Key concepts
The endoluminal functional luminal-imaging probe (EndofLIP) measures intra-balloon pressure, cross-sectional areas of the esophagus, and esophagogastric junction (EGJ) by impedance, as well as motility by planimetry.
The EGJ is opened by means of balloon distension using the functional luminal image probe (FLIP), allowing the measurement of its diameter and distensibility; at the same time, secondary peristalsis is created, allowing motility assessment.
The FLIP technique is used for conditions such as achalasia and eosinophilic esophagitis. However, its usefulness is less clear in gastroesophageal reflux and in intraoperative assessment of EGJ during fundoplication.
EndoFLIP allows diagnosis achalasia and its subtypes.
EndoFLIP has clinical utility as a diagnostic tool in patients with esophagogastric junction outflow obstruction, ineffective esophageal motility, and absent contractility in whom achalasia is clinically suspected within the spectrum of esophageal motility disorders and high-resolution esophageal manometry (MAR) is inconclusive.
Normal EndoFLIP findings may be used to rule out esophageal motility changes during endoscopy, which may reduce the need for high-resolution manometry to assess some patients.
Normal esophageal response to distention on EndoFLIP during upper GI endoscopy may indicate normal esophageal motility function.
Recent indications for its use include gastroparesis and alterations of anorectal function.
Introduction
The FLIP technique is based on the principle of impedance planimetry and allows direct measurement of intraluminal cross-sectional areas (CSA) and the assessment of intraluminal diameters, geometric lumen profiles, and changes in pressure, volume, and distensibility, that is, the biomechanical properties of the wall. It also provides a three-dimensional image of the esophageal lumen and the EGJ1,2. EndoFLIP (functional endoluminal image probe) is a system that measures the esophagogastric junction distensibility index (EGJ-DI) and secondary esophageal peristalsis through high-resolution impedance planimetry in real time 3-5.
The initial evaluation of impedance planimetry as a test was carried out in the late 1980s and the first studies were carried out with the devices available in the 1990s6. Then, in the early 2000s, several pioneering groups led by Mittal, Pandolfino, and Shaker attempted to address several questions about the use of this device in the assessment of sphincter distensibility and competence, and its biomechanical properties. In 2003, impedance planimetry became more practical as was used as an option to evaluate sphincter distensibility, leading to the first studies to evaluate sphincter dynamics in the EGJ7,8. It also made it easier to measure distensibility and detect the narrowest point at the EGJ.
The American Gastroenterological Association (AGA) published an expert review in 2017 summarizing the field4 and, to date, there have been more than 100 peer-reviewed articles on the subject.
EndoFLIP device and system
The device consists of a measurement catheter, the FLIP 1.0 module, and the FLIP 2.0 module3 (Figure 1). There are 2 models of FLIP catheter: EF-325, 8cm long, with 16 planimetric impedance sensors spaced every 5 mm; and EF-322, 16cm long, with 16 sensors spaced 1 cm intervals. The FLIP measuring segment is positioned inside a balloon catheter attached to a syringe located at the distal end of the catheter. A solid-state electrode that measures pressure is found at the most distal end of the balloon, and an infusion port, through which a conductive fluid is infused, is located at the proximal segment. The EF-325 catheter provides information on EGJ distensibility and CSA, while the EF-322 catheter provides secondary peristaltic patterns of the esophageal body in addition to the EGJ metrics (Table 1)3,4,9,10.
Figure 1 EndoFLIP device. A. EndoFLIP module with FLIP 1.0 system. B. FLIP system 2.0. C. Measuring catheter.
Table 1 FLIP catheter types, features, and protocols for use3
| Catheter setup | EF-325 | EF-322 |
|---|---|---|
| Balloon length | 8cm | 16cm |
| Sensors | 16 separated by 0.5cm intervals | 16 separated by 1cm intervals |
| Location | The central part of the catheter should be located at the EGJ | 2-3 distal sensors must be positioned below the EGJ |
| Baseline placement | 20 mL | 30 mL |
| Wait time at each fill | 15 seconds | 15 seconds |
| Balloon fill protocol | 30 mL, 40 mL, and 50 mL | 40 mL, 50 mL, 60 mL, and 70 mL |
| Wait time at each fill | 30 seconds | 60 seconds |
| Measurements | EGJ-DI and intrabag pressure | EGJ-DI diameter, intrabag pressure and esophageal contractility patterns |
Adapted from: Savarino E et al. Am J Gastroenterol. 2020;115(11):1786-1796.
