Introduction
Bezoars are defined as any object ingested, voluntarily or involuntarily, that lodges somewhere in the upper gastrointestinal tract, most frequently the stomach, and cannot be digested by the physiological mechanisms of the body. Furthermore, they are classified according to their composition1-4. It is an uncommon condition with a nonspecific clinical presentation5.
Bezoars have similar characteristics such as age, anatomical location, underlying disease or excessive intake of a certain element1-3,5-8. There are some bezoars without these characteristics, as they are not concretions of non-digestible material or they do not fit the abovementioned sociodemographic variables, for which they could be considered atypical. However, they exhibit similar clinical signs and symptoms, and represent a high risk for patients in cases of late diagnosis, which is why their management must be optimized(1, 3).
This paper describes the use of laparoscopic management in an atypical bezoar case in which endoscopic management failed; in addition, a literature review is also presented.
Clinical case
This is the case of a 67-year-old man with diabetes, high blood pressure and cirrhosis of the liver who, after being arrested by the National Police of Colombia, was admitted to our health institution for he had experienced nausea and vomiting, associated with asthenia, adynamia and weight loss, for one month. The fact he had been on a trip outside the country for the same period of time he had been experiencing said clinical signs and symptoms stood out. In addition, he reported that before returning to Colombia he had ingested 30 capsules covered with latex and filled with cash, of which he only had expelled 20 capsules. On physical examination the patient was agitated and abdominal distension and generalized abdominal pain on palpation were evidenced; there were no signs of peritoneal irritation.
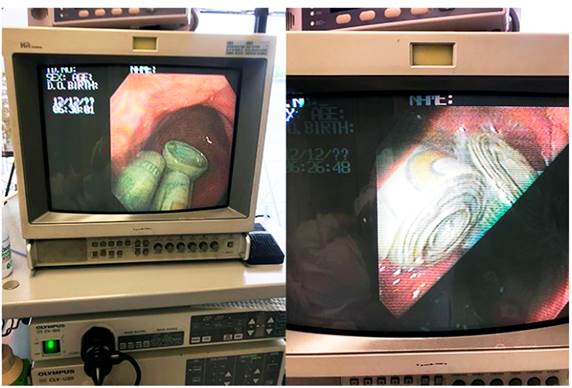
Once the ingestion of the capsule was known to us, instead of performing a diagnostic imaging test, an upper gastrointestinal endoscopy or esophagogastroduodenoscopy (EGD) was indicated as a diagnostic and management method, as shown in Figure 1. During the EGD, an impacted money bezoar without latex coating was found in the prepyloric region, which could not be endoscopically extracted as it was a compact mass of paper money. Laparoscopic extraction was then carried out by means of anterior gastrostomy in the antrum and body of the stomach, which was subsequently closed in 2 planes using 3-0 polydioxanone (PDS) suture with separate stitches using 3 trocars: 2 of 12 mm in the umbilical port and the right flank, and another of 3 mm in the left flank plus a liver retractor, as shown in Figure 2. The gastric content was extracted through the umbilical port using Endo Catch. The patient’s postoperative recovery was adequate, with tolerance to the diet at 12 hours, and being discharged 18 hours after the procedure was completed. One month later, in a follow-up no complications were reported by the patient.

Figure 2 A. Image showing the patient after the money bezoar was extracted by means of laparoscopy. B. Money bezoar after its extraction.
All procedures were performed under the supervision of the scientific and ethical committee of the institution. Besides, all protocols established by the National Police (as the competent control and surveillance body) to ensure the safekeeping of the bezoar were followed. Likewise, the National Police was in charge of carrying out the subsequent administrative procedures.
Discussion
The term bezoar is believed to originate from the Arabic word badzehr or the Persian word panzehr, both of which may mean “countervenom” or “antidote”3. Generally, they are classified according to their composition. There are 4 types of typical bezoars: pharmacobezoars, lactobezoars, phytobezoars and trichobezoars, being phyto and trichobezoars the most common1-3,5-8. However, some literature reviews classify bezoars in 5 types, adding the foreign body bezoar type, including wood chips, resins, starch and persimmons, among others7,8. Risk factors for developing a bezoar are listed in Table 1.
