Introduction
Mesenteric cyst is a rare tumor that may appear in multiple intra-abdominal locations. It was first reported at the autopsy of an 8-year-old boy by the Italian anatomist Benevieni in 1507; then, in 1800, Tillaux performed the first surgical resection of this type of lesion1.
Its current incidence is approximately 1 per 100 000 adult patients and 1 per 20 000 children attending a hospital2. The most frequent location of these lesions is the mesentery of the small intestine (60 %), followed by the ascending colon (24 %), and the retroperitoneal region (14.5 %)3. Their clinical presentation is diverse; they may be completely asymptomatic with a subsequent appearance of nonspecific symptoms such as intermittent abdominal pain, abdominal distension, diarrhea, or palpable abdominal mass, acute abdominal or intestinal obstruction symptoms, which are directly related to the size of the lesion4.
A classification system was proposed by Perrot et al., which is still in force, in which mesenteric cysts are classified according to their origin as follows:
lymphatic (simple or lymphangioma);
mesothelial (simple, benign, or malignant cyst);
enteric (intestinal duplication cysts or enteric cyst);
urogenital;
dermoid; and
non-pancreatic pseudocysts (infectious or traumatic)5.
Different imaging studies, such as ultrasound and computed tomography (CT), are used for diagnosis. The former shows solid lesions, but no anatomical details, while the latter, which is the most used, shows cyst contents, wall size, presence of septa and, if contrast medium is added, information on the relationship of the mass with vascular structures or other adjacent structures2,6.
On the one hand, the treatment of choice is surgery, and the laparoscopic approach is preferred, as it has advantages over other procedures such as achieving complete cyst enucleation, post-surgical recovery, and a low recurrence rate. On the other hand, techniques such as aspiration or marsupialization are not recommended due to the high rates of recurrence and superinfection7.
The present article reports the clinical case of a 38-year-old man with no significant history, who attended the emergency department after experiencing an oppressive abdominal pain of mild intensity, without acute abdomen criteria on admission, for a day. It was decided to request a total abdominal ultrasound, in which a giant retroperitoneal cystic mass was observed. Further studies were performed, including an abdominal CT with intravenous contrast agent, endosonography and magnetic resonance imaging of the abdomen, which led to the diagnosis of mesenteric cyst. Therefore, it was decided to perform mass resection with a laparotomy approach due to the size and location of the lesion, with histopathological confirmation of mesenteric cyst.
Objective
To present a case report on giant mesenteric cyst managed by the surgery service, reviewing its diagnostic features, treatment, and outcome.
Materials
A case report study that also includes a bibliographic review of its diagnostic and therapeutic strategy. A search was conducted in databases such as PubMed for publications containing the terms giant mesenteric cyst, with the most relevant articles being chosen.
Results
The patient was a 38-year-old male patient, resident in Colombia, with no known personal history, who consulted after experiencing mild abdominal pain on the left flank and left iliac fossa, with no other associated symptoms, for a day. He stated that he had taken oral analgesics without clinical improvement, therefore he decided to go to the emergency department. On admission, his vital signs were within normal parameters and the abdominal examination did not reveal signs of peritoneal irritation, therefore, it was decided to start symptomatic management. Due to the persistence of the symptoms, laboratory tests were requested, and the results yielded normal values (Table 1). A total abdominal ultrasound was requested, reporting a passive lesion behind the left kidney of 160 x 140 x 90 mm, multiseptated, and associated with left pyelocaliceal dilatation. Based on these findings, it was decided to perform a CT scan of the abdomen as a complementary study.
