Introduction
Hiatal hernia is a frequent pathology in the general population; however, its reported incidence does not exceed 5 % since only a low percentage of patients present associated symptoms1. This symptomatology can vary according to the size of the hernia and the severity of the pathology; those that present symptoms mostly improve with medical treatment.
According to the management guidelines of the Society of American Gastrointestinal and Endoscopic Surgeons (SAGES)2, surgery is performed when there is no resolution of symptoms with medical management or due to the presence of a giant symptomatic hiatal hernia (defined as > 5 cm), which represents approximately 5 % of hernias3. Other authors suggest treating hiatal hernia once the diagnosis is made regardless of the presence of symptoms due to the risk of presenting them; this has been reported by up to 30 %. Additionally, the risk of presenting hernia complications and the morbidity associated with an emergency surgical procedure (which can increase from 17 % to 57 %) are mentioned3-5. Despite what has been described, these indications are still under debate.
The surgical correction of this pathology can be done by hiatoplasty-with simple absorbable monofilament stitches-or by adding a mesh-which separates components-when the defect is significant. The type of surgical correction is controversial in the current literature, and some mention that it is up to the surgeon to define whether to use the mesh6,7. The latter is based on the fact that by placing the component-separating prosthetic mesh, the resolution of the symptoms reported in the literature is greater than 50 %8. Moreover, some comparative studies mention that the mesh can decrease the percentage of recurrence of hiatal hernia from 42 % down to 9 %1. However, placing the mesh is risky due to the prosthetic material inclusion1,9. Unfortunately, the follow-up and meta-analyzes of many of these studies are incomplete and inconclusive regarding routine mesh placement6,7. Likewise, the difference in using either biological or synthetic meshes to reduce these complications is unclear when concluding their benefits of one over the other10,11.
Regarding the complications associated with the procedure, the literature mainly reports recurrence in up to 30 % of cases6,7; complications other than recurrence and long-term are rare and are reported in less than 9 % of cases8. When hiatoplasty is performed with a component separating mesh, complications occur in a low percentage, among those: pneumothorax, injury to structures adjacent to the hiatus esophagus, bleeding, esophageal lumen stenosis, reproduction, and, to a lesser extent, migration of the prosthetic mesh to the esophageal lumen. Regarding the last complication described, there are only case series in the world (only one case series is mentioned in the reviewed literature)12.
Next, the following case presents the migration of a component separating mesh to the esophageal lumen; it shows the initial approach, diagnosis, and definitive management with which a favorable clinical outcome was obtained, which is relevant to this type of rare complication for which there are no management algorithms established in the literature.
Presentation of the case
An 83-year-old male patient with a history of symptomatic giant hiatal hernia underwent a hiatoplasty, which was performed by placing a component separating mesh in addition to a Nissen-type fundoplication. Its prognosis is adequate.
The patient went for consultation ten months later after presenting a clinical picture of progressive dysphagia for solids and liquids, worsening in the last four months before the consultation. On admission, an upper gastrointestinal endoscopy (UGIE) was performed, revealing a foreign body highly suggestive of non-passable mesh prosthetic material 36 cm from the dental arch. In Figure 1, the initial endoscopy image is shown.
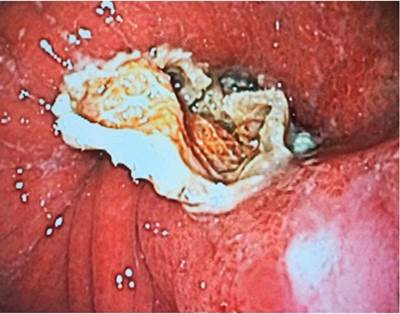
Figure 1 Image of the first UGIE showing a foreign body highly suggestive of being prosthetic material.
Given the stability of the patient, it was decided to do a serial study of the upper digestive tract, which evidenced the passage of contrast medium without reflux; a chest and abdominal tomography, which showed postoperative changes in the esophagogastric junction with esophageal dilation and delays in passing the contrast medium without any extravasation. In Figure 2, the most representative section of the tomography is shown. As no findings suggesting esophageal perforation were found in the studies performed, a new endoscopy was performed to cut and remove the mesh.
