Introduction
Solitary rectal ulcer syndrome is a rare, benign disease characterized by a variety of symptoms, clinical findings, and histopathological abnormalities. It was first described by Cruveihier in 1829, who reported 4 cases of rectal ulcers1. However, the term solitary rectal ulcer was coined by Lloyd-Davis at the end of the decade of 19302.
Its incidence is uncertain but is estimated to be 1 in 100 000 individuals per year, and it is considered an underdiagnosed condition. It is mistaken for other disorders such as inflammatory bowel disease (IBD) and neoplastic lesions; it occurs more frequently in the third decade of life in men and the fourth decade in women, with a slight predominance in women3.
Description of the clinical case
The case was a 31-year-old female patient, who presented with colicky pain and abdominal distension associated with multiple episodes of abundant rectal bleeding in March 2016.
A colonoscopy was performed in May 2016, finding a mucosal irregularity of 5 cm in diameter located in the anterior wall of the rectum on an erythematous base, with thickened folds and friability. The histopathological result reported a malignant tumor lesion consisting of moderately differentiated adenocarcinoma. She was referred to the oncology service for resection of the tumor lesion; however, performing a new rectosigmoidoscopy was considered. No malignancy was identified in the new histopathological study. Due to this new finding, oncological management was not performed. After 2 months without any symptoms, rectal bleeding recurred, and an endoscopy was performed again (Figure 1). An ulcer was observed at 6 cm from the anal margin; histopathology revealed reactive crypt changes and fibrosis without malignant changes. She received symptomatic treatment and was in remission for several months. In March 2017, another endoscopy was performed due to the recurrence of symptoms, finding transverse rectal ulcer of 6 cm covered by fibrin with thickened and hard edges, as well as a histopathology result indicating chronic colitis (Figure 2).
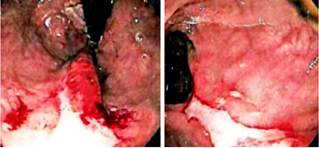
Figure 1 Colonoscopy performed in September 2016. A 3 x 1 cm ulcerated lesion with defined edges and covered by fibrin without bleeding is observed at 6 cm from the anal flange, with histological findings of rectal mucosa with reactive crypt changes, fibrosis, and vascular congestion in the lamina propria without malignant changes.
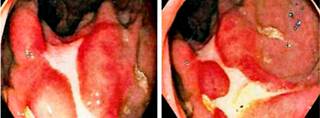
Figure 2 Colonoscopy performed in March 2017. A 6cm transverse rectal ulcer covered by fibrin with thickened and hard edges was identified; the rest of the study was normal up to the distal ileum. Biopsy of the ulcer revealed chronic colitis.
The patient attended a follow-up endoscopy in 2019, which revealed a 3 x 2 cm ulcer covered with fibrin located 5cm from the anal canal. The biopsy reported a chronic ulcer with reactive changes and fibrosis. She was diagnosed with Crohn’s disease and was treated only with prednisolone cycles, improving rectal bleeding.
She was first assessed in our institution in August 2019 after 11 days of rectal bleeding, with 10-12 episodes daily, severe abdominal pain and fever. On physical examination, she was found hemodynamically stable, with signs of dehydration. Due to her medical history, it was decided to start management for IBD with a new cycle of prednisolone. A review of previous pathology studies, conducted in May 2016, was requested and an ileocolonoscopy was performed (Figure 3).

Figure 3 Rectosigmoidoscopy performed in August 2019. An alteration of the structural pattern with loss of vascular pattern, erythematous mucosa, edema and nodularity, slight friability with mucosal retraction and scarring at distal level was observed from the pectineal line to the transverse folds of the rectum.
Ileocolonoscopy identified solitary rectal ulcer, with no lesions in the ileal mucosa. Histopathology samples from May 2016 were evaluated by institutional pathologists, in which mucosa with tissue artifacts was found with focal presence of cell groups with cytologic and architectural atypia (Figure 4), so adenocarcinoma was initially suspected based on the inflammatory reactive changes. However, the lesion was not represented in immunohistochemical sections. In the new samples obtained at our center, hyperplastic mucosa was found without dysplasia, as well as ulcer fragment without tumor lesions (Figure 5); no architectural changes, microorganisms, granulomas, or clear fibromuscular replacement of the lamina propria were observed.
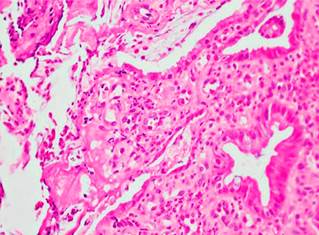
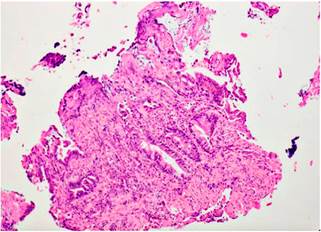
Figure 4 Fibroinflammatory replacement of the lamina propria. Hematoxylin and eosin stain (H&E): 10 X.