Table 1 Laboratory tests on admission
| Test | Result | Reference values | |
|---|---|---|---|
| Complete blood count |
|
|
|
| Urine cytology |
|
|
|
| Creatinine | 0.5 mg/dL | 0.6- 1 mg/dL | |
| Urea nitrogen | 12 mg/dL | 6- 20 mg/dL | |
| Amylase | 34 UI/mL | 0-137 U/L | |
| Carcinoembryonic antigen | < 0.50 ng/mL | < 40 ng/mL | |
| Total bilirubin | 1 mg/dL | 0.1- 1.2 mg/dL | |
| Indirect bilirubin | 1 mg/dL | 0- 0.7 mg/dL | |
| Alkaline phosphatase | 68 U/L | 50-136 U/L | |
| Calcium | 1.187 mmol/L | 1-2.4 mmol/L | |
| HbA1c | 5.3 % | < 5.6 % | |
| PT: | 10.4 sec. | 10-13.5 s | |
| PTT: | 25.2 sec. | 25-35 s | |
| INR | 0.98 | < 1 | |
| ALT | 37 U/L | 30-65 U/L | |
| AST | 31 U/L | 15-37 U/L | |
| α-fetoprotein | 1.92 IU/mL | < 15 IU/mL | |
| CA 125 | < 4 | < 35 | |
ALT: alanine aminotransferase; AST: aspartate aminotransferase; CA 125: cancer antigen 125; HbA1c: glycosylated hemoglobin; INR: international normalized ratio; PT: prothrombin time; TTP: partial thromboplastin time.
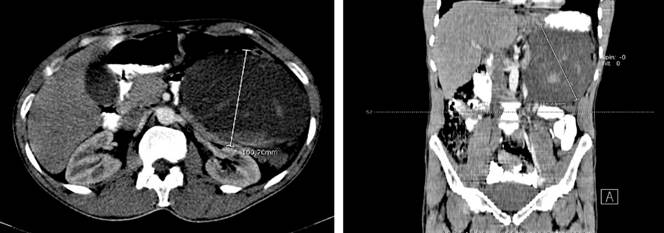
The CT report showed a voluminous collection projected on the left retroperitoneum, which displaced the colon and ipsilateral kidney, with heterogeneous content and hyperdense areas inside, forming a level, suggesting a collection with different evolutionary stages of bleeding, with measurements of approximately 154 x 135 x 100 mm for an estimated volume of 180 mL. The lesions exerted a mass effect on the body of the pancreas and projected towards the transcavity of the omentum. After injecting the contrast agent, no areas of enhancement were observed for this lesion. The pancreas appeared thin at the body and tail levels due to the compressive effect exerted by the previously described mass, normal intestinal loops, kidneys, and normal excretory system (Figures 1 and 2).
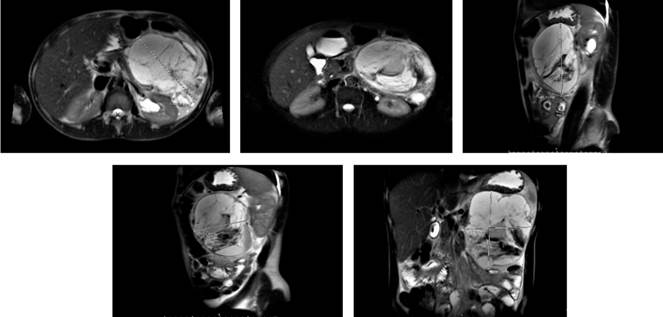
The patient was evaluated by the general surgery service, which requested tumor markers (Table 1) to rule out a neoplastic lesion of the pancreas and magnetic resonance imaging to define the surgical plan. The report showed an irregular multiseptated lesion of the body and tail of the pancreas of 87 x 130 mm that extended to the spleen, without cleavage plane, and the stomach moved to the upper and anterior side (Figure 2). A high-resolution chest CT was also performed as an extension study, which was normal.
Given the MRI findings, it was necessary to rule out that the lesion was dependent on the body or tail of the pancreas. Therefore, a biliopancreatic endoscopic ultrasonography was performed, finding a large septated multi anechoic lesion with well-defined edges of approximately 110 x 90 mm in the pancreaticoduodenal space with displacement of the left kidney and a suitable cleavage plane with the pancreas in the region of the head, body, and tail without focal lesions; the rest of the study showed no alteration.
