Introduction
Inflammatory bowel disease (IBD) includes ulcerative colitis and Crohn’s disease. In Colombia, IBD has an estimated prevalence of 87 cases per 100,000 inhabitants: For Crohn’s disease, it is 17 per 100,000 inhabitants, and for ulcerative colitis, it is 113 per 100,000 inhabitants1. Although the exact etiology of IBD remains studied, most agree that there is tissue damage caused by an excessive immune response against luminal bacterial flora in predisposed people as a result of the action of different environmental factors2.
These diseases are characterized by periods of remission and outbreaks. These outbreaks are triggered by an immune system that presents a chronic inadequate response and, therefore, drug treatment includes a diverse number of immunosuppressive drugs3. Currently, the new severe acute respiratory syndrome due to the severe acute respiratory syndrome by coronavirus type 2 (SARS-CoV-2) is of great concern in patients with IBD given their immunosuppressive status. Indeed, since the identification of the first cases of the 2019 coronavirus disease (COVID-19) began in Wuhan, China, at the end of 2019, this infection has spread precipitously to countries where IBD is more prevalent. It is of greater concern when there is a worse clinical outcome in patients with comorbidities and coinfection of SARS-CoV-24. In patients with chronic diseases such as IBD, the appearance of COVID-19 has generated uncertainty in the approach and treatment since the effect of this infection with the decompensation of the underlying pathology, severity of symptoms, and immunosuppressive management is not clear5. A case of a patient with Crohn’s disease and SARS-CoV-2 coinfection is described below.
Clinical case
A 28-year-old young man with a 3-year history of non-fistulizing Crohn’s disease with involvement of the distal ileum of chronic ileitis and in the cecum of erosive chronic colitis and pseudopolyps, with Montreal A2L3B2 classification. The patient attends a tertiary care clinic with generalized abdominal pain, fever, distended abdomen , nausea, liquid stools without blood, and episodes of emesis of food content. He has a history of resectioning neuroblastoma in the adrenal gland in 1994 and laparotomy for complicated appendicitis in 2019. He had suspended the pharmacological management of mesalazine 2 g oral.
When admitted, his admission weight was 57 kg, his vital signs were significant, with blood pressure (BP) of 119/82 mm Hg, heart rate (HR) of 136 beats per minute (bpm), oxygen saturation (SatO2) Of 98% in ambient air and a temperature of 37 °C. The C-reactive protein (CRP) was 136 mg/L (normal: < 8 mg/L). Blood, stool and urine cultures were negative. Total abdominal computed tomography (CAT) on admission reported a focal continuity solution of the terminal ileum wall 3 cm from the ileocecal valve, compatible with perforation, which communicates with a collection related to the face of the right psoas muscle, at the level of its middle third (approximate volume: 12 cm3). There was little free fluid in this iliac fossa, a moderate inflammatory process of the local intestinal walls and fatty tissue. The adynamic ileus was secondary. He was evaluated by the specialties of general surgery and coloproctology. Surgical management was considered after initiating antibiotic treatment with ampicillin/sulbactam 3g intravenous and nutritional support. He showed improvement in the clinical picture.
Later, 7 days after admission, he again presented an episode of abdominal pain, fever, and mild blood-free liquid bowel movements with a frequency of 2 to 3 times a day. A new computed tomography (CAT) scan of the whole abdomen was taken, which reported a partial resolution of the signs of an inflammatory process in the ileocecal valve region. There was no evidence of liquid collections in this exam. The antibiotic staging was decided with piperacillin/tazobactam 4.5 g intravenously.
The patient showed clinical improvement during a week, but again presented thermal spikes quantified at 41.5 °C. It was decided to reculture with negative results, negative infectious profile (human immunodeficiency virus [HIV], tuberculosis, hepatitis B [HBV] and C [HCV]) And due to persistent fever, it was decided to take the reverse-transcription polymerase chain reaction (RT-PCR) test for SARS-CoV-2 by positive nasopharyngeal swab. There were no respiratory symptoms at any time, but chest CAT was taken, which was reported within normal parameters.
