Introduction
Esophageal schwannomas are tumors that develop from perineural components of the Schwann cell nerve sheath in peripheral nerves1. Their incidence is rare, and in most cases they are benign. Histologically, these tumors are characterized by peripheral lymphoid nodules, benign nuclear atypia and spindle-shaped cells2-4.
Esophageal schwannomas account for 1 in 5000 patients with esophageal tumors. They most frequently occur between the third and seventh decade of life, with a male/female ratio of 1:35. Five percent of diagnosed cases can be associated with neurofibromatosis type I, which have an early presentation and the most aggressive prognosis6. Clinically, they may be asymptomatic; however, in most cases esophageal schawannoma is diagnosed at an advanced stage, and it mainly manifests with symptoms and clinical signs such as moderate to severe dysphagia and dyspnea, associated with chest pain, epigastric pain, cough, hemoptysis, palpitations and pneumonia, depending on its location and mass effect6.
Regarding its diagnostic approach, imaging studies (X-rays, computed tomography [CT] scans, magnetic resonance imaging [MRI]) provide more information on the anatomical characteristics of the tumor. However, these findings do not allow differentiating a schwannoma from other submucosal tumors, for they share similar imaging characteristics7. A correct diagnosis relies on histopathological studies and immunohistochemistry tests, being S-100 the tumor marker with the highest specificity and sensitivity for this disease, provided that in all the schwannoma case reports described in the literature this marker has been positive compared to other markers6,8.
Clinical case
This is the case of a 38-year-old woman who had experienced dysphagia for one year, together with occasional episodes of hematemesis; for this reason, she underwent an upper gastrointestinal endoscopy in which a 12 cm long endoluminal, friable and irregular lesion located 27 cm from the dental arch was observed and from which a sample was taken for histopathological purposes. A benign lesion compatible with leiomyoma was described in the histopathology report. In addition, a 128 mm x 66 mm x 84 mm (L x AP x T) tumor mass located in the cervical esophagus, extending to the transmural thoracic esophagus, was observed in a contrast enhanced CT scan of the chest. The lesion was exophytic, with homogeneous enhancement depending on the anterior wall, conditioned the obstruction of the light and exerted a mass effect on the trachea in approximately 70% (Figure 1A and B).
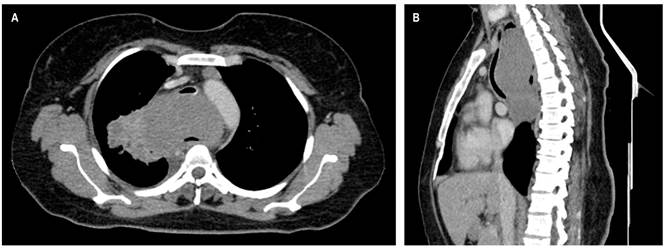
Figure 1 Contrast enhanced chest CT scan. 128 x 66 x 84 mm (L x AP x T) mass located in the middle mediastinum, without significant enhancement after the administration of the contrast medium. The mass is homogeneous, has partially defined lobulated contours, and extends from C7 to T7 with a compressive effect on the adjacent mediastinal structures, especially the trachea, that displaces the tissue in an anterior direction with a decrease in its caliber of approximately 73%; and in the esophagus, where its lumen is partially observed. Prevascular subcentimeter lymph nodes, where the largest one has a short axis of 8 mm; para-aortic lymph nodes with a short axis of 10 mm are also observed. A. Axial view. B. Sagittal reconstruction.
The case of the patient was taken to the medical-surgical board because of concerns regarding the histopathological findings, so performing a new biopsy of the mediastinal lesion was decided, which was achieved by means of a thoracoscopy. The following findings were informed in the biopsy report: a spindle cell tumor with immunoprofiling that favors the peripheral nerve sheath tumor without clear criteria of cellular atypia (Figure 2) and positive immunohistochemistry for S100 protein and negative for acute myelogenous leukemia (AML), H-Caldesmon, desmin, CD117, DOG-1, CD34, CKAE1/AE3 and STAT-6. The cell proliferation index (Ki-67) was 5%, so it was concluded that the mass was compatible with an esophageal schwannoma. A new contrast enhanced CT scan of the chest showed an increase in the size of the mass with involvement of the mediastinal pleura and the right apical pulmonary parenchyma, in direct contact with the right pulmonary artery, the aortic arch and the azygos vein arch. The case of the patient was presented again before the surgical board (thoracic, oncological and esophageal surgery services), where, after assessing the case, the tumor was deemed surgically unresectable due to its size and vascular involvement. She was referred to the clinical oncology service to consider another therapeutic option aimed at reducing the severity of her symptoms. In addition to the symptoms and clinical signs described here, the patient experienced several pneumonia episodes during the course of the disease that required inpatient antibiotic treatment and mechanical ventilation (Figure 3).
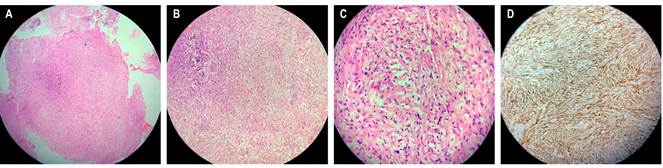
Figure 2 Microscopic study. Neoplastic lesion consisting of spindle cells and some pleomorphic cells on a fibrocollagenous stroma associated with the presence of lymphocytic inflammatory infiltrate. A. Hematoxylin-eosin (HE; 4X magnification) staining. B. HE staining (X10 magnification). C. HE staining (40X magnification). D. Positive immunohistochemistry for S100 protein.
