Introduction
Endoscopic retrograde cholangiopancreatography (ERCP) is a minimally invasive procedure used as a therapeutic method to treat different biliary or pancreatic diseases. It was created in 1968 to visualize the biliary tree and since 1974 it has made possible to make approaches to the ampulla of Vater, such as papillotomy1-3. However, it is not a harmless procedure, since complications occur in 2.5% to 8% of cases, and it has a mortality rate ranging between 0.5% and 1%1,3. Among these complications, acute pancreatitis (1% to 7%), bacteremia (1.4%), gastrointestinal-biliary tract bleeding (1%), intestinal perforation (1%) and acute cholecystitis (0.2%) stand out in order of incidence1,3. Although mortality due to these complications is not very high (0.5%-1% to 3% according to some case series)1,3, morbidity is high and is represented by prolonged hospital stays, intensive care unit (ICU) admission requirement, among others.
Subcapsular hematoma of the liver after ERCP is a rare complication that can lead to a fatal outcome. Worldwide, most of the literature addressing this complication consists of case reports.
Case report
This is the case of a 68-year-old man with no significant history of disease who was admitted to the emergency department since he had experienced colicky abdominal pain of high intensity in the right hypochondrium for a whole day; no other associated symptoms were reported. The following findings were described on physical examination: abdominal pain in the right hypochondrium on palpation with no signs of peritoneal irritation.
Regarding laboratory tests, altered liver function tests values (elevated AST, ALT and alkaline phosphatase) and normal range amylase levels were reported, while leukocytosis and neutrophilia were evidenced on the complete blood count test. Then a hepatobiliary ultrasound was performed in which cholelithiasis without cholecystitis, biliary mud and prominence of the extrahepatic biliary tract were documented.
With these findings, the patient was classified as having an intermediate risk of choledocholithiasis, so a magnetic resonance cholangiopancreatography (MRCP) was performed, where intra and extrahepatic bile duct dilatation secondary to choledocholithiasis, together with a 9 mm stone in the distal common bile duct were observed.
Therefore, an ERCP was performed which showed an elongated intradiverticular papilla up to the second part of the duodenum. A wire guided cannulation up to the hepatic ducts was attempted using a papillotome; however, after 3 attempts and a Needle knife infundibulotomy, accessing the biliary tract was impossible, so the ERCP was considered to be unsuccessful. Then, 5 days after the first failed procedure, a second ERCP was attempted, where metallic guidewire cannulation up to the hepatic ducts was possible; then, a large ovoid stone was extracted from the common bile duct by means of a wide papillotomy on metallic guidewire (Figure 1). The patient’s condition improved satisfactorily after undergoing the procedure; somehow, 8 hours later he suddenly experienced abdominal pain of high intensity in the right hypochondrium, with no signs of peritoneal irritation.

Figure 1 Intraoperative fluoroscopy - Endoscopic retrograde cholangiopancreatography, access to the biliary tract.
In view of the deterioration of the patient’s clinical condition, a complete blood count test was requested, where anemia with a hemoglobin levels of 6.8 mg/dL and amylase levels within normal limits were reported. Based on these findings and the absence of evidence of active gastrointestinal bleeding, a contrast-enhanced CT scan was performed, which allowed confirming the diagnosis of subcapsular hepatic hematoma (Figure 2).
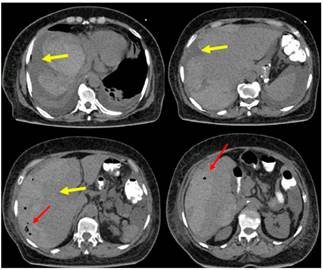
Figure 2 Contrast-enhanced CT of the abdomen. 206×150×70 subcapsular hematoma of the liver; volume: 1168 cc (yellow arrow), with free fluid in the cavity and presence of pneumobilia (red arrow).
After evaluating the clinical condition of the patient and in view of his hemodynamic stability, conservative management consisting of fluid replacement, transfusion of 3 units of red blood cells, intravenous administration of antibiotics and observation at the ICU was initiated.
72 hours after conservative management was started, the patient’s condition improved satisfactorily, achieving hemodynamic stability. A new contrast-enhanced CT scan of the abdomen was requested, where no changes were evidenced with respect to the findings shown in the previous enhanced CT scan. Finally, given the improvement of his clinical condition, he was discharged with indications of using oral antibiotics, analgesics and attending ambulatory follow-up at the general surgery and hepatobiliary surgery service.