The specialty of infectology evaluated him, and considered to recommend avoiding major surgery because of the high likelihood of complications due to the active IBD and SARS-CoV-2 coinfection. In that order of ideas, the coloproctology specialty decided to defer surgical management on the recommendation of the infectiology specialty and, given that the laparoscopic surgery for the pneumoperitoneum that is required would become an aerosol-generating medical procedure, with a high probability of nosocomial infection to health personnel, the procedure was deferred until a negative result of RT-PCR for SARS-CoV-2.
The patient continues to be followed up by internal medicine and gastroenterology specialties. According to the Crohn›s disease activity index (CDAI), it is classified as severe activity (466 points) according to the clinical manifestations of the patient›s admission (weight: 57 kg, ideal weight: 74 kg, sex: male, total number of stools in the previous 7 days: 21, abdominal pain: severe, general condition: terrible, abdominal mass: doubtful, hematocrit: 37%, fever: yes). It was decided to give an initial dose of ivermectin, 1 drop per kg weight, with a second dose at 10 days, and metronidazole 500 mg intravenously was added to the antibiotic administration. Steroids were started with methylprednisolone 45 mg intravenously/day for 5 days (prednisolone equivalent to 1 mg/kg/day). An entero-resonance was performed that reported stenosis of the most distal aspect of the last loop of the ileum due to focal concentric thickening of its walls. There are no signs of an acute inflammatory process, fistula, or liquid collections.
The patient showed improvement in his clinical picture with a CDAI of 207 points and was decided to discharge on day 25 of hospitalization with pharmacological management of prednisolone 50 mg oral with progressive reduction, azathioprine (2 mg/kg/day) 50 mg orally every 12 hours and extended-release granules of mesalazine 2g every 12 hours due to ileal and right colon involvement. The RT-PCR test for SARS-CoV-2 was repeated by nasopharyngeal swab twice and was eventually negative after 42 days of initial presentation. A fecal calprotectin was taken with a result of 414 µg/g (normal: < 50 µg/g).
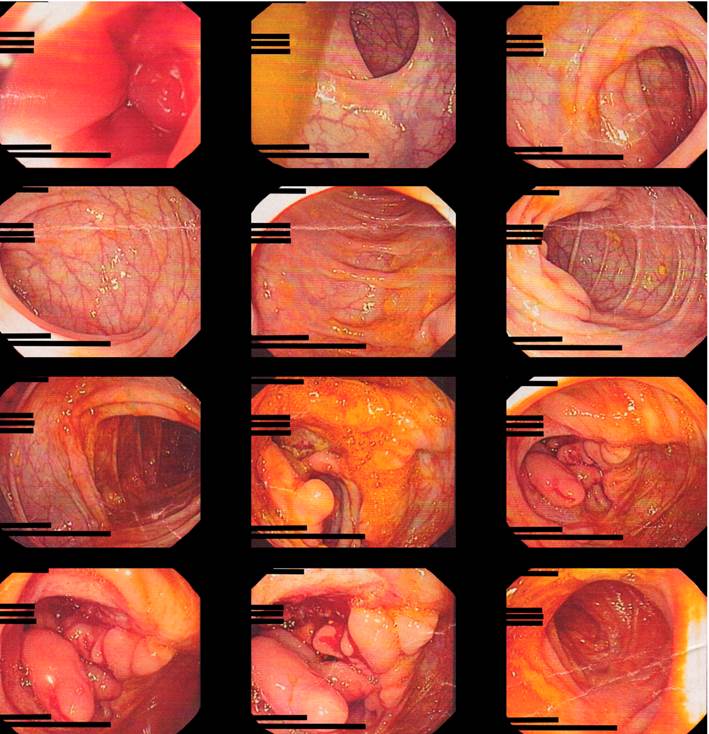
The colonoscopy biopsy report resulted in acute and chronic ileitis with erosion, acute, and severe chronic ulcerative colitis. In the endoscopy biopsy report, superficial chronic gastritis and Helicobacter pylori were observed in small amounts (Figure 1). He was followed up in the outpatient control with gastroenterology and infectology specialties. As a health worker, the patient had the complete vaccination schedule, so the specialties determined that the most recommended biological management according to the clinical and social situation of the patient was with vedolizumab 300 mg with an induction and maintenance scheme, and with nutritional support due to moderate protein-calorie malnutrition. The infectology service recommended, due to immunosuppression and real risk of reinfection, not to work in an area where patients with COVID-19 are managed. The patient reported improvement in his gastrointestinal symptoms, weight gain and improvement in quality of life, controls with negative CRP and erythrocyte sedimentation volume (ESR). He presented a CDAI at the beginning of the management with a fall of more than 100 points and is currently <150 points, which indicates clinical remission.