EndoFLIP interpretation
Measurements and normal values
The FLIP 1.0 module has an 80 mL syringe operated by an electro-hydraulic pump, which is controlled via the unit’s touch screen. The infusion of a conductive fluid into the balloon allows the excitation electrodes, at either end of the balloon, to emit a continuous low electrical current and measure voltage through the paired impedance sensors (Ohm’s Law: Voltage = Current x Resistance). Through voltage, the FLIP 1.0 calculates the CSA in each range of sensor pairs, allowing the estimation of diameter at 8 or 16 points along the distal esophagus. The pressure electrode simultaneously measures intrabag pressure during distension. Distensibility is calculated from the simultaneous measurement of pressure and CSA. These data are shown as a three-dimensional representation of the esophageal lumen (Figure 2)3,4,10.
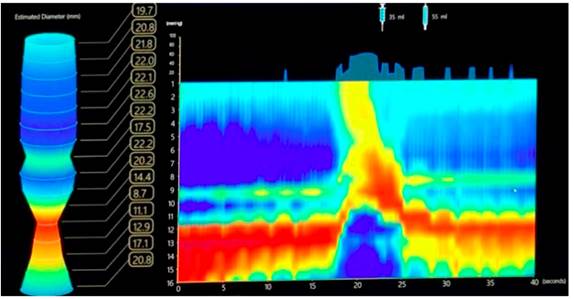
Figure 2 EndoFLIP performed with a 16cm EF-322 catheter. On the left, FLIP 1.0 module with 3D representation of the esophagus and its diameters. On the right, FLIP 2.0 with topographic image of the esophagus.
In the FLIP 2.0 module, diameter data along the axial plane of the esophagus are interpolated and color-coded on a hot/cold scale to generate FLIP topography, in which small diameters are noted by red tones and large diameters by blue tones (Figure 2). Using the EF-322 catheter in this module, the changes in the pressure-diameter ratio along a space-time continuum are visualized, which are useful to describe motility patterns of the distal esophagus in response to distension3,4,11,12.
The prospective study by Carlson et al.13 evaluated 20 asymptomatic volunteers (age: 23-44; 14 women) using a 16cm FLIP positioned across the EGJ and distal esophagus (and repositioned at the proximal esophagus in 8 subjects also) during upper gastrointestinal endoscopy with sedation9. FLIP data were analyzed with a customized MATLAB program that generated FLIP planimetry plots and calculated the EGJ-DI and distensibility plateaus of distal and proximal esophageal body. Distension-induced esophageal contractility was also evaluated. These 20 asymptomatic subjects had an EGJ-DI >2.8 mm2/mm Hg, a maximum EGJ diameter of >18 mm, a distal esophageal body distensibility plateau >18 mm, and a pattern of repetitive antegrade contractions was demonstrated in response to distension.
Then, the normal parameters of esophageal distensibility are EGJ-DI >2.8 mm2/mm Hg and distensibility plateaus >18mm. Regarding planimetry, antegrade contractions, which occur in a repetitive pattern with balloon esophageal distension, are considered physiological (Table 2).
Table 2 Interpreting EndoFLIP results
| Normal | Indeterminate | Abnormal | |
|---|---|---|---|
| Esophageal distensibility (FLIP 1.0 and 2.0) | |||
| - EGJ distensibility index | > 3 mm2/mm Hg | 2-3 mm2/mm Hg | > 2 mm2/mm Hg |
| - EGJ diameter | > 18 mm | 13 - 18 mm | < 13 mm |
| Esophageal distensibility (FLIP 2.0) | |||
| - Distension-induced contractility | Repetitive antegrade contractions | Indeterminate patterns of contractility | Repetitive retrograde contractions Absent contractility |
Interpretation of obtained values
Considering the results obtained after the measurement, the contractile response of the esophagus to volumetric distension can be classified into 4 categories (Figure 3):
Repetitive antegrade contractions when there are ≥3 consecutive antegrade contractions.
Repetitive retrograde contractions, if there are ≥3 consecutive retrograde contractions, which is an abnormal response often associated with esophageal spasm, achalasia, or post-surgical esophagogastric junction outflow obstruction
Absent contractility, which suggests aperistalsis, type I achalasia, scleroderma, and significant ineffective esophageal motility.
