Introduction
Intramural esophageal hematoma (IEH) is a very uncommon cause of thoracic pain, which displays submucosal dissection. It may be triggered due to esophageal pressure disorders, trauma, or spontaneously. Its clinical presentation manifests in thoracic pain, dysphagia/odynophagia, and hematemesis. Imaging tests allow for their diagnosis and the possibility to discard differentials. Prognosis is good in most cases. A clinical case of thoracic pain secondary to IEH is presented below.
Case report
A 71-year-old patient with a history of hypertension, insulin-requiring type-II diabetes mellitus, hypothyroidism, and acute myocardial infarction (AMI) with obstruction of the right coronary artery (RCA) of 20% in the previous year, checked into the emergency service of Clínica Partenón in the city of Bogotá, Colombia. The clinical picture of 40 minutes of evolution consisted of sudden retrosternal pain, in crescendo, an intensity of 10/10, oppressive, radiating towards the dorsal and mandibular region, associated with a single emetic episode, diaphoresis, and a feeling of nausea. This pain appeared after ingesting food.
Due to the high suspicion of a new coronary event, the patient was transferred to the resuscitation room. The initial vital signs were blood pressure 171/100 mmHg, heart rate (HR) 80 beats per minute (bpm), respiration rate 18 breaths per minute (BPM), temperature (T) 36 ºC, and oxygen saturation (SaO2) 93%. No supplementary oxygen is required; it is cold, diaphoretic, and all other physical examinations are normal.
An electrocardiogram (ECG) was immediately performed, which showed a sinus rhythm, inverted T wave in V1. The following was reported in the initial paraclinical tests: normal blood count, renal function, electrolytes, coagulation times, hepatic profile, and a negative cardiac biomarker. Due to the short period between the initiation of symptoms and the consultation at the emergency service, a new troponin check was performed 3 hours later, which was also negative. Therefore, an acute coronary event was discarded.
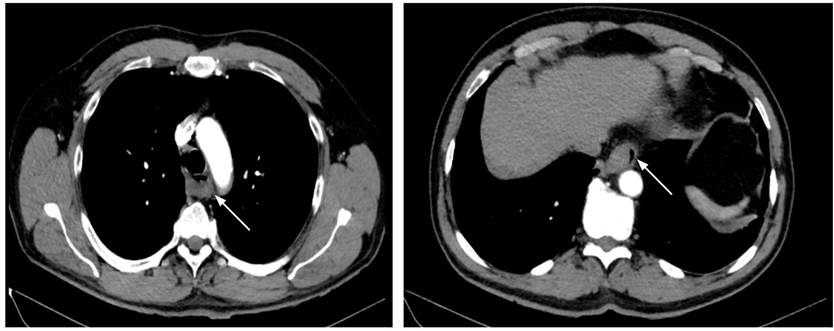
After this, a potential aortic dissection was suspected due to the location and intensity of the pain. A computed axial tomography (CAT) angiogram of the thorax was performed, resulting in negative vascular disturbances (Figure 1).
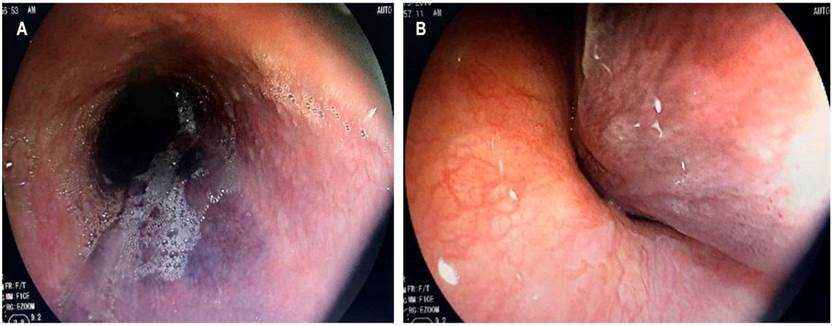
In search of differential diagnoses and due to symptomatology initiating after consuming food, an upper gastrointestinal endoscopy (UGIE) was ordered that revealed a spontaneous hematoma dissecting the esophageal wall (Figure 2A and B).
