Introduction
Appendicitis is defined as inflammation of the vermiform appendix, the most common cause of acute abdomen (approximately 60%). Thus, appendectomy is the most performed emergency surgery worldwide1-4. It has been estimated that the risk of having this disease throughout life is approximately 12%2,3,5, with young people under 29 years of age making up 45% of patients4,6-9.
This pathology occurs due to inflammation of the cecal appendix, secondary to the obstruction of its lumen by fecaliths, lymphoid hyperplasia, tumors, parasites, among others. It disrupts local blood flow, irritating the adjacent peritoneum and causing pain. Finally, it results in a perforation of the anatomical structure, releasing intestinal content into the abdominal cavity and causing complications, such as peritonitis, sepsis, shock, and, in some cases, death10-12. The clinical picture must be known and the pathology identified in time to avoid this. However, there is a great variety of manifestations among individuals, age groups, and genders. There are also several differential diagnoses to consider, leading to a wrong or late diagnosis in one out of five patients13-17.
To make a timely diagnosis and reduce the rate of complications in patients with appendiceal pathology, the clinical component must be considered, together with diagnostic tests (paraclinical tests). They can reduce the error from an estimated 22% to 5%, representing a cost reduction of up to 200,000 euros per year18. Numerous scales have been developed to help the clinician recognize which patients with abdominal pain are more likely to have the disease. The available scales include the Alvarado score, the pediatric appendicitis score (PAS), and the RIPASA score, which assign scores to clinical manifestations and incorporate laboratory test results18-21. However, there is no biomarker with optimal performance that effectively diagnoses acute appendicitis (AA) or can predict its severity or complications19-21.
This article aims to analyze the potential markers of severity in AA for diagnostic purposes and timely management of surgical diseases in emergency services.
Materials and methods
Population
The study group comprised the entire population with a diagnosis of AA treated at the Hospital Regional de la Orinoquía (HORO) in Yopal between January 1, 2013, and December 31, 2018. It will be identified using the international code of diseases (ICD-10) as follows: K37 (Unspecified appendicitis); K35.9 (Acute catarrhal, fulminant, gangrenous, obstructive, retrocecal, and suppurative appendicitis); K35.1 (Acute appendicitis with peritoneal abscess); K35.0 (Acute appendicitis, perforation, peritonitis, or rupture); A06.8 (Amoebic appendicitis); and K36 (Obstructive appendicitis).
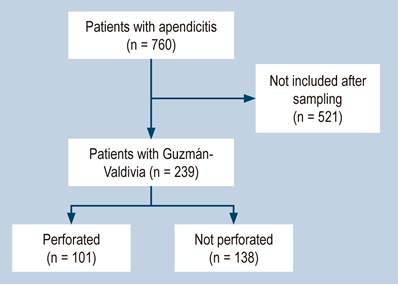
To calculate the sample, the following variables were considered: The population served according to the institution’s clinical records was 760 people diagnosed with appendicitis, the prevalence of appendicitis of 24.6%22, the margin of error of 5% and 95% confidence interval (95% CI). As a result, 239 people were included in the study, who were selected by simple random probabilistic sampling.
Inclusion criteria
The population treated at the HORO from 2013 to 2018 with an Alvarado score22 was included. A score of 5 to 6 is compatible with the diagnosis of AA; 7 to 8 indicates probable appendicitis; and 9 to 10 indicates a very probable appendicitis, together with imaging (ultrasound or tomography) and histopathological studies to confirm the diagnosis. In addition, the Guzmán-Valdivia scale was considered according to the intraoperative findings.
Exclusion criteria
We excluded medical records with incomplete or nonexistent blood count (BC), C-reactive protein (CRP), neutrophil/leukocyte ratio (NLR), and minors (18 years) from the study.
Variables
Based on Calvo et al’s study23, a list of variables was established, including sociodemographic (sex, age, rural or urban origin), clinical (acute pain in the epigastrium radiating to the right iliac fossa, fever) and paraclinical (leukocyte count >11,000, neutrophil percentage > 85%, lymphocyte percentage > 10%, NLR > 5.5, and CRP > 15 mg/dL) data.
Statistical analysis
The database was registered in Excel, version 2013, and analyzed in the statistical package SPSS, version 22. The univariate analysis was performed using a descriptive statistic for the selected population, and the absolute and relative frequencies of the categorical variables were determined. In the case of quantitative variables, we calculated measures of central tendency (mean, median) and dispersion (standard deviation and interquartile range) according to the distribution of the variable.