Discussion
Endoscopic approach to the bile duct (endoscopic retrograde cholangiopancreatography) is a minimally invasive procedure that, despite being safe and having low mortality rates, has a complications rate up to 7%2,4,5. These complications include gastrointestinal bleeding, which can be clinically relevant and account for 0.1% to 2% of cases3,5, and those that do not involve clinically relevant bleeding, which constitute 10% to 30% of cases5. Even if ERCP is performed by an expert, its performance may be associated with the occurrence of bleeding or hematoma, conditions that can be life-threatening if they are not timely diagnosed5,6.
Post-ERCP subcapsular hematoma of the liver is a rare complication, with available literature consisting of case reports1,5. In 2001, Ortega et al. published the first case report; since then similar cases have been published2.
According to the information we found after conducting a literature review, most patients who present with post-ERCP subcapsular hepatic hematoma are women, with a median age of 59 years; besides, in most patients, symptoms occur within the first 24 hours after undergoing the ERCP, as it happened in the case described here7.
Abdominal pain is its most frequent clinical presentation (91%), followed by anemia (43%), hypotension (29%) and fever (20%); however, it should be noted that some patients are asymptomatic5,8. Computed tomography is the gold standard for confirming the diagnosis of the disease; in addition, involvement of the right lobe of the liver is reported in 95% of cases when using this imaging technique. This systematic review shows that medical treatment is the best management option. A 9% mortality rate has been reported8.
Regarding causality, multiple theories are described, such as accidental puncture of the biliary tree leading to the rupture of the vessels of the hepatic parenchyma or the use of excessive force when extracting the stones1-8.
To best of our knowledge, in this paper we present the case of the largest subcapsular hematoma of the liver that has been reported so far, since its size was 206 × 150 mm (being 100 × 130 mm the average size reported in the literature), and it affected both lobes of the liver1-9.
Treatment depends on the clinical evolution and hemodynamic stability of the patient, as well as on imaging findings4. Multidisciplinary treatment is recommended8.
The following types of treatment can be used: conservative, surgical or interventional radiology1,4.
Conservative management (43.5% of cases) aims at strictly monitoring hemodynamic status1,5. It is indicated in patients with hemodynamic stability and in which the hepatic vein is not compressed by the hematoma4. The use of prophylactic antibiotics is recommended due to the risk of infection of the hematoma, which has been shown to reduce mortality8. Likewise, serial hemoglobin control tests and imaging control studies are recommended3-5,8 (level of recommendation: C).
Management based on interventional radiology is an alternative to surgical treatment. It consists of selective (26% of cases) or superselective embolization of the vessels or percutaneous drainage of the hematoma (17.4% of cases) 5 (level of recommendation: C).
Surgical management (13% of cases) is only indicated in the presence of deterioration of the patient’s general condition, hemodynamic instability, signs of peritoneal irritation, high risk of hematoma rupture, free fluid in the abdominal cavity, contrast media extravasation, failure of conservative management, and extrinsic compression of the hepatic vein1,4,8,9 (level of recommendation: C).
If necessary, follow-up imaging studies should be also performed to evaluate is also performed to evaluate its progression5.
Based on the literature review conducted by us and on the information described by the cases reported worldwide, we can say that the subcapsular hematoma of the liver described in this case is the largest subcapsular hematoma known to date. It is worth noting that conservative management was sufficient to control this complication and that interventional or surgical management were not required. This reflects the importance of multidisciplinary management and the impact of conservative management despite the large size of the hematoma, which must be the standard initial management approach in all subcapsular hepatic hematoma cases.
Conclusions
Post-ERCP subcapsular hematoma of the liver is a rare complication of bile duct endoscopic approach; however, it can be life-threatening if it is not timely diagnosed. Given the low number of cases reported worldwide, its true incidence remains unknown. Somehow, it is a complication that must be included as a differential diagnosis in patients who don’t have a good recovery after undergoing an ERCP. Timely diagnosis is key to prevent a fatal outcome. Finally, it is worth noting that the subcapsular hepatic hematoma presented here is the largest one reported worldwide so far, and that conservative management was successful and must remain as the first-choice treatment, although it must be adjusted to each clinical situation.











 text in
text in 