After discussing the case during a multidisciplinary board of specialists, a defecography was performed, which was highly suggestive of rectoanal intussusception as the cause of the persistent ulcerated lesion; therefore, it was concluded that the patient presented with a solitary rectal ulcer syndrome.
Discussion
Solitary rectal ulcer is a rare condition and approaching it may be challenging given its similarity to other conditions. Regarding diagnostic difficulty, it should be emphasized that a directed and up-to-date medical record is essential, with clear details of risk factors and clinical history. In this case, when the patient was interviewed again, long-standing symptoms of constipation and limitation of rectal evacuation were observed, which were valuable to suspect rectal intussusception.
The term solitary rectal ulcer is not the most appropriate term for this syndrome since ulcers are found in only 40 % of patients. About 20 % have solitary ulcers and the rest of the lesions vary in shape and size and may include anything from hyperemia of the colonic mucosa to a broad-based polypoid lesion3.
Its pathogenesis is not completely elucidated, but there are several factors that can contribute to its development. The 4 theories raised in this regard could be summarized as follows4:
Prolonged straining during bowel movements in a patient suffering from chronic constipation may lead to direct trauma to the mucosa.
Self-induced instrumentation trauma that occurs when people try to eliminate impacted stool by rectal digitation.
Paradoxical or uncoordinated contraction of the puborectalis muscle associated with increased intrarectal pressure, resulting in ischemia and ulceration.
Rectal prolapse and intussusception that can lead to localized vascular trauma.
The syndrome also overlaps with anxiety disorders and obsessive-compulsive disorder4.
Clinical manifestations are variable and may be absent in up to 26 % of patients5. Some symptoms include rectal bleeding, copious mucoid discharge, prolonged excessive straining, perineal and abdominal pain, feeling of incomplete defecation, constipation and, rarely, rectal prolapse6,7. Endoscopic findings may vary from mucosal erythema to single or multiple ulcers and polypoid lesions. In most patients, lesions are located in the anterior rectal wall within 10 cm of the anal margin but can also be located in the anal canal or sigmoid colon.
Histological features include fibromuscular obliteration of the lamina propria, extension of muscle fibers, and hypertrophy of the mucosa with alteration of the glandular crypt architecture. There are other minor microscopic changes such as crypt distortion and reactive epithelial atypia, which may lead to misdiagnosis since similar findings can be seen in IBD and neoplasms. However, the diffuse arrangement of collagen fibers in the lamina propria and abnormal smooth muscle fiber extensions are sensitive markers to differentiate solitary rectal ulcer syndrome from other conditions at the histological level.3
The assessment of the patient with solitary rectal ulcer syndrome can be supplemented to evaluate the existence of functional disorders or rectal prolapse, thus enabling a better therapeutic approach. Hence, tests such as defecography and endoscopic ultrasound may be performed. Defecography allows to visualize different stages of defecation, which determine the presence of intussusception or prolapse of the mucosa. It may also demonstrate occult prolapse, as well as impaired relaxation of the puborectalis muscle and incomplete or obstructed defecation. Endoscopic ultrasound is an alternative to defecography that allows evaluating the thickness of the internal anal sphincter, as well as intussusception.8
The management of solitary rectal ulcer syndrome depends on the severity of symptoms and the presence of rectal prolapse. In asymptomatic patients, observation and education are the mainstay of the approach. In non-severe symptomatic cases, treatment is based on the use of bulk-forming laxatives and biofeedback therapy to correct abnormal pelvic floor behavior. Surgery is reserved for patients with rectal prolapse or with severe symptoms that do not respond to conservative treatment9. Surgical options include local excision, rectopexy, or fecal diversion.
Other types of treatments have been described and, although they do not have sufficient evidence, have an impact on the symptomatic management of patients. They include topical treatments with sucralfate, salicylate, corticosteroids, sulfasalazine, and mesalazine10.
The differential diagnosis of solitary rectal ulcer syndrome includes IBD, ischemic colitis, infectious proctitis, and malignant neoplasms. The prognosis is difficult to determine since it is a chronic condition, with a significant impact on the quality of life of individuals. Many of them will present with persistent symptoms of anorectal dysfunction, even after an adequate therapeutic approach.
Conclusion
This syndrome is characterized by painful and difficult defecation, a feeling of incomplete evacuation, and sometimes lower gastrointestinal bleeding. Its presentation is variable and has a low incidence; a comprehensive diagnosis must be achieved through endoscopic studies, radiology, and histological confirmation, considering differential diagnoses.
In the present case, a multidisciplinary approach along with the coloproctology and pathology services, as well as the expansion of the clinical history of the patient based on the results of the defecography and a literature review, led to provide an adequate diagnosis and treatment. The existence of this syndrome should be recognized and reported as a result of the diagnostic approach used in this case.











 text in
text in