Introduction
The “weekend effect” refers to worse outcomes, including mortality in patients who attend the hospital on weekends or holidays1-3. There are multiple reasons for this phenomenon, such as fewer health workers on weekends and less access to resources such as laboratories, radiological examinations, or specialists1. Other authors describe that patients may be sicker or present a critical condition when they go to the emergency services on the weekend3.
Upper gastrointestinal bleeding (UGIB) is the most common emergency in gastroenterology. Peptic ulcer remains the leading cause, accounting for more than half of the cases of acute gastrointestinal bleeding (AGIB)4-7 and reporting mortality rates between 10% and 14%8. Early recognition and prompt medical management decrease the risk of death associated with UGIB. Acute management of gastrointestinal bleeding (GIB) involves several steps, i.e., coordinated care ranging from resuscitation/stabilization to definitive diagnosis and medical or surgical therapy4-6.
Regarding UGIB and the “weekend effect,” the endoscopy units are closed in some institutions or have reduced business hours on weekends and holidays9. Critically ill patients with risk factors and UGIB should undergo endoscopy within the first 24 hours of admission (early endoscopy)8-10. Multiple studies, including two recent meta-analyses, show contradictory results on the “weekend effect” in the UGIB scenario on outcomes such as length of hospital stay and mortality11-14.
We decided to conduct a descriptive study comparing two groups, patients admitted during working days (weekdays) versus weekends or holidays in a tertiary referral hospital in Medellín, Colombia, to determine their demographic characteristics and characterize outcomes such as hospital stay and mortality.
Materials and methods
We conducted a descriptive observational study of a retrospective cohort of adult patients over 18 years of age who attended the emergency room between January 2016 and December 2018 due to suspected UGIB who underwent upper gastrointestinal endoscopy.
Definitions
On business days (weekdays), attendance was from Monday from 7 a.m. to Friday at 5 p.m.; weekends were set for hours between Friday after 5 p.m. and Monday at 6:59 a.m., and holidays were included according to the official Colombian calendar. Weekends and holidays were included in the same group.
The variables taken into account were sex, age, and date of care for correlation with the Colombian calendar; diagnosis by ICD-10; alcohol intake in the last 72 hours; use of cocaine, marijuana, non-steroidal anti-inflammatory drugs (NSAIDs), antiplatelet drugs, warfarin, or other anticoagulants; main symptom of admission; ASA (American Society of Anesthesiologists) classification; the presence of chronic liver disease, history of chronic kidney disease, heart disease, Glasgow-Blatchford Bleeding Score (GBS), endoscopy performed, cause of bleeding, treatment with a proton pump inhibitor, endoscopic treatment, treatment by interventional radiology or surgical treatment; laboratory results: international normalized ratio (INR), first hemoglobin, creatinine, and blood urea nitrogen (BUN); length of hospital stay in days; need to stay in a high-dependency unit, and mortality.
Data collection
We obtained the medical records in which the diagnosis was related to UGIB during emergency care. The ICD-10 codes considered were as follows:
K922: Gastrointestinal hemorrhage, unspecified
K921: Melena
K920: Hematemesis
K250: Acute gastric ulcer with hemorrhage
K594: Unspecified chronic gastric ulcer with hemorrhage
K260: Acute duodenal ulcer with hemorrhage
K262: Acute duodenal ulcer with both hemorrhage and perforation
K264: Chronic or unspecified duodenal ulcer with hemorrhage
K266: Chronic or unspecified duodenal ulcer with both hemorrhage and perforation
K270: Acute peptic ulcer, site unspecified, with hemorrhage
K272: Acute peptic ulcer, site unspecified, with both hemorrhage and perforation
K280: Acute gastrojejunal ulcer with hemorrhage
K282: Acute gastrojejunal ulcer with both hemorrhage and perforation
K286: Chronic gastrojejunal ulcer with both hemorrhage and perforation
K290: Acute gastritis with bleeding
K226: Gastro-esophageal laceration-hemorrhage syndrome
K221: Ulcer of esophagus
All researchers reviewed the related medical records, and the variables to be measured were recorded in a data collection table.
Population and sample
Patients older than 18 years who were admitted to the emergency room with a suspected or confirmed case of UGIB in the study period. The risk was established according to the GBS with a cut-off of 7 or greater for high risk. The exclusion criteria were events unrelated to GIB and patients admitted for reasons other than bleeding or who had already had bleeding in the hospital. Patients with varicose bleeding were excluded too.
Statistical analysis
Continuous variables were expressed as medians and interquartile ranges (IQR) or simple ranges, as appropriate. Categorical variables were summarized as counts and percentages. According to the day of care-weekdays or weekends-the results were compared using the χ2 test. We analyzed continuous variables using a nonparametric Mann-Whitney U test (for independent samples) after rejecting the null hypothesis of normality. All reported p-values were based on two-tailed tests, with a significance level of 0.05.
