Introduction
Villous adenomas have been described as polypoid, preneoplastic lesions that account for 5 to 15 % of adenomatous polyps. They exhibit a papillary and villous architecture with a high tendency to dysplasia associated with a high mitotic activity and epithelial renewal, with malignant transformation rates up to 72 %. They are frequently found in the colon or the rectum; however, a few cases of villous adenomas occurring in the upper digestive tract, especially in the esophagus, have been described1,2. The finding of this type of lesions in an ectopic gastric mucosa patch in the cervical esophagus has been described in few cases; besides, these lesions are frequently underdiagnosed, since they are located in an area in which decreased endoscopic occurs due to the rapid passage of the endoscope. Furthermore, these adenomas are considered to be congenital, and therefore it is believed they have a low malignant potential2,3.
The case of a patient with a villous adenoma found in an ectopic gastric mucosa patch located in her cervical esophagus is presented. Likewise, a review of the literature about this rare condition was performed1-3.
Clinical case
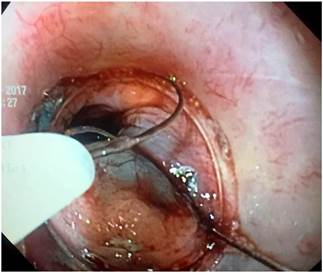
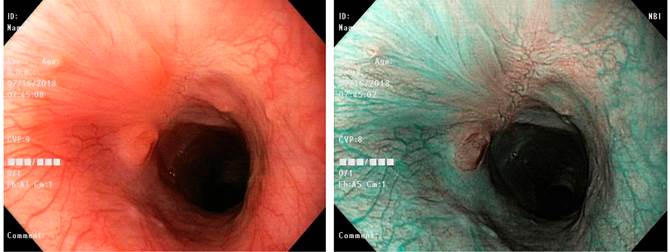
This is the case of a 41-year-old man with a family history of stomach cancer (mother) and a history of hemorrhoidectomy and chronic gastritis. Two years before visiting our institution for consultation he had been treated for Helicobacter pylori infection. The reason for consultation was the presence of epigastric pain and intense heartburn, predominantly at night, for six months. The patient denied having experienced emesis or digestive bleeding episodes. In addition, during the consultation, he provided the treating physician with the results of an esophageal scintigraphy he had undergone and in which at least 10 episodes of gastroesophageal reflux were reported, being the most significant a 10-second episode that extended to the proximal third of the esophagus. During white light endoscopy, 2 islands of salmon-colored antral-like mucosa with well-defined borders were observed in the cervical esophagus and immediately below the upper esophageal sphincter, being the largest one about 18 x 26 mm in size. On narrow band imaging (NBI) evaluation, these 2 islands of columnar mucosa were clearly visible and, in addition, 2 small patches of adenomatous-like whitish and slightly raised mucosa were observed at the upper end of the largest island. The gastric cavity showed isolated prepyloric erosion and chronic gastropathy with multifocal atrophy (Figure 1).
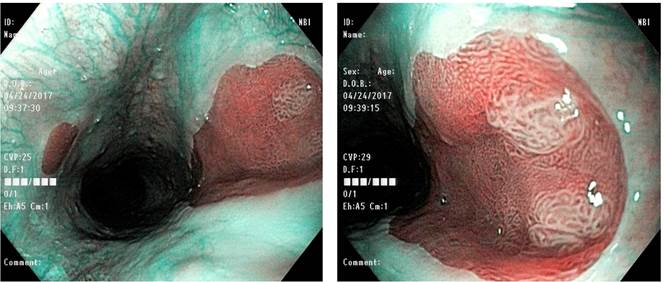
Figure 1 Ectopic gastric mucosa patch located in the cervical esophagus, with 2 islands of adenomatous-like tissue (NBI).
Chronic atrophic gastritis, positive H. pylori, esophagitis and a lesion suggestive of villous adenoma were described in the histopathological report. First-line triple therapy for H. pylori infection was indicated.