Other contractile patterns that do not meet the criteria for the previous 3 categories, called diminished or disordered contractile response, which probably represents a milder form of motility dysfunction.
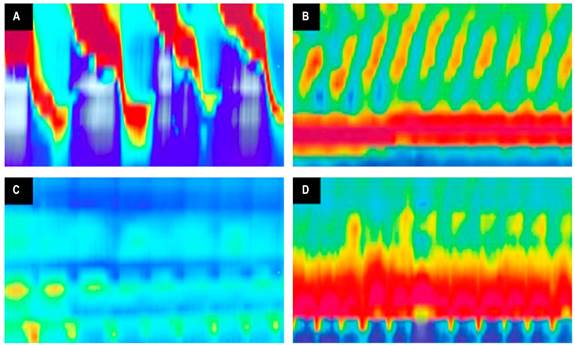
Figure 3 Esophageal contraction patterns in FLIP 2.0. A. Repetitive antegrade contractions. B. Repetitive retrograde contractions. C. Absent contractility. D. Undetermined contractile pattern.
These results can also be used in comparative studies of esophageal diseases such as achalasia and eosinophilic esophagitis to facilitate the application of FLIP planimetry in clinical practice.
The American Gastroenterological Association (AGA)14 recommends using FLIP along with HRM to diagnose alterations in esophageal motility in patients with obstructive esophageal symptoms and borderline findings on HRM (conditional recommendation, poor quality of evidence), and in patients in whom manometry could not be completed due to failure in catheter placement despite multiple attempts, for example.
The study by Deprez et al.15 showed that most EndoFLIP studies identified a subgroup of patients with achalasia and were useful in the intraoperative assessment of therapeutic efficacy in achalasia. They also considered the use of EndoFLIP in the esophageal body (esophageal planimetry), as well as in other esophageal diseases such as gastroesophageal reflux disease (GERD), eosinophilic esophagitis, and in sphincter regions other than the EGJ, such as the pylorus and the anal canal, but confirmatory studies are needed.
Clinical utility of EndoFLIP
Achalasia
Achalasia is a primary esophageal motor disorder that can result in impaired lower esophageal sphincter relaxation16. Diagnosis is based on symptoms such as dysphagia, regurgitation, weight loss, chest pain or heartburn, which must be present for at least 1 year so as not to be confused with pseudoachalasia, as indicated by the Seoul and European Union guidelines17,18, plus an endoscopy without mechanical obstruction at the EGJ, and HRM compatible with some of the subtypes of achalasia defined in the Chicago Classification v 4.016,19. However, there are patients who do not tolerate HRM, so the American College of Gastroenterology guidelines are the first to consider the usefulness of EndoFLIP as a diagnostic tool in achalasia20.
As mentioned above, EndoFLIP provides important information about patients with achalasia, such as esophageal and EGJ distensibility, by measuring the cross-sectional area of the gastroesophageal junction (CSA-EGJ) through impedance sensors plus pressure (P) inside the balloon. The values should be measured when the balloon is distended with 6 mL of conductive solution2,21. The CSA-EGJ/P ratio is the EGJ-DI, whose normal value is 3.0-9.0 mm2/mm Hg. It is considered abnormal between 0-2.0 mm2/mm Hg and in gray zone between 2.1-3.0 mm2/mm Hg21. EGJ-DI tends to reduce in conditions associated with obstruction or alteration of EGJ relaxation; abnormal values are found in 91 % of patients with achalasia, but if the value is extended to the gray area, it improves its sensitivity and is observed in 97 % of patients with achalasia22. There is another parameter that is also relevant, namely the diameter of the EGJ, which was <16 mm in 96% of patients with achalasia. Therefore, having an EGJ-DI ≤3.0 mm2/mm Hg plus an EGJ diameter <16 mm confirms the presence of achalasia when FLIP is used, since these characteristics are not observed in healthy people9,22.
As previously mentioned, distension causes contractions in the esophageal body, which are measured by FLIP version 2.0 (Figure 3)2,21. As with HRM, these contractions have been able to typify achalasia into 3 types, which is well known to have prognostic value after treatment17,18,20. The esophageal contraction patterns visualized by EndoFLIP have a sensitivity/specificity of 45 %/95 % for the diagnosis of type 1 achalasia, 72 %/73 % for type 2 achalasia, and 93 %/82 % for type 3 achalasia23,24. Therefore, it is useful in patients whose HRM does not meet all the Chicago Classification v 4.0 criteria due to altered peristalsis but have a normal integrated relaxation pressure (IRP), and in whom provocative maneuvers and esophagram also fail to confirm the presence of achalasia25-27.