Two people processed the information independently in Microsoft Excel with double data entry of 100% of the subjects. All statistical analyses were performed in SPSS Statistics® 18.0 (IBM, Armonk, New York).
Bias control
We considered selection, information, and confounding biases; the possible sources of error in the subjects selected to participate in the study; the quality of the data obtained, and the possibility of overestimating the differences in the two groups. Regarding control strategies, participation in the study was limited to subjects whose symptoms on admission to the hospital were only associated with a high suspicion of GIB, standardizing the records search to the primary diagnosis for GIB causes according to ICD-10, except for varicose bleeding, as it is deemed a confounding variable due to an increased risk of death. Additionally, double data validation upon admission was used as a strategy to improve the information obtained.
Results
From January 2016 to December 2018, data was collected from 274 patients who attended the emergency room for UGIB and underwent upper GI endoscopy (Figure 1). 107 (39.1%) attended on weekends and holidays compared to 167 (60.9%) on weekdays. The median age was 68.5 years (IQR: 53-79), and 56.6% were men. The demographic characteristics and different results about the day of admission are presented in Table 1, together with the factors associated with bleeding, comorbidities, and clinical manifestations.
Table 1 Comparative demographic and clinical characteristics of patients according to weekend and weekdays
| Variable | Weekend group (n = 107) | Weekday group (n = 167) | P-value* |
|---|---|---|---|
| Gender (M) | 52.3 % (56) | 59.3 % (99) | 0.258 |
| Factors associated with bleeding | |||
| - Alcohol | 10.3 % (11) | 9.0 % (15) | 0.721 |
| - Cocaine | 2.8 % (3) | 0.6 % (1) | 0.138 |
| - Marijuana | 1.9 % (2) | 0.6 % (1) | 0.324 |
| - NSAIDs | 15.0 % (16) | 12.0 % (20) | 0.477 |
| - Antiplatelets | 25.2 % (27) | 29.9 % (50) | 0.398 |
| - Warfarin | 1.9 % (2) | 0.6 % (1) | 0.324 |
| Another anticoagulant | 4.7 % (5) | 3.0 % (5) | 0.470 |
| Comorbidities | |||
| - Chronic liver disease | 13.1 % (14) | 12.0 % (20) | 0.786 |
| - Chronic kidney disease | 10.3 % (11) | 12.0 % (20) | 0.664 |
| - Heart disease | 14.0 % (15) | 16.2 % (27) | 0.628 |
| Type of treatment | |||
| - Intravenous PPI | 74.8 % (80) | 80.8 % (135) | 0.233 |
| - Endoscopic interventionism | 43.9 % (47) | 48.5 % (81) | 0.458 |
| - Component therapy | 34.6 % (37) | 38.3 % (64) | 0.530 |
| - Interventional radiology | 0.9 % (1) | 1.2 % (2) | 0.837 |
| - Surgical treatment | 0.0 % (0) | 0.0 % (0) | NA |
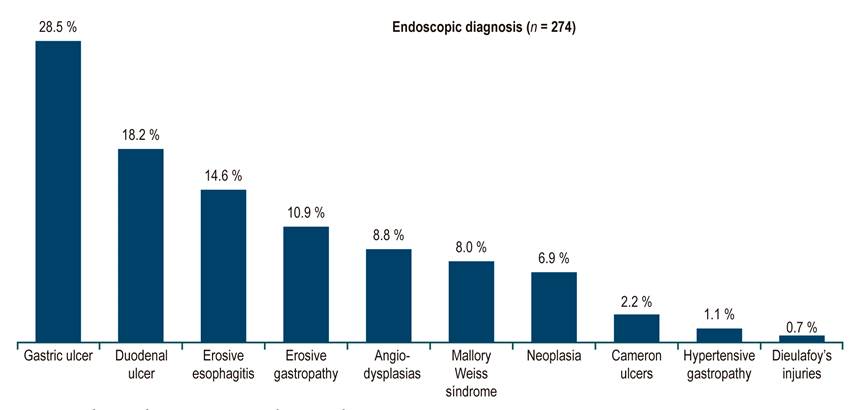
| Endoscopic diagnosis (n = 274) | |||
| - Gastric ulcer | 32.7 % (35) | 25.7 % (43) | 0.471 |
| - Duodenal ulcer | 15.9 % (17) | 19.8 % (33) | |
| - Erosive esophagitis | 15.9 % (17) | 13.8 % (23) | |
| - Erosive gastropathy | 13.1 % (14) | 9.6 % (16) | |
| - Angiodysplasias | 5.6 % (6) | 10.8 % (18) | |
| - Mallory-Weiss syndrome | 8.4 % (9) | 7.8 % (13) | |
| - Neoplasia | 3.7 % (4) | 9.0 % (15) | |
| - Cameron ulcers | 1.9 % (2) | 2.4 % (4) | |
| - Hypertensive gastropathy | 1.9 % (2) | 0.6 % (1) | |
| - Dieulafoy’s injury | 0.9 % (1) | 0.6 % (1) | |
| Time since admission to upper GI endoscopy | |||
| - Within 12 hours | 57.0 % (61) | 58.7 % (98) | |
| - 12-24 hours | 23.4 % (25) | 31.7 % (53) | |
| - More than 24 hours | 19.6 % (21) | 9.6 % (16) | 0.041 |
| Hospital place of admission | |||
| - General room | 61.7 % (66) | 61.7 % (103) | 0.142 |
| - Emergencies | 13.1 % (14) | 19.8 % (33) | |
| - Special care | 16.8 % (18) | 15.6 % (26) | |
| - Intensive care | 8.4 % (9) | 3.0 % (5) | |
*Calculated with the chi-square test (χ2). PPI: Proton pump inhibitor; NA: Not applicable.