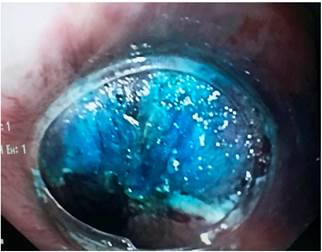
Endoscopic submucosal dissection (ESD) was scheduled to resect the lesion. During the procedure, and possibly due to the scarring process secondary to the samples taken for biopsy purposes, the lesion was not successfully raised after injecting it with indigo carmine saline solution; for this reason, the resection technique was changed and complete resection was performed using the endoscopic mucosal resection (EMR) Kit Model K-009 by Olympus (injector, cap and polypectomy loop) and the ERBE VIO 200 S electrosurgical unit (endocut Q mode, level 3 effect, cut duration 1 and a cut interval 6) (Figure 2). Finally, the ectopic gastric mucosa patch was completely resected in 4 fragments, including the adenomatous tissue foci. No residual columnar epithelial tissue was observed and ablation of the resection borders was not performed due to the absence of bleeding and the fact that columnar mucosa itself is not a premalignant lesion (Figure 3).
The resected fragments were sent to the histopathology service for analysis. The larger ones were extended on a piece of cork and fixed with pins.
The following findings were informed in the histopathology report: esophageal mucosa affected by a dysplastic lesion made of tubular and villous glands, lined by a simple cylindrical epithelium, hyperchromatic nuclei without evidence of polarity loss or basement membrane involvement. Scarce low grade dysplasia chronic inflammatory infiltrate compatible with villous adenoma was observed in the lamina propia (Figures 4 and 5).
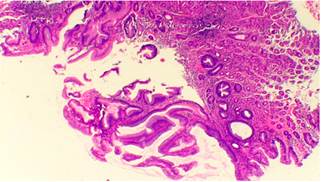
Figure 4 Microscopic image. Hematoxylin-eosin stain: 10 x magnification. Findings compatible with villous adenoma.
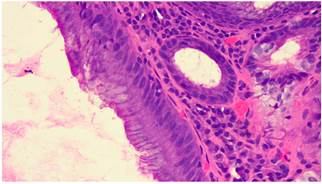
Figure 5 Microscopic image. Hematoxylin-eosin stain, 40x magnification. Findings compatible with villous adenoma.
The patient’s clinical condition improved satisfactorily and he did not experience any gastrointestinal symptoms or postoperative bleeding episodes. Finally, a control endoscopic procedure carried out 6 months after the lesion was extracted evidenced the presence of a whitish tissue associated with reepithelialization in the esophagus, as well as a small central kissing scar and a small columnar mucosa island (5 mm). No other abnormal findings were described (Figure 6).
The patient is still being monitored by the gastrointestinal surgery group and shows an adequate clinical evolution.
Discussion
Neoplastic polyps, also known as adenomas or adenomatous polyps, are premalignant lesions that can turn into adenocarcinomas. They are classified as tubular, tubulovillous and villous adenomas, being a dysplastic epithelium their histological feature. They are further subdivided into low and high grade dysplasia lesions based on the type of dysplasia, the level of nuclear agglomeration and hyperchromasia, according to their mitotic activity, cytoplasmic differentiation and distortion of cellular architecture. Tubular adenomas present between 0 % and 25 % of villous histology; tubulovillous adenomas, between 20 % and 75 %; and villous adenomas, between 75 % and 100 %1-4.
Villous adenomas usually have a papillary villous architecture, which has been associated more with lesions > 2 cm. This type of polyp occurs in both men and women, especially in the sixth and seventh decades of life. They are characterized by being long glandular structures extending from the surface to the center of the polyp. This subtype is associated with larger adenomas, more severe degrees of dysplasia and a greater tendency to malignancy, with malignant transformation rates of up to 72% being described4-6. They account for 5-15% of all adenomas and occur most frequently in the rectum and the sigmoid rectum, with only a few reports of their occurrence in other parts of the digestive tract1,2,4.
This condition is probably underdiagnosed and its clinical relevance is not entirely clear, since a significant proportion of patients do not report related symptoms. Although endoscopic findings may suggest a neoplastic potential, the degree of malignancy of the lesion can be only determined through histopathological analysis1. Gastric villous adenomas are asymptomatic lesions in more than 90% of cases, but they can cause clinical manifestations such as gastrointestinal bleeding, anemia, abdominal pain or pyloric syndrome. Despite the antrum is their most frequent gastric location, case series such as those conducted by Miller et al. show that villous adenomas can also be found in the gastroesophageal junction4,5,7.
