According to the Esophagectomy Complications Consensus Group, an anastomotic leak is a “full-thickness defect involving the esophagus, anastomosis, staple line or conduit” (1. Anastomotic leaks, after surgery, have been associated with higher morbidity and mortality rates, especially if there is a delay of more than 48 hours in diagnosis 2,3. The failure in the repair of an esophageal leak is the main cause of death of these patients. Adequate drainage, reoperation with pleural or diaphragmatic flaps and derivation (esophagostomy) are treatment options for severe, uncontrolled leaks. Recently, attention has been drawn to minimally invasive options to treat anastomotic leaks (4, including esophageal stenting, which have shown to be effective in the initial treatment of esophageal anastomotic leaks offering low comorbidities, with results that can be compared to those of other treatments5-9.
Stents are placed via endoscopy in order to avoid or treat surgical complications and offer a shorter patient stay (6. Even with a good stenting technique (10, complications continue to occur. The stent migration, the patient’s pain, the erosion of neighboring tissue, and the persistent leak are some of the most common complications. The type of stent and the placement method may vary depending on local availability, the physician’s preferences and the characteristics of the patient, which can contribute to different complication risks. It is believed that there are several factors that contribute to the failure of the stent, such as poor patient selection, incorrect stent diameter, longer stent stay, low functional activity before the surgery, development of a esophageal fistula, prior exposure to chemotherapy, delay on the diagnosis of the leak 48 hours after its occurrence, advanced age, increased fistula size and severe comorbidities (6,7,9.
This issue presents the Ovalle et al. research, of unicentric and retrospective nature, who for 11 years studied 11 patients suffering post-surgical esophagogastric anastomotic leaks and received 14 stents subsequently assessing their technical and clinical outcomes. The technical success was 100% and the clinical success reached 72.2% with a fistula closure of 63.5% (7/11 patients). Complications came to 27.7% (3/11) and they were only related to stent migration (1 case with 3 migrations and 3 stentings).
When performing a retrospective analysis of the publications from the last decade regarding the treatment of esophagogastric leaks with stents, certain procedure adjustments took place for their management, with a diameter increase of the stents, total versus partial coatings and a greater availability and expertise at the time of placement (10. With regard to stent diameters, a clinical study took place testing larger diameters (megastents) for the treatment of this type of complications with a tendency to a lower migration rate compared with historical controls treated with a conventional stent (11.
This study, just like several other publications, shows great diagnosis and treatment differences for esophagogastric leaks; different diagnostic methods are described, and in the current series, the esophagogram is the most frequent (7/11 patients); the size of the defect is not emphasized, there are different instructions for stenting, different stenting times as well as the initial leak diagnosis, various stent types (size, total or partial coating), the use of other endoscopic techniques such as EndoVac or in this case the OVESCO clip, and the post-treatment management protocol for radiological studies, which may range from a simple x-ray to a tomography.
These questions cannot be answered with any retrospective series and a randomized study can hardly be implemented in order to compare the use of stents against another group with no endoscopic therapy, due to ethical considerations. Currently, studies are focused on defining the role of the stent compared to other endoscopic options such as fibrin sealants, endoclips or vacuum therapies such as EndoVac or a combination of these, like in the case of the series, successfully treated with OVESCO plus stent.
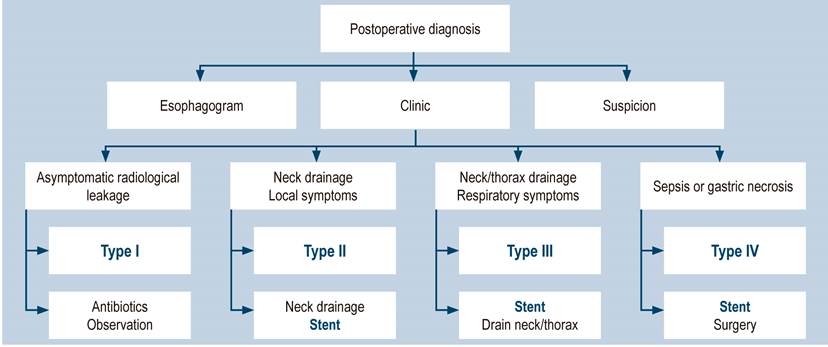
A standardized diagnosis and treatment protocol is necessary for patients clinically suspected of leaks after the esophagectomy or gastrectomy, which would allow obtaining better results. Recently, we have presented at the National Surgery Conference our experience with the treatment of 22 patients with esophageal fistulas after an esophagectomy and the gastric ascent in neck, with a 100% technical success and a 64%12 fistula closure, the proposal for the treatment is included in Figure 1.
The optimal time for stenting has been suggested, which is within the first 24 hours after the leak diagnosis, with the purpose of limiting infectious complications and favoring healing (13. An agreement on the optimal time for stent removal in order to achieve the closure of the esophageal leak has not been reached. Recent studies show that the necessary time varies from 4 to 12 weeks (14.
While clinically stable patients with minor contained leaks can be treated in a conservative manner with IV antibiotics and a possible percutaneous drainage, patients with mediastinal and pleural contamination can now often save the conduit utilizing esophageal stents, endoluminal vacuum or other sutures and endoluminal clips. The benefit of continued enteral nutrition with endoluminal stenting shall be considered against greater rates of complications and migration of the stent in comparison with EndoVac. Although EndoVac has shown promising results for anastomotic leak closure, further studies on its use in patients with complex leaks are justified. As medicine continues to evolve, more novel ways to address such complications will be found and someday anastomotic leaks will be completely avoided.
The study limitations include its retrospective nature, with results reporting data from a single tertiary center, with a possible bias on the selection, which hinders the generalization for daily practice, as well as the small number and heterogeneous patient population. However, it only reflects patients with postoperative esophagogastric leaks and addresses clinical and endoscopic factors associated with the endoscopic resolution of leaks. As final corollary and revisiting the title, the virtue or success (in medio virtus) of the treatment for such complex cases lays in the rigorous selection of the patient, the stent or other endoscopic means in order to achieve, as in this Ovalle et al. series, good results.











 texto en
texto en