EndoFLIP has also been shown to be useful in the treatment of achalasia, both in the intraoperative phase and during patient follow-up28. During the procedure, whether pneumatic dilatation, Heller myotomy, or per-oral endoscopic myotomy (POEM), EndoFLIP is the only method that measures esophageal distensibility in real time, which has been shown to be useful in predicting a symptomatic response defined with Ekcardt <3 points, when the value of the EGJ-DI is ≥3.0 mm2/mm Hg. It is even better than the normalization of the IRP and the decrease of the lower esophageal sphincter pressure measured with HRM21,28,29. In addition, the study by Campagna et al. showed that EGJ-DI is not affected during general anesthesia30. In this way, EndoFLIP allows to establish, if required, a greater dilatation or length of the myotomy during the procedure until achieving an increase of EGJ-DI; thus, a better response to treatment is obtained and the risk of gastroesophageal reflux decreases31,32.
GERD
Anti-reflux barrier function with impaired EGJ is a contributing factor in the pathogenesis of GERD, suggesting the usefulness of FLIP in assessing EGJ distensibility for the diagnosis of GERD. However, data have not demonstrated a reliable diagnostic threshold for the EGJ-DI in GERD.
As EGJ incompetence may contribute to the pathophysiology of GERD in some patients, it is reasonable to suspect that FLIP may help identify greater EGJ distensibility (i.e., larger EGJ diameters at lower distention pressures). Nevertheless, study results have been inconsistent. Consequently, since EndoFLIP measures EGJ distensibility, it has been hypothesized that it could improve knowledge of the pathophysiology of GERD and aid in diagnosis.
Carlson et al.33 reported in their study that increased EGJ-DI contributes to reflux. Using FLIP, the objective was to evaluate the esophageal response to distension in patients undergoing esophageal pH monitoring. The EGJ incompetence is an important factor related to the development of GERD, so measuring alterations in EGJ distensibility may help characterize patients with GERD. The study also aimed at evaluating the association of esophageal acid exposure with esophageal response to distension among patients undergoing GERD evaluation with wireless esophageal pH monitoring and FLIP, showing that, although EGJ distensibility was not consistently associated with acid exposure of the esophagus, distension-induced impairment of contractility was associated with increased exposure of the esophagus to acid34.
However, the use of EndoFLIP in the diagnosis of GERD is controversial, as studies conducted to evaluate its utility in a large-scale population have found differences in distensibility between erosive reflux disease, non-erosive reflux disease, and control groups. In patients with erosive GERD, CSA and DI were higher compared to the control group. When comparing the results of HRM with 24-hour pH monitoring, the IRP was lower in the non-erosive reflux group than in the other groups, and 24-hour pH monitoring showed a significant difference in all groups. Moreover, due to its high cost, EndoFLIP may not be recommended for all patients with GERD. However, it may be useful in some cases, for example, before a treatment such as anti-reflux surgery, or in refractory GERD, as it is believed to be an additional diagnostic method when information of distensibility is needed33,34.
EGJ-DI in patients with GERD showed a significant increase compared to the control group, regardless of the presence of erosive esophagitis. Measuring EGJ distensibility using EndoFLIP is useful in the diagnosis of GERD. Besides ambulatory pH-impedance, HRM, and endoscopy tests, EndoFLIP can aid in the diagnosis of GERD based on objective evidence and classification of the GERD subtype.
FLIP can also identify the presence of hiatal hernias and differentiate the lower esophageal sphincter (LES) from the crural diaphragm (Figure 4). LES distensibility was reported to be higher in the presence of hiatal hernia compared with asymptomatic control subjects35. Finally, using FLIP 2.0 planimetry, Carlson et al.33) observed that esophageal exposure to abnormal acid was associated with an altered contractile response to esophageal distension volume, corroborating the well-known concept that esophageal exposure to acid is dependent on acid clearance mechanisms. However, data on the diagnostic utility of FLIP in GERD remain incomplete, especially as the FLIP metrics in GERD show a considerable overlap with metrics observed in healthy controls.
