Case report
A 42 years-old female patient, from the Colombian Amazon, was admitted to the emergency department for a clinical picture of 4 days of evolution, characterized by moderate to severe burning abdominal pain, located in the epigastric irradiated to the right band hypochondrium, associated with fever and multiple biliary emetic episodes. On physical examination, she was dehydrated, feverish, with jaundice tinge and pain on abdominal palpation in the epigastrium, without signs of an acute abdomen.
It was decided to place a nasogastric tube given multiple emetic episodes, with subsequent clinical improvement. Paraclinics reported amylase at 600 U/L (normal: 30-100 U/L), leukocytosis 21,000 (normal: 5,000-10,000 cel/U), 92% neutrophilia (Normal: 50%-60%), transaminases, electrolytes, lipids, phosphatase and bilirubin within normal limits. During her hospital stay, the patient expelled an ascaris through the nasogastric tube (Figure 1).
A biliary ultrasound was performed that ruled out cholelithiasis and choledocholithiasis, although there was evidence of pancreatic inflammation. A contrast abdominal computed axial tomography (CAT) scan showed necrosis in the body of the pancreas without identifying defined collections, compatible with acute necrotizing pancreatitis (Balthazar C) (Figure 2), and a cholangiopancreatography showed that the patient had interstitial edematous acute pancreatitis with a peripancreatic collection of 32 x 23 mm (Figure 3), which was classified as moderate, based on the clinical severity index, with AN APACHE II (Acute Physiology and Chronic Health Evaluation II) of 6 points, and a 1-point assessment in the modified Marshall classification.
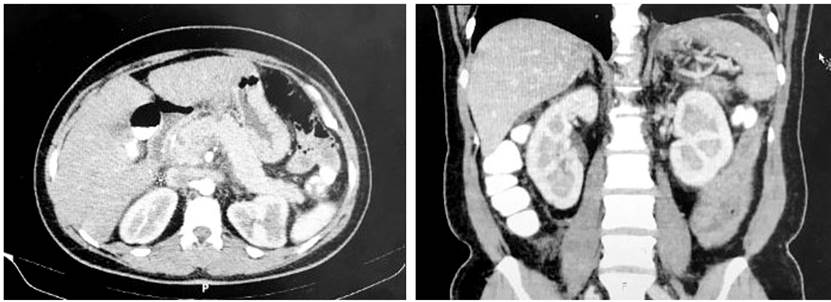
Figure 2 CAT scan with necrosis in the body of the pancreas without identifying defined collections.

Figure 3 Cholangiopancreatography with interstitial edematous acute pancreatitis with a 32 x 23 mm peripancreatic collection.
Consequently, management was started with fluid resuscitation, oral restriction, antiemetic, analgesia, broad-spectrum antibiotics with ampicillin/sulbactam due to the collection evidenced in the cholangiopancreatography and albendazole 400 mg in a single dose because of the history of expulsion of ascaris through the nasogastric tube.
On the third day after hospital admission, the patient showed clinical improvement with a decrease in leukocytosis and abdominal pain. On the seventh day, a new imaging control was performed without evidence of collections with mild pancreatic edema. The patient was discharged on the tenth day of hospital stay due to satisfactory evolution, with a general good condition, and with adequate controls at the external consultation one month later.
Discussion
Etiologies involved in acute pancreatitis are identified in 75%-85% of cases, and biliary lithiasis and alcohol consumption are the two most common causes in adults1. Only about 10% of cases of acute pancreatitis are idiopathic, including parasitic infections2.
Ascariasis is the most common helminth infection in the world, caused by Ascaris lumbricoides, and has a global prevalence of 25%. It is a ubiquitous parasite in the Indian subcontinent, China, the African continent and Latin America. It is estimated to occur in approximately 16% of rural citizens of the European Union3 and in approximately 4 million people in the United States4. Its prevalence is increasing, especially in industrialized countries, due to immigration and the increasing number of refugees5. According to World Health Organization (WHO) figures, soil-borne helminthiasis affects more than 2,000 million people worldwide, of whom A . lumbricoides infest 1,221 million, causing alterations in the ability to work and learn, as well as delays in the physical growth of children6.
The present case came from the Colombian Amazon, an endemic area for Ascaris. The prevalence of ascariasis is associated with hot and humid climates; in these tropical and subtropical regions, A. lumbricoides infections are part of the daily lives of low-income populations4,7. Risk factors associated with transmission are poor hygiene, contaminated environment, poor educational level, open sewage, inadequate water supply, poor nutritional status, and use of human biosolids for fertilizers and irrigation5.
Ascariasis is more prevalent in children; however, evidence shows that acute pancreatitis secondary to hepatobiliary and pancreatic ascariasis (HPA) is an adult disease, predominantly in women4,8. The clinical picture presents severe abdominal pain, biliary colic, jaundice, vomiting that may or may not be accompanied by live adult worms, and fever9,10. These symptoms occur due to the invasion of the parasite into the bile ducts; rarely, the parasite invades the pancreatic duct. Patients with pancreatic ascariasis frequently present necrotizing pancreatitis4,8.