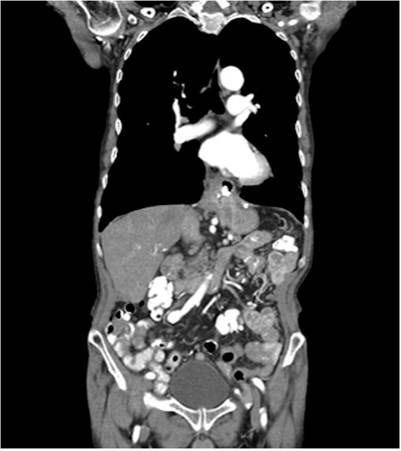
Figure 2 Coronal section image of the thoracoabdominal tomography shows postoperative changes in the esophagogastric junction with esophageal dilation without extravasation of the contrast medium.
UGIE was performed with a single-channel endoscope. It went through the esophagus, evidenced by a previously identified foreign body, suggesting a mesh. First, the material was cut, and then the mesh was extracted from the esophageal lumen with endoscopic scissors. In total, two endoscopic sessions were required; the first session was diagnostic, and the second was therapeutic, managing to resect and remove the entire segment of the included mesh. Figure 3 shows the resected mesh segment.
After this, the patient presented a good prognosis and tolerance to liquids and solids. A favorable clinical evolution was evidenced during the first months of follow-up consultations. The patient did not attend subsequent check-ups. During the initial hospitalization, the patient authorized and signed the informed consent to publish the case along with the images. Likewise, the institutional research and ethics committee approved the publication of the case.
Discussion
Hiatal hernia is a frequent pathology often diagnosed incidentally; for the most part, it is an asymptomatic hernia, and when it does present symptoms, it usually improves with medical management. In the case of the giant hiatal hernia, it is generally symptomatic and has an indication for surgical management; the type of procedure is debated between a hiatoplasty with or without the use of a mesh due to the high recurrence rate independent of surgical treatment and the complications described1. Within the results of the studies and the recommendations of the management guidelines of the Society of American Gastrointestinal and Endoscopic Surgeons, the laparoscopic route is the choice for prosthetic mesh placement2,9,13. Regarding the type of mesh, there is no specific recommendation about which type of material to use: biological over non-biological. Some reports suggest a lower risk of inclusion when using the former; however, more studies are needed to make such recommendations, and by now, it is left at the surgeon’s discretion11. The Society of American Gastrointestinal and Endoscopic Surgeons guidelines do not mention the use of biological mesh2.
Esophageal mesh inclusion is a rare complication after the performance and correction of hiatoplasty with mesh; it is reported in less than 2 % of cases11. The chief clinical manifestation of this type of complication is dysphagia, as in our patient’s case. Once the imaging and endoscopic studies are performed to visualize the intraluminal mesh component in the distal esophagus, an attempt is made to correct the complication non-invasively by endoscopy. In this regard, it is important to mention the availability of these therapeutic measures to make timely management. When endoscopic management is not possible, surgical management should consider removing the prosthetic material with a distal esophagectomy with reconstruction with esophagogastric anastomosis14. In our case, endoscopic management was performed on time, which helped this therapeutic option and ultimately led to a favorable outcome. Whenever endoscopic extraction is not possible, a surgical correction is considered. However, it can carry a high risk of morbidity and mortality; therefore, it is not the first option.
Conclusion
Esophageal mesh inclusion is a rare complication. The initial management of this complication can be done via endoscopy with good results, as in this case. If symptoms persist during the patient’s follow-up, it is proposed to place an esophageal stent and remove the rest of the prosthetic material in subsequent endoscopic attempts. These patients should be closely monitored once this pathology occurs because it may require additional management. Nowadays, no algorithm has been established to indicate and standardize the procedures to correct this complication. However, based on what was explained, it is considered that the management carried out may represent an adequate guide for treatment in a stable patient without esophageal perforation, with a good prognosis.











 texto en
texto en 