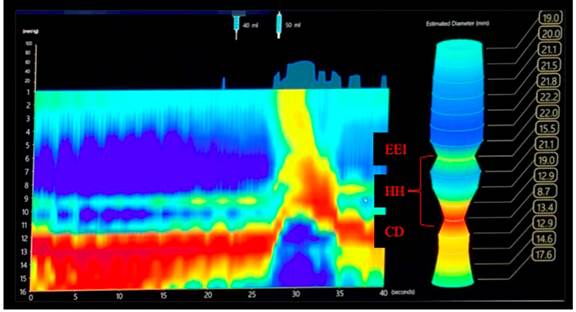
Figure 4 Hiatal hernia in FLIP 2.0. DC: diaphragmatic crura; HH: hiatal hernia up to 21 mm in diameter.
In summary, the role of FLIP for the physiologic evaluation and treatment of GERD remains appealing, but the level of evidence is low, and FLIP is currently not recommended for its diagnostic or therapeutic approach. Further studies are needed to confirm the usefulness of FLIP in GERD and to develop metrics to predict severity and response to treatment after anti-reflux treatment.
Dysphagia and esophagogastric junction outflow obstruction
Non-obstructive dysphagia is one of the main symptoms studied to establish alterations in esophageal motility, and HRM is used to this end. Defining the type of disorder of the lower esophageal sphincter, either achalasia or esophagogastric junction outflow obstruction (EGJOO) is essential. It should be noted that HRM has limitations, and, consequently, FLIP plays an important role in the evaluation of non-obstructive dysphagia, as it may be useful in suspected clinical achalasia with normal IRP, inconclusive HRM findings, and in patients who do not tolerate the HRM, among others1.
EGJOO is a heterogeneous group of disorders defined by the Chicago Classification v4.0 based on the following HRM findings: elevated IRP (supine and upright), ≥20 % elevated intrabolus pressure (supine), and not meeting criteria for achalasia19,36. Both conditions are classified within the lower esophageal sphincter disorders37) and are considered a common but nonspecific motility pattern38 that may be caused by functional obstruction, mechanical obstruction (mainly in patients with a history of fundoplication, hiatal hernia, and stenosis), medications (mainly opiates), or artifacts36.
The gold standard for the diagnosis of EGJOO is HRM. Although its prevalence is unknown, it has been reported that it can vary between 3 % and 21 %, with a mean age of presentation between 56 and 67 years, mostly in women. The most common symptom is dysphagia, followed by typical and atypical GERD symptoms; it should be noted that 5 % of patients are asymptomatic, but are diagnosed based on HRM findings. Its clinical significance is not exact: the impact on quality of life, natural history and optimal treatment are not yet fully known, but it can progress to achalasia, so it may be considered an early stage of achalasia. It is not known which patients may progress to achalasia or which will have an early resolution36; therefore, it is not yet clear who benefits from achalasia-type treatment (dilation, Heller myotomy, or POEM) and who will be managed expectantly, with medications or behavioral therapy. It should be noted that up to 50 % of patients may have a spontaneous resolution when the etiology is non-mechanical 37,38.
It is believed that FLIP using impedance planimetry could become a promising tool for the diagnosis and treatment of EGJOO36,37, as it assesses the luminal diameter and corresponding distension pressure in the esophagus during volumetric distension38, which gets its value through the distensibility index37.
FLIP has been compared with HRM in patients with dysphagia. It has been found that FLIP detects major motility disorders more accurately3; in addition, it analyzes the reaction of the esophageal body to balloon distension such as repetitive anterograde contractions, repetitive retrograde contractions, and absent contractility, which are useful to establish achalasia as a differential diagnosis36. However, FLIP has been found to be useful in identifying patients with EGJOO who are more likely to benefit from achalasia-type therapy (patients with EGJ-DI <2 mm2/mm Hg, with adequate post-treatment response) and allows patients with distensibility >3 mm2/mm Hg to receive successful medical management38. This serves as a post-treatment follow-up strategy, in which it is determined that an improvement in the EGJ-DI with a value >3 mm2/mm Hg would be considered normal, showing a successful response to treatment, and confirming that the efficacy of lower esophageal sphincter modification is determined by the improvement lower esophageal sphincter distensibility, a factor that is optimally evaluated by EndoFLIP3. It has been reported that the lower the EGJ-DI, the higher the IRP, which may be useful in differentiating patients with more significant outflow obstruction that require intervention37. The ability of EndoFLIP to assess both EGJ distensibility and esophageal contractility could confirm the clinical relevance of isolated “abnormalities” of IRP in HRM3; thus, this is a tool to improve diagnosis when manometric findings are uncertain and, additionally, to select management and follow-up strategies3,37,38.