Based on the above findings, a mesenteric cyst was diagnosed, and the patient was scheduled for surgery. An exploratory laparotomy was performed in which a tumor was found in the mesentery of the transverse colon toward the splenic flexure measuring 150 x 200 mm with a solid cystic appearance (Figure 3), firmly attached to the spleen, tail of the pancreas and colon. Consequently, resection of the mesenteric cyst, splenectomy, distal pancreatectomy, and partial left colectomy with intestinal stapled side-to-side anastomosis were performed. Due to a blood loss of approximately 1200 mL and hemodynamic instability, the patient required transfusion of intraoperative blood products and infusion of vasopressors. His post-surgical evolution was adequate, and he was discharged 8 days after the surgical procedure. An outpatient post-surgical follow-up was performed two months later, and the patient’s condition was normal.
The last pathology study reported:
Macroscopic description: en bloc resection of the large intestine, measuring 19 x 2.5 cm; an irregular brownish lesion measuring 15 x 11 cm was identified toward the transverse mesentery of the colon, with a smooth external surface; after cutting, it was found cavitated and multiloculated, with extensive hemorrhagic change and hemorrhagic fluid outflow, measuring 9 x 4 cm and firmly attached to the body of the pancreas. The spleen weighed 150 g and measured 12 x 9 x 2.5 cm; there were no visible macroscopic lesions in the sections.
Microscopic description: colon wall without evidence of lesion. In the sections of the intestinal wall, tumor, and tumor area in relation to the pancreas, a lesion characterized by the presence of fibrous septa without epithelial lining with mixed infiltrate consisting of polymorphonuclear and plasmacytes associated with extensive recent bleeding was observed ; the lesion was found to be attached to the mesentery of the colon and to the peripancreatic adipose tissue, without interstitial involvement. In the spleen section, splenic tissue was identified with preserved architecture and an adequate ratio of red and white pulp, without histopathological lesions.
Diagnosis:
Discussion
Mesenteric cysts have a low global incidence of approximately 1 out of 100 000 adults seeking medical care, and they primarily affect people in their second to third decades of life with a male-to-female ratio of 2:18,9. These lesions can affect any part of the mesentery and represent 7 % of all abdominal cysts10. They have mainly benign characteristics, but up to 3 % of these lesions may be malignant. The cause of mesenteric cysts is unknown; however, the most accepted theory, proposed by Gross, suggests that it is a benign proliferation of mesenteric lymphatic tissue associated with a lack of communication of the lymphatic and venous systems, which may be idiopathic or secondary to previous surgical procedures, infection, neoplastic disease, endometriosis, or pelvic inflammatory disease11.
The diagnosis of mesenteric cysts is difficult to achieve, as it commonly mimics other conditions such as pelvic inflammatory disease, pancreatic pseudocyst, and aortic aneurysms12. There are three types of diagnostic suspicion: nonspecific abdominal symptoms, incidental radiological findings, or acute abdomen13. Some reported complications include intestinal obstruction, bleeding, rupture, and twisted bowel or volvulus14.
Imaging studies are important for preoperative diagnosis. Varied imaging modalities provide different clinical benefits, although CT scan and MRI are more useful for detecting an accurate location as well as their interaction with other neighboring structures14. A definitive diagnosis is established through surgical excision and histopathological examination of the mass. All these considerations were taken into account in the management of our case.
Surgical resection of the cystic mass is the mainstay of treatment and has shown to prevent recurrence and malignant transformation15,16. The laparoscopic approach is the safest and reduces postoperative pain, shortens the length of hospital stay, and improves recovery rates. In our case, laparoscopy was not possible due to the size of the lesion, but epidural analgesia was used, and early mobilization measures were taken to prevent complications. Simple aspiration is not recommended due to higher rates of recurrence and infection.
Conclusions
Mesenteric cyst is a rare and mostly benign condition, with nonspecific clinical presentation and delayed diagnosis. Its diagnostic and characterization process is based on radiological studies, ranging from ultrasound to magnetic resonance imaging. The treatment of choice is surgical, thus avoiding recurrences. The clinical case presented here had abdominal pain that did not improve. In this case, imaging studies revealed a retroperitoneal mass that was removed via laparoscopic surgery; the patient had a favorable postoperative course with no complications related to the procedure or the histological report described.











 text in
text in