Hospitalization in the resuscitation room continued for clinical surveillance, intravenous hydration, and a proton pump inhibitor administration. The patient was assessed by the thorax surgery service, which discarded the presence of an intraluminal foreign object and mediastinitis.
Due to clinical stability, improving pain, and adequate oral tolerance, surveillance was resumed in the observation room. The patient was subsequently hospitalized, and the intravenous administration of a proton pump inhibitor continued. A control blood count was performed without evidence of leukocytosis, neutrophilia, anemia, or thrombocytopenia. Due to good evolution, the patient was discharged with warning signs, general recommendations, and an outpatient follow-up appointment by the gastroenterology service.
Discussion
IEH is a very uncommon pathology characterized by blood collections in the esophageal wall1.In terms of its epidemiology, it was found that it is more frequent in the female population (relative risk of 1.8), the mean age is 63 years, a bimodal distribution occurs with age peaks at 45 and 70 years2-6.
Typical clinical manifestations include thoracic pain, odynophagia/dysphagia, and slight hematemesis2,5,7. Thoracic pain occurs in most patients (84%)-considered the predominant symptom-characterized by its sudden origin, its retrosternal location, and often irradiated to the dorsal or interscapular region, as manifested in this patient.
The form of presentation of said pain in the adult population may be confused with an acute coronary syndrome, with the risk of worsening the hematoma and the gastrointestinal profile if anti-ischemic or fibrinolytic treatment is initiated4. In this sense, a detailed clinical history of these patients helps differentiate the thoracic pain from an aortic dissection, coronary syndromes, or esophageal perforations.
Hematemesis appears with less frequency (56%), secondary to the dissection of the hematoma by the esophageal mucosa(2). Only 33% of patients display the classic symptom triad, and 90% display one symptom thereof, as in the case discussed above, which began solely with thoracic pain. After suspecting an esophageal pathology, the Mallory-Weiss and the Boerhaave Syndrome (total rupture of the esophageal wall)6 must be considered differential factors.
Triggering factors include3:
Sudden increase in the esophageal pressure, which may appear with Valsalva’s maneuvers, nausea, or emesis;
Secondary to endoscopic procedures;
Suddenly.
Predisposition for esophageal disorders (e.g., achalasia) or coagulation disorders (antiaggregation or anticoagulation) has been observed in idiopathic cases. Furthermore, post-thrombolysis esophageal dissection cases have occurred in coronary syndromes with elevation in the ST segment4,8.
Paraclinical tests such as an electrocardiogram and thorax x-rays may be employed to discard differentials when faced with clinical suspicion. Traditionally, an esophagogram used to be employed, evidencing a filling defect or a “double duct sign” found in the distal third of the esophagus (location of most significant affectation, as it shows lower support from surrounding structures)2,6.
Currently, the computer axial tomography (CAT) and nuclear magnetic resonance (NMR) of the thorax allow for a faster and less invasive diagnosis, excluding differentials, such as aortic dissection or perforations. What is shown in the images is a well-defined thickening of the esophagus without enhancement6. Lastly, the UGIE allows clarifying the location of the hematoma in the submucosa, usually observed as a violet or blue lesion in the posterior region, which can often be confused with varicose veins or tumors2.
After diagnosis, the treatment is mainly conservative, employing intravenous fluids and dietary progression according to the patient´s evolution. Surgery is only indicated for cases with abundant bleeding, esophageal perforation, or formation of complicated abscesses with difficult draining1,3. Gastric protection agents have not been proven to offer any benefit for this pathology2. Approximately 75% of patients fully recover between 7-14 days without complications; cases with a poor prognosis are those related to terminal patients or patients with achalasia (greater rebleeding recurrence)2. These patients can be monitored through UGIE or echoendoscopy.
Conclusions
In conclusion, the IEH is an uncommon pathology that must be considered in patients with sudden thoracic pain and gastrointestinal symptoms, such as dysphagia or hematemesis. Suspicion of this pathology must be mainly based on a good clinical history, considering complications from a poor patient approach (e.g., initiation of antiaggregation or anticoagulation treatments due to suspicion of the coronary syndrome).











 text in
text in