EndoFLIP and gastroparesis
Clinically diagnosing gastroparesis can be challenging as symptoms, patterns, and severity are poorly correlated with gastric emptying. Pyloric dysfunction has been identified as unusually prolonged and intermittent pyloric contractions known as pylorospasms. Recently, pyloric distensibility assessment using the EndoFLIP has been validated as a complementary measurement to sphincter pressure in gastroparesis. Measurement of pyloric distensibility can be easily achieved by placing a probe under fluoroscopic guidance through the endoscope. Whether or not anesthetics impact pyloric distensibility has not yet been investigated.
In most studies, pyloric distensibility has been inversely correlated with gastric emptying15. Furthermore, pyloric distensibility correlates negatively with symptoms of gastroparesis, including nausea, sense of fullness, and early satiety. This contrasts with the measurement of gastric emptying, which correlates poorly with symptoms or quality of life, suggesting that pyloric distensibility may be a clinically relevant tool in a subset of patients with gastroparesis to better identify one of the underlying mechanisms involved in gastric retention.
Endoscopic interventions that have shown to be effective in the treatment of gastroparesis with pyloric dysfunction as the primary etiology include endoscopic botulinum toxin injection, endoscopic gastric peroral pyloric myotomy (G-POEM) and, to a lesser extent, pneumatic balloon dilatation39,40. In 30-50% of patients with gastroparesis, higher pressure and lower elasticity of the pyloric sphincter has been demonstrated in comparison with healthy volunteers; moreover, pyloric characteristics observed with EndoFLIP provide relevant information regarding symptoms, gastric emptying, and prediction of response to treatment41,42.
The first endoscopic treatment option in gastroparesis with pyloric dysfunction refractory to pharmacological and non-pharmacological treatments is the application of botulinum toxin under direct visualization. Desprez et al.15 evaluated pyloric distensibility with EndoFLIP in 35 patients with gastroparesis before botulinum toxin injection and found 19 patients with altered pyloric distensibility and 16 with normal pyloric distensibility; 3 months after the procedure, the total symptom score, quality of life, dyspeptic symptoms and gastric emptying improved in patients with impaired pyloric sphincter distensibility compared to those with normal distensibility, who had no improvement. This leads to the conclusion that evaluation with EndoFLIP predicts the response to treatment in patients with gastroparesis who are candidates for botulinum toxin injection42.
G-POEM is a recent endoscopic therapy for refractory gastroparesis. The first procedure was performed in 2013 and consists of a submucosal dissection of the pyloric ring, which has gained ground due to its efficacy and safety43. Vosoughi et al.44 demonstrated that EndoFLIP is a diagnostic tool that can predict which patients will respond to G-POEM therapy; after evaluating 37 patients treated at 5 centers due to refractory gastroparesis who underwent G-POEM and had EndoFLIP measurements (CSA, balloon pressure and distensibility index), they compared clinical success at 1 year and gastric emptying at 3 months, finding decreased CSA was a predictor of success following G-POEM44.
Pyloric balloon dilation as a treatment for patients with refractory gastroparesis has limited evidence40. However, in patients who have undergone G-POEM or laparoscopic pyloroplasty and remain symptomatic, recent studies have shown the benefit of balloon dilatation, since persistent symptoms may be related to incomplete myotomy or stricture due to fibrosis. Jehangir et al.45 included 13 patients with refractory severe gastroparesis who underwent pylorotomy and pyloroplasty and subsequent pneumatic balloon dilatation after assessment of pyloric characteristics with EndoFLIP. It was observed that dilatation improved symptoms in one third of the patients and a lower pyloric distensibility before dilatation with EndoFLIP was documented in responding patients45.