Table 1 Etiological factors for the development of bezoars1-13
This is a rare disease: it occurs in 0.06% to 4% of the population9. The age of patients with bezoars ranges from 16 months to 79 years1,3; besides, 90% of patients are young adult women, mostly with psychiatric disorders7.
Between 5 % and 12 % of patients who undergo a gastrectomy present with bezoars6; likewise, this disease accounts for 0.4 % to 4.8 % of mechanical intestinal obstruction (IO) cases in the adult population2,3,6,9, and in 1.1 % its clinical presentation corresponds to acute abdomen that requires surgical treatment1,3. According to different case series of bezoars found as incidental findings during endoscopy, it has a prevalence between 0.4 % and 0.6 %7.
Bezoars can be found in any part of the gastrointestinal tract, although most of them are located within the stomach3,5,10, as it was the case of our patient, in which the bezoar was impacted in the prepyloric region. Tricobezoar is another example of intragastric bezoars; when this type of bezoar extends through the pylorus to the jejunum, ileum and sometimes colon, it is known as the Rapunzel syndrome, although it should be noted that its occurrence is very rare1,2. Bezoar impaction in the narrowest segment of the small intestine, 50-75 cm from the ileocecal valve, is also common3,6.
An atypical bezoar is a bezoar that does not match the aforementioned parameters. As shown by Masaya Iwamuro et al.10 who reported the case of a bezoar made up of gallstones, the concept of atypia in bezoars might correspond to those with an endogenous origin10.
Ideally, diagnosis must be early. The aim is to avoid complications associated with OI such as intestinal perforation, that may endanger the patient’s life. According to the literature, bezoars diagnosis can be reached using ultrasound, CT scans or EGD11-13. Audel Pedroza et al.4 reported the case of a 39-year-old woman who had sought medical assistance on several episodes due to acute pancreatitis, and in which a toothbrush impacted in the duodenum was found during a biliopancreatic endoscopic ultrasound4. As in the case of our patient, diagnosis was made endoscopically, although endoscopy was not a practical tool for extraction. Bezoars are usually asymptomatic until acute OI occurs1. The occurrence of OI as a clinical manifestation of a bezoar will depend on its location9. According to the literature, abdominal pain is the most common clinical sign (49%-100%), with a history of nausea and vomiting (35%-75%), bloating, constipation, epigastric pain and fever3,6,5,8; other less frequent symptoms include weight loss, anorexia, hematemesis and intussusception5. Our patient did not experience abdominal pain, but he did suffer from nausea, vomiting and weight loss. Despite these are variable clinical signs, all these symptoms must be considered for making a bezoar diagnosis.
Bezoars are mainly removed through enzymatic methods, endoscopy and open or minimally invasive surgery3. In the case of our patient, as well as in the case described by Audel Pedroza et al.4, endoscopy was not an appropriate tool for extraction, because the material of the bezoar did not allow traction. For this reason, similar to our decision, Audel Pedroza et al.4 chose to perform a laparoscopy4, but unlike them we used a 3-port laparoscopic approach, since there is an advanced laparoscopy expert in our institution. The choice of treatment is oriented to the case of the patient. The material, size and location of the bezoar, as well as the physiological characteristics of the patient must be taken into account3.
Laparoscopy has been used in a small series of patients with bezoar-induced IO, with a significantly short operative time, although it often involves exploratory laparotomy, with or without enterotomy, for the subsequent extraction of the bezoar2,6. During surgery, a thorough exploration of the abdominal cavity must be performed to extract concomitant gastric or intestinal bezoars6.
Conclusions
Atypical bezoars are those that deviate from the characteristics normally found in bezoars such as age, location and composition, as well as from the common characteristics of their concretion. Although they rarely occur, they can be life-threatening due to complications derived from IO, so assessing the possibility of IO is crucial at the time of diagnosis, which in turn must be based on a complete anamnesis and imaging tests, of which EGD stands out. Regarding its treatment, laparoscopic management is ideal in cases in which endoscopic intervention is not sufficient.











 text in
text in