and is a frequent reason for consultation in the emergency department. It is estimated that approximately 5 % of the adult population suffers from this disease, and it is much more frequent in patients over 50 years of age, reaching a frequency of up to 50 %7,8. In Colombia, there are no epidemiological registry studies of this disease.
The etiology of HD is not very clear; however, four theories have been proposed. The most accepted theory is the mechanical theory, in which prolonged defecation effort (poor bowel habit) and constipation cause dragging, stretching and damage of collagen fibers in tissues lining the anal canal9. The second theory points to the venous compression that obstructs blood return in the hemorrhoidal plexus caused by the uterus during pregnancy, at which time the hemorrhoids often become symptomatic. The third theory would explain the origin of external hemorrhoidal thrombosis, with vasodilation occurring with the consumption of some foods (fats, alcohol, condiments) and activities that increase intra-abdominal pressure (such as cough, straining when vomiting, squatting, or curling up for long periods), or local heat (sitting on hot surfaces); these events are frequently reported by patients with external hemorrhoidal thrombosis. Vasodilation and increased hemorrhoidal intravenous pressure cause elongation, endothelium shedding and exposure of subendothelial connective tissue, causing platelet aggregation and hemorrhoidal thrombosis. The fourth theory is vascular, which consists of the presence of arteriovenous fistulas and the absence of valves in the hemorrhoid bundles, which cause an increase in blood volume and elongation of the hemorrhoid bundles and the anal lining, being the indication for performing procedures such as selective hemorrhoidal artery ligation10. Many patients with external hemorrhoidal thrombosis report this as their first event and have no history or symptoms of internal hemorrhoidal prolapse.
Hemorrhoids are classified into internal and external and depend on their relationship with the dentate line5,6. Internal hemorrhoids are located proximal to the dentate line, are covered by columnar epithelium of endodermal origin, and are innervated by visceral fibers that do not transmit pain. Internal hemorrhoidal disease is classified into 4 degrees based on the level of hemorrhoidal prolapse with respect to the anal border; this classification is used to select and evaluate treatments11.
External hemorrhoids have a location distal to the dentate line, are covered by squamous epithelium derived from the ectoderm and their innervation is somatic, so they tend to be painful when thrombosis occurs6,12. Thrombosis of external hemorrhoidal bundles is the main complication of external hemorrhoidal disease (EHD).
The clinical presentation of external hemorrhoidal thrombosis is related to intense, continuous, and sudden onset of anal pain, accompanied by the sensation of a lump or mass in the anal region; in some cases, a few days later (48 to 72 hours) anal bleeding may occur when accompanied by necrosis of the wall of the thrombosed hemorrhoid bundle with subsequent partial evacuation of the thrombus.
Standard treatment for this complication in the first 72 hours is based on symptomatic medical management and, in the most severe cases, surgery. The latter consists of elliptical resection of the thrombosed external hemorrhoid bundle under local/regional or general anesthesia. The main indications and objectives of surgery are presented in Table 1.
Table 1 Indications and objectives of surgical management in thrombosed external hemorrhoidal disease.
| Medical indication: |
|---|
| - Thrombosed external hemorrhoid > 2 cm |
| - Severe pain that does not improve with analgesics |
| - Large anal mass that persists after 3 weeks |
| - Wall necrosis or bleeding of thrombosed EHD |
| - Patient’s desire for resolution of the mass sensation |
| - Repeated episodes (more than 3 episodes of thrombosis in 1 years, regardless of bundle size) |
| Objective: |
| - To improve anal mass |
| - To improve anal pain |
| - To avoid rethrombosis |
| - To return soon to daily activities |
| - To achieve low-cost treatment and easy in-office resolution |
The effects of this type of surgery are wound pain and a skin defect of variable size due to the resected skin ellipse, which may take 2 to 4 weeks to heal, as well as the availability of a surgical procedure room, which implies more costs and time required to solve this problem.