Fundoplication and bariatric surgery
Although the diagnostic utility of FLIP in GERD may remain controversial, additional studies have helped to evaluate the physiologic components related to the pathophysiology of GERD. Since patients with fundoplication appear to have reduced distensibility of the EGJ compared to controls, FLIP may be a useful tool to aid in anti-reflux surgeries such as fundoplication. Several studies demonstrated the feasibility of intraoperative use of FLIP during fundoplication and a consistent reduction in EGJ distensibility immediately after fundoplication. Reduction of EGJ distensibility after transoral incisionless fundoplication (TIF) has also been reported.
EndoFLIP has proven to be a useful intraoperative adjunctive procedure to perform EGJ calibration, as it allows real-time measurement of CSA, decreased distensibility and increased intraluminal pressure of the EGJ as a predictor of fundoplication success. It also allows evaluating its length to avoid excess distensibility, which is one of the pathophysiological mechanisms of GERD, and guiding the intraoperative modification of the technique when Nissen fundoplication is very tight35,46, which could not be previously quantified in the objective measurement of crural closure and when fundoplication was performed in most cases with a bougie without a more accurate measurement47. Measurements are made at the beginning, after intubation, followed by mobilization or reduction of the hernia, after crural closure, and after fundoplication48.
Su et al.49, in a prospective study evaluating the use of EndoFLIP during hiatal hernia repair and fundoplication in 175 patients with a 24-month follow-up after treatment, found that patients with a final EGJ-DI <2.0 mm2/mm Hg had more abdominal distension and dysphagia compared to those with a EGJ-DI ≥2.0 mm2/mm Hg (p = 0.040 and p = 0.025, respectively), which is more noticeable at 24 months (43 % vs. 12 %; p = 0.03). Moreover, patients with a final distensibility between 2.0 and 3.5 mm2/mm Hg had lower symptomatic index scores compared with a final distensibility <2.0 or >3.5 mm2/mm Hg (p = 0.042).
This device has also been approved for guiding therapy in bariatric surgery procedures, allowing standardization of lumen size and volume, thereby improving the results of the technique in real time4. Furthermore, its use is critical in strictures after sleeve gastrectomy with an incidence of up to 4% and causing symptoms such as reflux, epigastric pain, dysphagia, and regurgitation. EndoFLIP has proven useful in measuring lumen geometry before and after dilatation, which allows establishing a response to therapy with larger post-dilatation diameters (19.9 ± 2.9 mm) and EGJ-DI 21.3 ± 1.0 mm2/mm Hg50.
Eosinophilic esophagitis
Eosinophilic esophagitis is a chronic immune-mediated esophageal disease, characterized by esophageal symptoms (predominantly dysphagia and food bolus impaction) and eosinophilic inflammation51. Chronic inflammation is thought to progress to esophageal fibrosis, leading to narrowing of the lumen and loss of mural distensibility52. These remodeling consequences of eosinophilic esophagitis are the main determinant of symptoms and are usually assessed endoscopically53. Prevention and reversal of remodeling is an important goal of treatment3.
FLIP is used in eosinophilic esophagitis to assess esophageal narrowing and mechanical characteristics of the esophageal body, including measuring esophageal remodeling of fibrosis. The distensibility plateau is identified by measuring the narrowest CSA of the esophageal body and the corresponding intra-balloon pressure during volume distension2. Narrow luminal diameters correlate with lower distensibility plateau values54, which in turn correlate with lamina propria fibrosis and the occurrence of food bolus impaction. Although impaired distensibility can be observed in patients with eosinophilic esophagitis of all ages, it decreases with age and disease duration. Impaired distensibility is partially reversible, especially after successful treatment with steroids or diet; in contrast, distensibility does not change in patients with failed therapy55.
When symptoms persist despite optimal therapy, serial assessment of distensibility and luminal diameter using FLIP could provide an objective outcome metric that may indicate the need to intensify therapy. Similarly, in the presence of histologic healing with persistent symptoms, FLIP may reveal other mechanisms underlying clinical symptoms, such as increased esophageal spasms or reduced distensibility due to chronic esophageal fibrosis, which could indicate the need for esophageal dilation. Since this can be reliably measured with FLIP, FLIP distensibility measurements are gaining importance as secondary endpoints in eosinophilic esophagitis trials and mechanistic studies. Therefore, EndoFLIP measurements are an easy adjunct for the assessment of esophageal diameter and distensibility in eosinophilic esophagitis3.
FLIP may be superior to existing approaches of monitoring disease activity by upper endoscopy with biopsies because sampling may be inconsistent. Esophageal fibrosis measured endoscopically has been found to be inaccurate compared to fluoroscopy2.