The diagnosis of acute pancreatitis requires at least two of three criteria: Abdominal pain consistent with the disease, biochemical evidence of pancreatitis, and imaging findings characteristic of the condition11. The diagnosis of acute pancreatitis due to ascariasis should be made by clinical imaging, as laboratory tests do not assist in diagnosing HPA. Eosinophilia is usually present during lung migration, and stool microscopy reveals only eggs or adult worms. Blood counts, liver function tests, renal function tests, and serum amylase help to assess the pattern and severity of hepatobiliary and pancreatic disease4,12.
In this case, the diagnosis was made by exclusion. An abdominal ultrasound was requested that ruled out biliary etiology; the contrasted abdominal CAT was the second choice, which showed the presence of necrotizing pancreatitis and a possible collection that was clarified by cholangiopancreatography.
Hepatobiliary ultrasonography is a useful method for initial diagnosis; however, it has a sensitivity of 25%-86% to identify HPA and decreases in pancreatitis 9. The tested abdominal CAT scan is the gold imaging standard for determining the severity of pancreatitis and for identifying pancreatic and extrapancreatic complications, as well as collections. Magnetic resonance imaging (MRI) is the alternative study in case of contraindication or uncertainty to diagnosis1.
Cholangiopancreatography has a sensitivity of 97%-98% and a specificity of 84.4% for choledocholithiasis11; as well, biliopancreatic endoscopic ultrasonography is a good option in the presence of suspected biliary obstruction of unclarified etiology9. Cholangiopancreatography or endoscopic ultrasonography should be considered as control studies to detect occult choledocholithiasis when the etiology is uncertain and to avoid invasive studies in suspected patients4.
ERCP is the preferred method for identifying and eliminating the parasite. Early intervention with ERCP followed by anthelmintic medication reduces morbidity, mortality, and recurrence . Therefore, it is considered the first line in the management of HPA1,13. However, it has limitations as a diagnostic tool since it is invasive, not available to primary care physicians, and is at risk for postoperative complications (pancreatitis, bleeding, bowel perforation). All patients with severe pancreatitis should be evaluated by CAT, magnetic resonance cholangiopancreatography (MRCP), or endoscopic ultrasound to detect hidden stones in the common bile duct11.
Liquid collections and necrosis in pancreatic tissue are sterile during the early stages of acute pancreatitis; however, up to 40% of patients are usually over-infected in the course of the disease. Local or systemic infectious complications characterize the most severe forms of late-stage disease and can even lead to death from uncontrollable infections. Infected necrotizing pancreatitis (INP) is a determinant of increased mortality; in patients with acute pancreatitis, more than 80% of deaths are attributed to septic complications as a consequence of bacterial infections in INP14.
Diagnosis of INP can be difficult; fever and elevation of inflammatory markers are indicative of infection; these, together with risk factors for developing INP, are useful in clinical decision-making about disease management15. The current recommended treatment in INP and pancreatic sepsis is antibiotic administration16.
Imipenem, fluoroquinolones, and metronidazole are the drugs of choice because they reach high inhibitory concentrations in pancreatic tissue; acylureidopenicillins have intermediate penetrance17. In this case, due to the clinical condition of the patient and the elevation of the inflammatory markers, antibiotic therapy with ampicillin/sulbactam was indicated, which showed good results.
A. lumbricoides is extremely sensitive to antihelmintic treatment with benzimidazoles; mebendazole has efficacy of 84%-99%12,18, while albendazole is 93.2%-97.3%, and is administered in a single 400 mg 19. This is the most widely used antihelmintic drug for its high rate of cure and reduction of eggs17.
The mechanism of action of albendazole is mediated by selective binding to nematode β-tubulins, which inhibits microtubule polymerization and cell division, and thus leads to loss of chromosomal segregation and kinetochore alteration during meiosis, resulting in aneuploidy and infertility20. Resistance to treatment has been reported due to a genetic mutation in the β-tubulin protein to which albendazole binds. According to evidence from current literature, this can be solved by a synergy of nitazoxanide-combined therapies5,21.
Vaccines against ascariasis that have progressed to the clinical phase are currently unavailable5. However, studies of selective inhibitors that protect A. lumbricoides from host enzymes and the immune system have been able to identify a metallocarboxypeptidase (MCP) inhibitory protein, called ACI, which inhibits the action of enzymes in the intestine that participate indigestion. Hence, it plays a fundamental role in the survival of the parasite during infection, making it a target for the development of the vaccine22.
Conclusions
Ascariasis is the most common parasite involved in pancreatitis with a high mortality from necrotizing pancreatitis. Its diagnosis is based on excluding its main causes by an adequate physical examination and imaging using abdominal ultrasound as the first choice, followed by CAT and cholangiopancreatography. Antiparasitic treatment with albendazole is the most effective in the current literature; however, it is important to emphasize that the control of ascariasis is possible by improving sanitation combined with health education and personal hygiene.











 text in
text in 