In the case reported here, 2 lesions located on an ectopic gastric mucosa patch in the cervical esophagus and with endoscopic findings compatible with adenomatous neoformations were identified. These ectopic gastric mucosa patches are relatively frequent findings, but their prevalence varies greatly in the literature, with figures ranging from 0.18% to 1.6%. This discrepancy could be explained by the fact that these areas are frequently overlooked or ignored during endoscopic examinations10,11,13. These islands of ectopic gastric mucosa have been associated with a congenital origin and with a low intrinsic tendency to develop malignancy. Despite this, more than 50 cases of adenocarcinomas growing from ectopic gastric mucosa patches were reported between 1950 and 20168,9,11,16.
Tomohiro Kadota et al. found a total of 27 cases of esophageal adenocarcinomas that formed from islands of ectopic gastric mucosa in patients aged 43-83 years, with dysphagia being the main symptom11,12. In 96% of cases, the neoplastic lesion was located in the cervical esophagus or the upper thoracic esophagus, the preferred location of ectopic gastric mucosa patches. The main histopathological subtypes were well-differentiated and moderately differentiated adenocarcinomas, and the presence of gastric ectopic tissue adjacent to the lesion was observed in all cases13-16.
Ectopic gastric mucosa patches are not adaptive processes of esophageal tissue, but areas of gastric mucosa sequestered in the esophagus after a columnar epithelium is replaced by stratified squamous esophageal epithelium in an embryologic replacement process. However, the presence of intestinal metaplasia, described between 0 % and 12 % of cases, would indicate that these areas of gastric mucosa may also undergo transformation processes after being exposed to certain deleterious stimuli and represent preneoplastic conditions8-15.
Different theories have been proposed to explain the pathophysiological changes sequence that causes an ectopic gastric mucosa island to turn into an adenocarcinoma, such as the metaplasia-dysplasia-adenocarcinoma sequence; besides, the presence of H. pylori has also been associated with predisposition to malignant transformation. However, the low malignancy rates of these lesions when compared to conditions such as Barrett’s esophagus have led to the conclusion that ectopic gastric mucosa islands, per se, are not premalignant lesions8-10,16,17.
The case reported case, which is one of the first cases described in Colombia, helps to reflect that, although rare, there is a risk of developing potentially malignant lesions in ectopic gastric mucosa patches, which have been traditionally described as having a low tendency to malignancy.
Conclusions
In patients undergoing endoscopic studies, mainly those with gastroesophageal reflux disease, careful evaluation of the esophageal mucosa, especially in the cervical esophagus, aimed at identifying ectopic gastric mucosa patches is suggested. It is of utmost importance to remember that one of the specific quality indicators of esophagogastroduodenoscopy is the performance of a complete examination of each of the structures (esophagus, stomach and second part of the duodenum, including retroflexion of the stomach), which, in addition, must be clearly documented in the final report18.
Ideally, this area must be evaluated using narrow band imaging (NBI), a technique based on the modification of the bandwidth of the emitted light, which allows obtaining additional information on the mucosa and the morphology of the superficial vessels. Thus, NBI is useful to identify areas of suspicious tissue of neoplasm in the squamous epithelium of the esophagus19.
Careful endoscopic evaluation of esophageal gastric heterotopias is indicated for the assessment of findings suggestive of premalignancy. If mucosal irregularity is identified, samples must be taken for performing both a biopsy and complementary histopathological studies. The identification of adenomas in esophageal mucosa must be indicated for endoscopic resection; their percentage of villous histology will be associated with their malignant potential.
Take home points
In patients scheduled for upper endoscopy and especially those presenting with any upper esophageal symptom such as dysphagia, globus pharyngeus or gastroesophageal reflux, it is suggested to perform a detailed and careful evaluation of the cervical esophageal mucosa and, if possible, to use any digital chromoendoscopy technique to facilitate the identification of ectopic gastric mucosa patches.











 texto en
texto en