According to comorbidities or clinical conditions on admission, endoscopies were performed in all cases with sedation and analgesia or anesthesia. Before endoscopy, each patient was classified according to their surgical risk on the ASA scale: ASA I: 13.9%, ASA II: 33.2%, ASA III: 47.4%, and ASA IV: 5.5%. The GBS was described in the medical records of 261 patients; 41.4% were considered low risk with a cut-off < 7 and 58.6% with > 7 or high risk. Table 2 shows the bivariate analysis of clinical risk according to the GBS, showing no significant differences concerning the day of admission (p = 0.293) or mortality (p = 0.447).
Table 2 Bivariate analysis of clinical risk concerning the day of admission, mortality, and endoscopy
| Variable | Risk According to GBS | P-value* | |
|---|---|---|---|
| Low risk: ≤ 7 (n = 108) | High risk: ≥ 7 (n = 153) | ||
| Days of care | |||
| Weekend | 38.8 % (40) | 61.2 % (63) | 0.293 |
| Weekday | 43 % (68) | 57 % (90) | |
| Death | |||
| Yes | 3.3 % (3) | 66.7 % (6) | 0.447 |
| No | 41.7 % (105) | 58.6 % (147) | |
| Endoscopy times | |||
| Endoscopy within 24 h | 40.3 % (91) | 59.7 % (135) | 0.228 |
| Endoscopy after 24 h | 48.6 % (17) | 51.4 % (18) | |
| Death according to the time of the endoscopy | < 24 h (n = 237) | > 24 h (n = 37) | |
| Yes | 3.4 % (8) | 2.7 % (1) | 0.827 |
| No | 96.6 % (229) | 97.3 % (36) | |
* χ 2 test.
Regarding the endoscopic diagnosis, 46.7% of the bleeding was explained by a gastroduodenal ulcer (gastric ulcer: 28.5%, duodenal ulcer: 18.2%). The different endoscopic diagnoses are shown in Figure 1 and the endoscopy times in Figure 2.
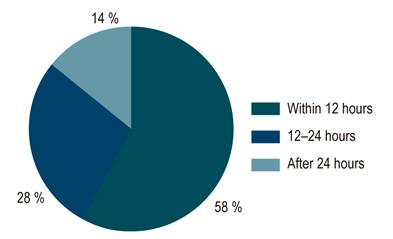
Figure 2 Endoscopy procedure time from admission into the emergency room within 12 hours (n = 159), between 12 and 24 hours (n = 78), and after 24 hours (n = 37).
After initial emergency care, 61.7% were hospitalized in general wards, 21.2% required admission to intensive care units (ICU), and the rest was discharged from the emergency department. The mean hospital stay was similar in both groups (7.38 ± 8.7 versus 7.38 ± 7.1 days, p = 0.234). Table 1 also describes the risk factors associated with bleeding, the most relevant comorbidities, and the medical and interventional treatment received by the two comparison groups.
On weekends, endoscopies were performed in 57% of the patients within 12 hours, 23.4% between 12 and 24 hours, and 19.6% after 24 hours. On weekdays, endoscopies were performed within 12 hours in 58.7% of the patients, between 12 and 24 hours in 31.7%, and after 24 hours in 9.6% (Table 3). In 86% of cases, endoscopies were performed within 24 hours, but on weekends, a higher percentage of endoscopies were performed after 24 hours. There are no differences between the 12-hour and 12-24-hour groups when discriminating the number of endoscopies. There were no significant differences when cross-checking the patients who died against endoscopies performed in less or more than 24 hours (p = 0.827). Table 3 describes the endoscopy procedure time according to the day of admission to the hospital.