Therapeutic use of FLIP
EsoFLIP
EsoFLIP is made up of a rigid balloon that can perform dilation with volume-controlled filling of the balloon. EsoFLIP dilation balloons are indicated for clinical use in adult patients to dilate the LES in achalasia (hydraulic dilation) and to dilate esophageal strictures following esophageal surgery or caused by primary gastroesophageal reflux disease, or radiation.
Although EsoFLIP and EndoFLIP use the same impedance planimetry technology and have several similarities, they are different devices with specific clinical applications: while EsoFLIP provides therapeutic dilation, EndoFLIP is a diagnostic device, as mentioned above. To facilitate dilation, EsoFLIP is available in 2 sizes: at a diameter of 30mm (ES-330) or 20mm (ES-320). However, because the fill volume of the balloon is controlled, dilation to smaller sizes than the maximum dilation size (e.g., 16 or 25mm) can be achieved with control of the fill volume, as well as real-time visualization of the 3D display.
Likewise, this technology requires endoscopic visualization of the site to be dilated. The measurement should be made from the dental arches, a wire is passed, the endoscope is withdrawn and the EsoFLIP catheter is introduced. If no wire is used, the measurement is made with the endoscope from the dental arches to the area to be dilated; when the endoscope is withdrawn, the EsoFLIP catheter is introduced, and its location is confirmed again with endoscopic visualization. Both techniques can be confirmed on the FLIP display56,57.
The real-time assessment of dilation by impedance planimetry using EsoFLIP, as well as dilation with volume-controlled filling of the balloon, offers several potential advantages over other balloon dilators. Although clinical data associated with this new device is still limited, the safety and feasibility of EsoFLIP balloon dilation have been reported56,57.
Advantages of EsoFLIP dilation
Dilation without fluoroscopy
Visualization of the EsoFLIP waist through real-time impedance planimetry may facilitate the performance of dilation, in particular for 30mm dilatations, without the need for fluoroscopy. Moreover, if the dilator balloon is moved, the position can be observed and corrected upon in real-time.
Control of dilation size (diameter)
Dilation size is established by via the volumetric control of balloon filling. Real-time measurement at the balloon waist allows for controlled dilation to any diameter to achieve the desired effect. This contrasts with the use of single-size or even multi-size dilator balloons that may require the use of multiple balloons if the desired effect is not achieved.
Measurement of stricture size and assessment of dilation effect
EsoFLIP dilation provides the possibility of objectively measuring stricture size and assessing the response to dilation immediately after the procedure. Studies in which EndoFLIP is used have demonstrated its utility in measuring stricture size, especially in eosinophilic esophagitis55,57-59. Additionally, measurement of EGJ-DI with EndoFLIP in achalasia patients facilitates the assessment of response to treatment (myotomy or pneumatic dilation) with associations to clinical outcomes at the time of treatment57,60,61. EsoFLIP 330 is also useful to perform EGJ dilation in patients with achalasia and success, defined as an Eckardt score <3, was obtained in 63 % of patients, with no major adverse events62,63.
Limitations of EsoFLIP dilation
Some features of the device may limit the ease of the procedure, such as the lack of ability to pass through-the-scope, the external guidewire that requires removal prior to dilation, the need for an external pressure monitor, and the time required to fill and empty the dilator balloon. Also, as expected due to the novelty of the device, there are few studies reporting on the use or efficacy of EsoFLIP57.
The study by Schnurre et al.63 found good efficacy in both subjective and objective short-term treatment outcome after EsoFLIP dilation in patients with previously untreated achalasia. These findings suggest that EsoFLIP is a promising dilation technology that should be further studied in a larger controlled setting and with a longer follow-up.
Conclusion
EndoFLIP is a new technology available in our country with a wide clinical utility, mainly as a complementary diagnostic tool, when esophageal manometry with swallowing tests and complementary imaging scans (esophagogram or barium sulfate) are not sufficient to confirm functional disorders of esophagogastric junction outflow obstruction. Furthermore, it has a therapeutic role in the dilation of achalasia, esophageal stricture, and during fundoplication surgery. Its clinical usefulness in other disorders such as eosinophilic esophagitis, gastroesophageal reflux, gastroparesis, among others, is yet to be determined.











 text in
text in 