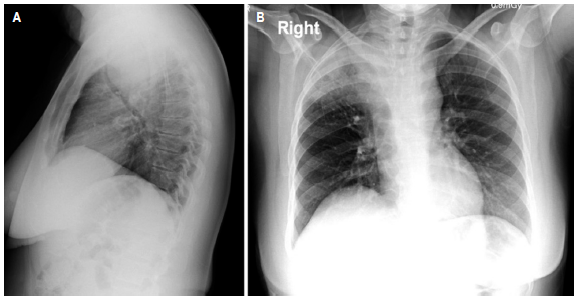
Figure 3 Chest X-ray. Mass located in the middle mediastinum with an internal air component in its upper region that does not rule out cavitation; this image communicates with adjacent consolidation of the right upper lobe, which does not rule out a fistulous tract. The mass produces an important compressive effect on adjacent structures, especially the trachea, with a decrease in its caliber of approximately 73%. Mass with involvement of the mediastinal pleura and the right apical pulmonary parenchyma, in direct contact with the right pulmonary artery, the aortic arch and the azygos vein arch without signs of infiltration. A. Lateral view. B. Posteroanterior view.
Discussion
Primary esophageal tumors represent 2 % of cases; of these, 80 % are leiomyomas and only 1 %, schwannomas; the remaining percentage corresponds to other histopathological types2,8,9. Esophageal schwannomas are rare and mostly benign. So far, 54 cases have been described in the literature, 6 of them being malignant; when comparing these reports it was found that our patient was in the age range between 30 and 60 years6, but with indeterminate histological characteristics to classify the tumor as benign or malignant, since spindle cell components and some pleomorphic cells without clear criteria of atypia on a fibrocollagenous stroma associated with the presence of lymphocytic inflammatory infiltrate were found in the microscopic study, which could preliminarily suggest a benign mass, and, in the immunohistochemistry tests, a positive result was obtained for S-100 protein, the gold standard for diagnosing schwannoma, although a cell proliferation index (Ki-67) of 5% was also reported, which is higher than the average described in the literature (2%-3%)10. From the above, an unusual development of rapid progression could be deduced, taking into account that several authors propose the presence of malignancy when there is a mass with an axis greater than 60 mm6. In the case reported here, a mass with 66 mm in its shortest axis was observed in the diagnostic imaging studies, which suggests malignancy.
In the literature it is common to find cases of patients with a history of masses that are first diagnosed as leiomyomas; however, if their evolution is unusual, a new biopsy, performed using another technique, is indicated when schwannoma is suspected4,8,11. This diagnostic approach is necessary because most of endoscopic biopsies are superficial, so that mainly submucosal tissue is found, without really obtaining components of the peripheral nerve sheath12. In this type of tumor, the technique used to obtain the sample for pathological and immunohistochemistry purposes is of great importance. In our case, the sample was obtained by thoracoscopy, but the initial approach was similar to what has been described in the literature, since a preliminary diagnosis of leiomyoma was made, and then, after an interdisciplinary assessment was made, a new biopsy was requested in order to confirm the schwannoma diagnosis. This could explain the underreporting of this type of tumor.
Regarding computed tomography scan findings, schwannomas share characteristics with other esophageal tumors, but they appear as rounded or oval images with defined borders, attenuation equal to or less than soft tissues, homogeneous or heterogeneous enhancement to the contrast medium depending on the presence of lipid content in the Schwann cells), trapped perineural adipose tissue and cystic spaces or small calcified areas, which are found in 5% to 10% of cases13. The findings reported in our case are similar to those described above, but the extension of the tumor to adjacent structures such as the trachea (70% obliteration); an esophagus with a slight appreciation of its lumen and the mass effect on the aortic arch, the right pulmonary artery and the arch of the azygos vein may condition the approach to be implemented.
Esophageal schwannomas are not radiosensitive or chemosensitive, but they can be surgically resected through procedures such as right or left posterolateral thoracotomy, video-assisted thoracoscopic surgery, and robot- and video-assisted thoracic surgery plus enucleation or esophagectomy5, depending on the tumor size, and the involvement of the esophagus and other adjacent structures. Even in the malignant schwannoma cases that have been reported, surgical treatment was implemented obtaining favorable outcomes and no evidence of recurrence was described12. In our case, however, surgery was ruled out given the size of the tumor and the involvement of different mediastinal structures. Surgical management of leiomyoma is similar to that of schwannoma9; in our opinion, this situation, together with the underreporting of schawannoma due to poor biopsy samples collection, facilitates said underreporting.
Currently, the patient continues to attend periodic check-up visits in order to monitor how much the functionality of her esophagus and trachea has been affected due to the mass effect exerted by the tumor. In addition, she is awaiting the concept by the clinical oncology service to evaluate possible management alternatives.
Conclusion
We report a case of esophageal schwannoma with a rare initial clinical presentation, S-100 marker positivity and a Ki-67 higher than what has been described in the literature; however, the patient did not show conclusive radiological or anatomopathological characteristics of malignancy, so that treatment was limited, with surgical management, the most appropriate therapeutic option, being ruled out.
Leiomyomas are the most frequent primary esophageal tumors, but obtaining a biopsy sample through an appropriate technique is of great importance, as well as achieving an anatomopathological and immunohistochemical analysis that specifies with certainty the type of histology associated with the clinical and radiological characteristics of the patient; however, in patients with a rare clinical presentation, esophageal schwannoma is a differential diagnosis in cases of primary tumors of the esophagus.











 text in
text in 