With simple thrombectomy, rethrombosis rates of up to 33 % measured at 24 months have been reported13-16. Thrombectomy with a wide skin incision and phleboextraction would reduce rethrombosis to less than 3 %, reduce postoperative pain, shorten healing time, and generate a prompt return to daily activities, while management is done in an agile and low-cost manner.
Thrombosed EHD that does not meet surgical criteria requires medical therapy. It may rage from the use of cold compresses in the first 3 days to sitz baths with warm water (between 38-40 °C) in the following 15 days, in which anti-inflammatory agents and skin astringents such as calendula or magnesium sulfate may be included. Stool softeners, avoiding poor bowel habits, discontinuation of vasodilator or perianal skin irritating foods, and the use of phlebotonics and oral analgesics are also recommended.
Materials and methods
A search was performed in the institution’s electronic medical records database. Patients diagnosed and treated for thrombosed external hemorrhoidal disease from January 1, 2014, to December 31, 2016, by the coloproctology service of the Hospital Militar Central were identified. Complete medical records were obtained from 197 patients diagnosed with a diagnosis of first episode of thrombosed EHD. The demographic characteristics of the population, the type of therapy (surgical and medical), and outcomes such as pain, bleeding, and infection (early complications) up to 30 days after initiation of treatment were described.
A review of the medical records with a minimum follow-up of 12 months after the initial treatment was carried out to assess the rate of retrothrombosis, healing time, and late complications (up to 1 year after the start of treatment) such as bleeding, infection, and chronic pain.
The standard surgical therapy provided in the coloproctology service of the Hospital Militar Central for the management of thrombosed external hemorrhoidal disease was thrombectomy with wide skin excision plus phleboextraction, which consists of the following steps (Figure 1).
Preparation: Besides signing the informed consent, the procedure must be explained to the patient, as well as its objectives and benefits. When the patient is motivated and calm, the procedure is started. The following items must be available: 15 blade scalpel, Kelly forceps, pre-cut gauze, and sterile gloves.
Exposure of the anal region: The patient is placed in a jackknife position, buttocks are separated with adhesive tapes (cloth tape) or manually by an assistant in Sims’ position.
The external thrombosed hemorrhoid bundle is digitally retracted, achieving eversion and exposure throughout its circumference to facilitate its fixation and approach.
Prior to asepsis and antisepsis, without anesthesia, using a 15 blade scalpel and its blade pointing upwards (to reduce pain), the area of greatest necrosis is incised by unroofing in a longitudinal and radial direction (with the anus as the center) over 90% of the surface of the hemorrhoid bundle. An incision should be made for each thrombosed external hemorrhoid bundle.
The clot is removed with digital pressure.
With a Kelly forceps, the hemorrhoidal vascular plexus is clamped and extracted by selective traction, similar to the phleboextraction performed in the treatment of venous insufficiency of the lower limbs.
Hemostasis and placement of anal gauze plug are verified.
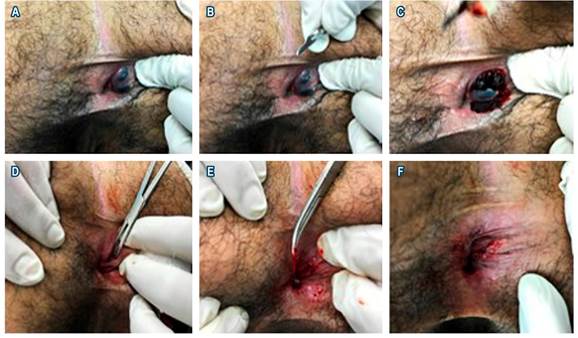
Figure 1 Thrombectomy plus phleboextraction. A. Digital fixation and eversion of 2 thrombosed external hemorrhoid bundles. B. 15 blade scalpel and its blade pointing upwards. C. Longitudinal incision of 90 % of the surface of each of thrombosed hemorrhoid bundle, compression, and removal of the clots. D. Search and gentle and careful clamping of the external hemorrhoidal vessels. E. Extraction of external hemorrhoidal vessels by traction using the Kelly forceps. F. Inspection of the area of thrombectomy and phleboextraction, local pressure in case of bleeding. A gauze is applied over this region at the end of the procedure, and it must be maintained for 6 hours before being removed. The patient may use a gauze in the anal region for 2 or 3 more days, and it must be changed 2 or 3 times a day. Oral acetaminophen every 8 hours for 2 days is prescribed.
