Introduction
Adenomas of the major duodenal papilla are premalignant lesions that may occur sporadically or in the context of genetic syndromes such as familial adenomatous polyposis. The endoscopic technique used to resect these lesions has been widely described1,2. In Colombia, several case reports and papers describing the local experience regarding endoscopic resection of adenomas of the major duodenal papilla have been published3,4. Adenomas of the minor duodenal papilla are much less frequent than major duodenal papilla and have been described only in case reports5-8. So far no cases of endoscopic papillectomy of the minor papilla have been described in Colombia. This paper presents two cases of patients with adenomas of the minor duodenal papilla who were treated using endoscopic papilectomy at the Clínica Universitaria Colombia, in Bogotá.
Description of the cases
Case 1
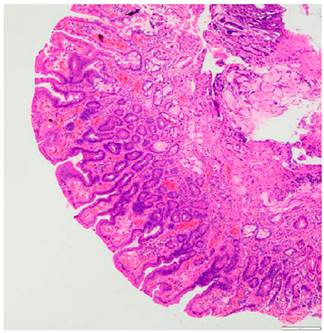
A 66-year-old woman underwent an esophagogastroduodenoscopy due to dyspeptic symptoms in which a 10-millimeter sessile polypoid lesion located in the second part of the duodenum was detected; in addition, using the side-viewing duodenoscope it was confirmed that the lesion was located in the minor duodenal papilla (Figure 1). A tubular adenoma with low-grade dysplasia was described in the biopsy report. Besides, a lesion, with involvement up to the muscularis mucosa, susceptible to endoscopic resection was found on endoscopic ultrasound. Normal findings were reported on total colonoscopy and magnetic resonance cholangiopancreatography; there was no evidence of pancreas divisum.
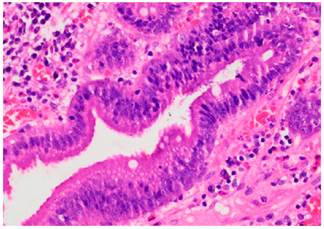
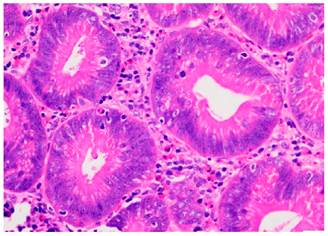
The patient underwent an ampulectomy of the minor duodenal papilla. Regarding the technique used during the procedure, the patient was under general anesthesia and was placed in a modified prone position. The second part of the duodenum was accessed using the duodenoscope and the major duodenal papilla was examined, where no abnormalities were found. An en-face view of the minor duodenal papilla was possible in the semilong axis, showing 10 millimeters of greater size adenomatous-like changes. The lesion was raised with normal saline solution + methylene blue (dilution ratio: 1:100 000) and an ampulectomy was performed using a diathermic loop. The specimen was retrieved with an endoscopic mesh basket and sent to the pathology service for analysis. There were no immediate complications. The following findings were described in the pathology report: a completely resected intestinal type tubular adenoma with low grade dysplasia (Figures 2 and 3).
The patient was hospitalized on the day the procedure was carried out for observation purposes, and since her condition improved satisfactorily she was discharged the following day. There was no evidence of lesion recurrence on follow-up duodenoscopy at 6 months, 12 months and 24 months.
Case 2
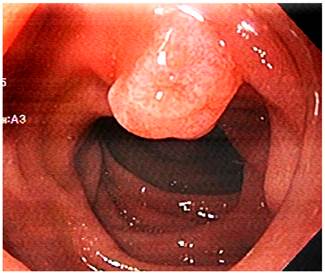
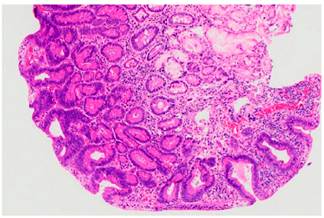
A 73-year-old male with a history of endoscopic submucosal dissection of a lesion in the rectum (high-grade dysplasia tubulovillous adenoma) underwent an esophagogastroduodenoscopy due to dyspepsia symptoms and in which an approximately 10 millimeters adenomatous-like lesion was detected; appearance was found; when assessed with the duedonoscope the lesion was compatible with an approximately 10 millimeters adenoma of the minor duodenal papilla (Figure 4); there were no abnormalities in the major duodenal papilla. A tubular adenoma with low-grade dysplasia was reported in the biopsy report. No abnormal findings or evidence of pancreas divisum were reported on the magnetic resonance cholangiopancreatography. The patient underwent a papillectomy of the minor duodenal papilla; the technique used during the procedure similar to that described in case No. 1. There were no immediate complications. The following findings were described in the pathology report: a completely resected intestinal type tubular adenoma with low grade dysplasia (Figures 5 and 6).
The patient was hospitalized on the day the procedure was carried out for observation purposes, and since his condition improved satisfactorily he was discharged the following day. There was no evidence of lesion recurrence on follow-up duodenoscopy at 4 months, 10 months and 20 months.
Discussion
Lesions affecting the minor duodenal papilla are rarely described; these lesions can be benign adenomas5-8, gangliocytic paragangliomas9,10 or carcinomas11,12. Furthermore, they can be single lesions or they can be associated with adenomas of the major duodenal papilla8 and familial adenomatous polyposis8.
Before performing a papilectomy it is necessary to define the anatomy of the pancreatic duct by means of endoscopic ultrasound or magnetic resonance cholangiopancreatography and rule out the adenoma involvement of the pancreatic duct. In case of concomitant pancreas divisum coexists, a pancreatic stent must be placed in the duct of Santorini after papillectomy in order to reduce the possibility of post-endoscopic retrograde cholangiopancreatography pancreatitis5-8. Pancreas divisum was not present in none of the two patients presented here, so no pancreatic stents were placed in the duct of Santorini and neither of them developed post-resection pancreatitis. In cases in which a pancreatic stent is placed, it is recommended to remove it after 2 weeks to reduce the risk of lesions in the pancreatic duct2.
Controversy has been raised regarding the use of submucosal infiltration to raise the lesion prior to resection. Currently, most authors do not use this measure in major duodenal papilla resection cases1,2. Some case series of papillectomy of the minor papilla report that this measure was not used5, while others report its use6. In the two cases presented here, submucosa was infiltrated with methylene blue diluted in normal saline in order to clearly delimit the lesion and reduce the risk of perforation according to the rationale provided by the physician who performed the procedures.
The goal of papillectomy is the complete resection, in one piece, of the adenoma, which was achieved in the two cases presented here. Postresection recurrence of major duodenal papillary adenomas has been reported in 0 % to 33 % of cases13. At the time of writing this case report, no specific data on recurrence of adenomas of the minor duodenal papilla after papillectomy were found.
Recommendations regarding endoscopic follow-up to rule out lesion recurrence vary. It must be performed using a side-viewing duodenoscope. Kandler & Neuhaus recommend performing a follow-up duedonoscopy every 3 months during the first year, then every 6 months the second year, and finally every year for 3 years2. The American Society for Gastrointestinal Endoscopy (ASGE) guidelines recommend carrying out follow-up studies between 1 and 6 months, and then every 3 to 12 months for at least 2 years1. These recommendations are mainly for postpapillectomy follow-up in major papilla adenomas cases. There are no specific recommendations for minor papilla adenomas postresection follow-up.
Conclusions
This paper presents two cases of patients who underwent endoscopic papillectomy of the minor duodenal papilla and in which complete resection of tubular adenomas with low-grade dysplasia was achieved without any procedure-related complication. In addition, there was no evidence of lesion recurrence at 20 and 24 months, respectively.











 text in
text in