Introduction and objectives
Gastrointestinal diverticula have their location mainly at the colonic level, and it has been observed that their second most frequent location is the duodenum, the latter at the level of the second and third duodenal portions1. They are called periampullary when they are within 2 to 3 cm of the Vater’s ampulla 2-3.
Periampullary duodenal diverticula (PDD) have an incidence between 10% and 15% in patients who have endoscopic retrograde cholangiopancreatography (ERCP). Its incidence increases with age, reaching up to 25% to 30% in patients between 50 and 60 years old1,4,5. In most cases, they are asymptomatic4 and are incidentally diagnosed2.
PDDs have been classified into three types according to the relationship between the major duodenal ampulla and the anatomical variant1, and are associated with an increase in failures and complications when cannulation is performed4,6,7; however, other authors consider that this procedure has the same risks with or without this defect8. As a result, we decided to review and describe our experience with this anatomical anomaly and demonstrate how this affects the procedure’s success rate.
Materials and methods
Population
A cross-sectional observational study was conducted, with retrospective data collection from electronic medical records, of patients diagnosed with PDD. The study population was patients at the Centro Intergastro, El Salvador, between 2013 and 2017.
Patients older than 18 years old with an incidental institutional finding of PDD and patients referred with PDD diagnosis for endoscopic intervention were included. The latter was performed by 2 endoscopists, who perform an average of 750 to 900 ERCPs per year. For the procedure, all patients were given topical oral-pharyngeal lidocaine 10% aerosol, sedation with midazolam (1-3 mg), or meperidine (30-50 mg) at the discretion of the endoscopist, and single-dose antispasmodic with hyoscine butylbromide (20 mg). According to the institution’s protocols, the procedure was performed with strict monitoring of the patient, which was supervised by the physician certified in sedation.
PDDs are classified according to Boix (Table 1)1. The technical failure was defined as problems related to cannulation and was classified according to Boix1 and ESGE (European Society of Gastrointestinal Endoscopy) guidelines (Table 2). Therapeutic failure was considered in patients who persisted with obstructive biliary syndrome during follow-up. Complications related to the procedure included post-ERCP bleeding and pancreatitis, which was defined as post-procedure abdominal pain with a blood amylase greater than 3 times the reference limit9.
The ethics committee of our institution approved this study. The protocol was performed according to the World Medical Association Declaration of Helsinki-Ethical Principles for Medical Research Involving Human Subjects guidelines, adopted by the 18 th WMA General Assembly, Helsinki, Finland, June 1964, and reviewed in Tokyo 2004”10.
Table 1 Classification of periampullary duodenal diverticula according to Boix1
| Type | Description | Subtypes |
|---|---|---|
| I | Location of the papilla within the diverticulum | a. Towards the upper side b. To the left side c. Towards the lower side d. To the right side |
| II | Location of the papilla within the edge of the diverticulum | a. Located on the left apical margin b. Located on the right apical margin c. Located in the left or right center margin d. Papilla located between the margin of two diverticula |
| III | Diverticulum located 2 to 3 cm from the papilla |
Table 2 Classification according to modified cannulation difficulty as explained by Boix and ESGE guidelines1,18
| Grade | Description |
|---|---|
| 1 | Easy deep cannulation with routine methods |
| 2 | Special guide wire or sphincterotome requirement to achieve cannulation |
| 3 | Difficult cannulation requires special techniques and skills such as needle knife sphincterotomy Other current techniques based on ESGE guidelines: Hemoclips, balloon dilation of the diverticulum, placement of pancreatic stent, use of video gastroscope with lid |
| 4 | Impossibility of deep cannulation |
Data collection
A retrospective review of medical records of patients undergoing ERCP with PDD findings was performed, including variables such as age, sex, pre-operative indication given by the reference center, endoscopic diagnosis, surgical variables, and postoperative complications.
The inferential statistical analysis of comparison was performed using the chi-square test (χ2), considering a p value <0.05 as statistically significant for a difference.
Results
Over 5 years, 214 patients had some type of PDD with an incidence of PDD of 4.7% in our population. In the sex distribution, there were more women (68.2%) than men (31.8%), with a ratio of 2.15:1; and a median age of 73 years (standard deviation [SD] + 16.08).