Results
A total of 197 medical records of patients diagnosed with thrombosed external hemorrhoidal disease were evaluated; 142 (72 %) of them underwent medical therapy and 55 (27.9 %) were treated surgically according to the indications proposed in Table 1. No significant differences were found between sex and age. The mean follow-up time after initiation of medical or surgical therapy was 16 months. The recurrence rate was 7.2 % and the recurrence interval was 29.2 months in the surgical group. No infectious complications were evident during the follow-up in both groups of patients (Table 2).
Discussion
Thrombosed external hemorrhoidal disease is a common surgical condition. Despite the fact that a number of treatment options have been used, there is a surprising lack of prospective comparative data on therapy and long-term effects. Some possible explanations include its management being regarded simple with a predictable outcome, a lack of innovation in novel management techniques that make it unappealing as a subject of study, and the inability to conduct prospective studies due to population size. Furthermore, due to its high recurrence rate, thrombectomy for the management of thrombosed EHD has historically had a negative reputation and little acceptance among surgeons.
Because the outcomes of medical versus surgical therapy are not easily comparable, it has been suggested that the time of pain resolution in medical therapy cases and the resolution of pain, anal mass, bleeding, wound healing, patient satisfaction, costs, and time required by the patient and surgeon to solve the problem in surgical therapy cases should be used to decide which method to use13.
In individuals undergoing surgical therapy, complete pain remission occurs around the fourth day after the procedure, as opposed to conservative management, in which pain may last up to day 2413. Our data show that pain in 81.9 % of patients undergoing surgery disappears 72 hours after the procedure, whereas pain persists in up to 92.2 % of patients in the conservative therapy group. Additional medical management strategies, such as addition of topical nitroglycerin or nifedipine, have been proposed 13.
Cavcić et al.17, Greenspon et al.13, and Perrotti et al.18 have proposed different strategies for the medical management of thrombosed external hemorrhoids, mainly using stool softeners, local or systemic analgesics combined with topical nitroglycerin or nifedipine, and have shown better results than analgesic use alone.
There is no evidence in the literature that conservative therapy improves outcomes in early consultation cases following the onset of symptoms; this practice appears to be based on judgments passed down through the years.
In a retrospective study comparing conservative versus surgical therapy of thrombosed external hemorrhoids, Greenspon et al.13 showed a recurrence rate of 25.4 % in the conservative therapy group, with an average recurrence time at 7.1 months, in contrast to the surgical therapy group, in which a recurrence of 6.3% was observed, with an average recurrence time of 25 months. With the data extracted from our population with the described technique, it was possible to decrease the recurrence rate and increase the time of recurrence, even considering that it is a second independent episode.
Conclusions
Thrombectomy with a wide skin excision plus phleboextraction improves results with a lower recurrence rate and faster healing, making it an efficient technique at a low cost. This is an office procedure, which quickly and efficiently resolves the feeling of mass, pain, and bleeding without the need to be taken to an operating room. It also has the advantage of not requiring local/regional or general anesthesia, and outcomes are achieved along with a reduced healing time and perianal pain, a rethrombosis rate of 3% measured at 24 months, and excellent overall patient satisfaction. This is a procedure with an easy, reproducible, and low-cost technique. It would be worthwhile to validate the technique by designing a randomized controlled clinical study, comparing the ellipse resection of the thrombosed external hemorrhoid bundle with broad thrombectomy plus phleboextraction, and to give consistency to our findings with the experience of other centers that can implement the technique and confirm the proposed benefits.











 text in
text in 