Discussion
This case is interesting for different reasons; firstly, because of the specific manifestations of COVID-19 in patients with IBD. The main clinical picture of this infection in this group of patients is similar to that of the general population, with fever and cough in most of them (77%-90% and 66%, respectively)6,7. In our patient, there were never respiratory symptoms or lung involvement, but in this viral infection, it can be found that in up to 61% of cases gastrointestinal symptoms such as anorexia (35%), diarrhea (34%) and nausea (26%) are present8. This observation recommends that in IBD patients who develop new digestive symptoms during the SARS-CoV-2 pandemic, especially if it is diarrhea, this infection should be considered within the differential diagnosis9.
Second, it should be determined whether there is an increased risk of infection in patients with IBD. Different studies have been conducted to find a relationship between IBD and COVID-19; SARS-CoV-2 has been found to use the angiotensin-converting enzyme II (ACE-II) as an input receptor and the protease TMPRSS2 to enter the cell10-12. An increase in the expression of this receptor in the inflamed intestine of patients with IBD has also been reported13. These findings show an increased risk of acquiring and facilitating the entry of SARS-CoV-2 into the body, but one should still wait until direct clinical evidence is found14.
Third, the patient tested positive for a prolonged SARS-CoV-2 infection. Studies show that the average positivity duration for the virus is approximately 12 days15. In the case of our patient, it should be studied whether the use of immunomodulators and immunosuppressants could lead to a prolonged SARS-CoV-2 infection.
Finally, the approach to medical and pharmacological management of patients with IBD and COVID-19 is based primarily on prevention, biosafety measures and continuous monitoring. This is due to recommendations made by international organizations such as the European Crohn’s and Colitis Organization (ECCO) and the International Organization For the study of Inflammatory Bowel Disease (IOIBD)14-16.
It is also important to determine when to initiate immunosuppressive or biological management following SARS-CoV-2 infection. The patient presents with severe IBD activity with a mild SARS-VOC 2 coinfection with no lung involvement, allowing uncomplicated immunomodulatory and steroid management initiation. However, different studies report that in cases of severe infection, immunosuppressive treatment should be temporarily or definitively discontinued16. It was decided not to initiate biological management in the patient until a negative RT-PCR result for SARS-CoV-2 was obtained. Studies recommend waiting at least two weeks to start administering biological drugs17.
There is currently a database called Surveillance Epidemiology of Coronavirus Under Research Exclusion-Inflammatory Bowel disease (SECURE IBD), which tracks COVID-19 in patients with IBD. As of January 8, 2021, 4,280 cases had been reported in 64 countries of the world, led by the United States with 38% of cases, and in Colombia, 3 cases had been reported. The mortality observed in patients treated with anti-integrins is 1%, compared with 5-aminosalicylic (5-ASA), which is 3%, budesonide: 3%, steroids: 7%, azathioprine: 2%, methotrexate: 3%, monotherapy with tumor necrosis factor antagonist alpha (anti-TNF-α): 0%, combined therapy with immunosuppressants: 1%, anti-interleukin (IL)-12/23: 1% and JAK inhibitor: 2 %. According to the severity of IBD, patients with moderate/severe activity have a mortality rate of 2%18. This registry allows this case to be approached and compared with the IBD and SARS-CoV-2 coinfection population.
Future studies should investigate the duration of SARS-CoV-2 positivity in patients with IBD and its transmission capacity. Also, the impact of immunomodulation on the outcome of infection and, finally, look for the relationship if SARS-CoV-2 infection is a cause of increased IBD activity.











 text in
text in