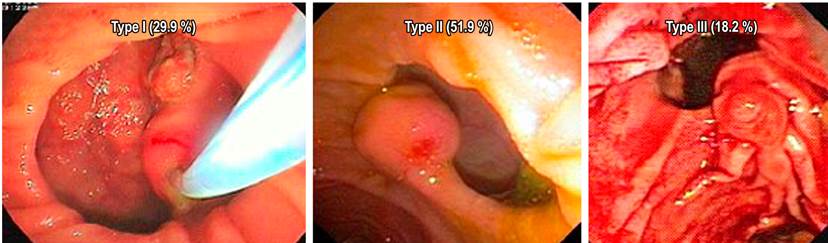
The most frequent indication of ERCP was choledocholithiasis in 114 patients (53.3%), and the distribution of subjects by type of PDD was: Type 1: 29.9%, type 2: 51.9% and type 3: 18.2 % (Figure 1, Table 1). Complications included a relationship between the technical success rate (cannulation) and PDD type. Considering the type 1 discriminated in degree of difficulty as grade 4 (11.6%) and grade 3 (21.74%), with a non-significant p(0.23) (Table 3).
Table 3 Types of difficulty in cannulation
| Boix type | Difficulty | Total | |||
|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | ||
| 1 | 25 | 16 | 15 | 8 | 64 |
| 2 | 62 | 30 | 17 | 2 | 111 |
| 3 | 31 | 4 | 4 | 0 | 39 |
| Total | 118 | 50 | 36 | 10 | 214 |
The therapeutic failure rate for each type of PDD showed a higher failure rate for type 1 (28.12%), compared with type 2 (9%) and type 3 (0%), and it is statistically not significant (p = 0.35). Post-procedure bleeding occurred in a total of 7 patients (3.29%), and there was no statistical difference in the rate of complications between PDD types (p = 0.395) (Table 4). This study did not identify other associated complications such as post-ERCP pancreatitis, perforation, or cholangitis.
Discussion
The most frequent location of PDDs is at the periampullary level at about 75%4. According to Boix, the latter are endoscopically classified into three types according to their location in relation to the Vater’s ampulla. Types 1 and 2 are subclassified into a, b, c, and d (Table 1)1. The most common typification according to the literature is 3 (55.8%)6,11, followed by type 2 (25.6 %), and type 1 (18.6%)6; however, in our study, type 2 (51.9%) and 1 (29.9%) were more frequent than 3 (18.25%).
PDDs are more prevalent in women than in men6,12,13, as demonstrated in our study with a ratio of 2.15:1. The majority of the population with this alteration does not report associated symptoms, and the diagnosis is obtained incidentally by less frequent radiographic images or by endoscopic means during ERCP6,7,14. However, they may present nonspecific or specific gastrointestinal symptoms in around 5%, in which abdominal pain is found at the umbilical, epigastric, or right hypochondrium level, emetic symptoms, and belching but the presence of these does not confirm the diagnosis15.
This anatomical variant is associated with stones of the common bile duct, which is attributed and is based on several theories, which include a malfunction of the sphincter of Oddi, the compression that the diverticulum can generate in the common bile duct in its distal portion, or increased pressure in the tract caused by papillary spasms6,16,17. In this study, an association between PDDDDP and biliary lithiasis of 53.3% was found following the evidence in the literature, but it has also been related to perforations, major papilla bleeding, choledocholithiasis, pancreatitis, and, in isolated cases, tumors6-8,11.
The literature states that cannulation in patients with PDD has greater complications and therapeutic failures than ERCP without this anatomical variation. The difficulties encountered are the increase of time, attempts, experience, and skill of the endoscopist4,7. According to ESGE guidelines, it is considered difficult cannulation when you have 5 contacts with the major ampulla and this is attempted for more than 5 minutes after recognizing the structure18. The technical failure rate is around 61% to 95.4%6-7 when this anatomical variant exists, indicating a decrease in relation to those without this alteration6. The main cause of technical failure is the non-identification of the Vater’s ampulla 6-7, and this is seen mainly in type 1 PDD6, as seen in our study in 8.4% of the cases.
In a retrospective study conducted by Sfarti et al. from 2016 to 2017 with 98 patients, they were divided into groups A (43 PDD) and B (55 non-PDD), all undergoing ERCP. Their study group showed that women tend to be at higher risk with an odds ratio (OR) of 1.099, as documented in our study. According to the classification, type 1 had 18.6%, type 2 had 25.6%, and type 3 was the most frequent with 55.8%. Easy cannulation was lower in group A (628%) compared with group B (83.6%); additionally, this technique was more difficult in group A (25.6%) than in group B (16.4%). Therapeutic failures were greater in group A (11.6%) than group B (0%). There was no significant difference between one group or another in the post-procedure complications, similar to what was evident in our study6.
The main limitation of our study is that it is an observational study without randomization, based on a retrospective evaluation of a database of our institution.
Conclusion
PDD presence during ERCP is associated with increased technical failure (cannulation failure) and therapeutic failure (persistence of biliary obstruction). In addition, these failures increase substantially when it comes to a Boix-classified type 1 intradiverticular papilla, so we suggest that experienced endoscopists perform biliary endoscopic procedures under these conditions to minimize the likelihood of technical failure and therapeutic and associated complications.











 texto en
texto en