Table 3 Endoscopy procedure in the group of patients admitted on weekends compared to the group admitted on weekdays
| Endoscopy procedure* | Weekend (n = 107) | Weekdays (n = 167) | P-value |
|---|---|---|---|
| Within 24 hours | 80.4 % (86) | 90.4 % (151) | 0.018 |
| After 24 hours | 19.6 % (21) | 9.6 % (16) | |
| Discrimination by subgroups | |||
| Within 12 hours | 57.0 % (61) | 58.7 % (98) | 0.041 |
| 12-24 hours | 23.4 % (25) | 31.7 % (53) | |
| After 24 hours | 19.6 % (21) | 9.6 % (16) | |
* χ 2 test.
Nine deaths (3.3%) related to digestive bleeding occurred; seven (77.7%) were admitted on weekdays. In this group, 100% were classified with a high-risk GBS; of these patients, eight (88.8%) underwent endoscopy within 24 hours.
Discussion
This study was carried out in a tertiary referral hospital. It has a gastroenterology and endoscopy service with business hours from Monday to Friday from 7 a.m. to 5 p.m. with a gastroenterologist on-call the rest of the time from Monday to Friday and weekends. In this cohort of patients, more than 60% attended the emergency room on a weekday; this percentage is because there are proportionally more weekdays. The clinical and demographic characteristics of the two groups are similar, as shown in Table 1. Our work revealed that the “weekend effect” did not occur in the variables described as the length of hospital stay or mortality in this cohort of patients. These findings may be related to the 24/7 on-call gastroenterologist in our center and the procedures carried out based on institutional protocols that do not vary during the weekend. These data contrast with those described in two extensive national reports in the United States, demonstrating higher mortality in patients who attend on weekends15,16.
Therapeutic interventions such as PPIs, component therapy, endoscopic therapy, and interventional radiology did not differ significantly in the two groups. These data are similar to those described in a multicenter study of 212 institutions with more than 6,000 patients in the United Kingdom, in which there were no significant differences in therapeutic interventions in the group of patients admitted on weekdays versus weekends13.
The difference in mortality of patients who attended a weekday versus the weekend was not statistically significant (p = 0.274). These results are comparable with multiple observational studies conducted in the United States, Europe, and Asia17-19. No observational studies of these characteristics had been reported in Latin America.
In most patients, endoscopy was performed within 24 hours, regardless of the hospital admission group, but a higher percentage of endoscopies were performed after 24 hours on weekends. This behavior did not impact mortality in this cohort of patients. The data described possibly relates to the fact that the on-call gastroenterologist is only called when the emergency physician considers the endoscopy urgent; in other words, patients who have hemodynamic stability upon initial examination do not require an endoscopy urgently or preferentially. We agree that the priority of patients who present UGIB is the initial management, including resuscitation and stabilization with intravenous fluids, correction of coagulopathy if applicable, component therapy if initial hemoglobin is below 7 g/dL, and correction of hypoxemia, especially in patients with respiratory comorbidities7,8,20. After initial stabilization, endoscopy could be considered, and then, in this scenario, early endoscopy is recommended (within 24 hours)8,20.
According to the GBS, we did not identify differences concerning endoscopy times. Two randomized controlled studies found that early (within 24 hours) or delayed (up to 48 hours) endoscopy does not produce differences concerning rebleeding or mortality in patients with low risk according to the GBS(21, 22). Regarding high-risk patients, two recent studies show that “very early” or emergent endoscopy (within six hours) does not bring additional benefits on rebleeding rates, length of hospital stay, and admission in ICUs when compared with patients who underwent endoscopy after six hours23,24. About mortality in high-risk patients undergoing endoscopy, Lau J et al found no differences in mortality at 30 days between the “urgent” and early endoscopy groups23. A large cohort study of a national database stated that the “urgent” or “very early” endoscopy may increase mortality risk in high-risk and clinically unstable patients admitted. In contrast, early endoscopy (between 6 and 24 hours) can reduce mortality relative to delayed endoscopies25.
Among the strengths that we highlight in this study, we can mention that all patients underwent endoscopy, which helped in the final UGIB diagnosis from its findings. We could elucidate no differences in hospital stay and mortality between patients admitted on weekdays and those admitted on weekends or holidays. The limitations of our work include the retrospective design and that analysis was performed in patients treated in a single tertiary referral center. Therefore, the results may not apply to all centers. There is a need for multicenter prospective studies in the region to improve external validity and, thus, make recommendations.
In conclusion, in the cohort of patients admitted to our hospital due to UGIB, the “weekend effect” did not occur. Hospital stay times and mortality were similar in patients who attended on weekdays versus those who attended on weekends.
UGIE was performed in most of the patients early. Statistically, a significant difference was found in endoscopies performed after 24 hours on weekends without adversely impacting any of the variables studied.











 texto en
texto en