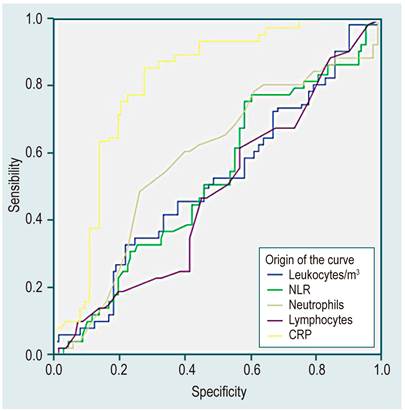
The cut-off value for leukocyte count (> 11,000/mm3), neutrophil percentage (> 85%), lymphocyte percentage (> 10%), CRP (> 15 mg/dL), and NLR (> 5.5) were determined using ROC curves (receiver operating characteristics) using SPSS software, version 22, to differentiate severe from uncomplicated cases. Finally, to determine the possible associations between the categorical variables, tetrachoric tables were made with diagnostic Odds Ratio measurement and their respective 95% CI (< 1 as a predictor of mild (without perforation); > 1 as a predictor of severe (perforation); and one without association). Additionally, we estimated the operating characteristics (sensitivity, specificity, positive predictive value, and negative predictive value) of the paraclinical tests performed more frequently during the hospitalization of patients with AA.
Biases
The risk of bias is deemed low since the scale used as the reference method (Guzmán-Valdivia) is based on the findings during the surgical procedure. These findings are classified into four grades (0: No appendicitis (prophylactic appendicitis, no post-surgical antimicrobial scheme); Ia: Edematous and engorged, Ib: Abscessed or phlegmonous (with seropurulent fluid around the appendix), Ic: Necrotic without perforation; II: Perforated with localized abscess; III: Complicated appendicitis with generalized peritonitis). It maintains a low risk of error and the dichotomization to assess severity. In the case of the qualitative variables, they were taken as dichotomous to analyze and adequately calculate the operating characteristics, which facilitated the assessment and grouping of the participants.
Results
Two hundred thirty-nine medical records of patients diagnosed with AA were evaluated (Figure 1).
Sociodemographic characterization
The population’s average age was 26.35 years, with an SD ± 6.4 years (coefficient of variation of 24%), ranging from 18 to 46 years. Table 1 shows the characteristics of the population.
Table 1 Population characteristics
| Variable | N | % | 95% CI | |
|---|---|---|---|---|
| Sex | ||||
| Female | 127 | 53 | 46.81 | 59.46 |
| Male | 112 | 47 | 40.54 | 53.19 |
| Residence | ||||
| Urban | 155 | 64.8536 | 65.21 | 79.31 |
| Rural | 84 | 35.1464 | 29.09 | 41.2 |
| Grade according to the Guzmán-Valdivia scale | ||||
| 1a | 65 | 27.1967 | 21.56 | 32.84 |
| 1b | 51 | 21.3389 | 16.15 | 26.53 |
| 1c | 22 | 9.20502 | 5.54 | 12.87 |
| 2 | 32 | 13.3891 | 9072 | 17.71 |
| 3 | 69 | 28.8703 | 23.13 | 34.62 |
Regarding the characteristics of inflammatory reactants, we observed that the mean value of the leukocyte count was 15,512.2/mm3, with an SD ± 5,386.84/mm3 (minimum of 1,904.1/mm3; maximum of 32,000/mm3). The percentage of neutrophils had a mean value of 12.625, with an SD ± 5,338.36/mm3 (minimum of 1,294.72/mm3; maximum of 27,840/mm3). The lymphocytes had a mean value of 2,271.28/mm3, with an SD ± 2,125.6/mm3 (minimum of 443/mm3; maximum of 17,908/mm3).
Meanwhile, the NLR had a mean of 8.5, with an SD ± 6.8 (minimum of 1; maximum of 31). The CRP had a mean of 47.46 mg/dL, with an SD ± 60.7 mg/dL (minimum of 0.50 mg/dL; maximum of 316 mg/dL).
A ROC curve was performed to determine the most precise cut-off point for each of the variables. The following values were found: Leukocyte count > 11,000/m3; neutrophil percentage > 85%; CRP > 15mg/dL; percentage of lymphocytes > 10%; and NLR > 5.5 (Figure 2).
Diagnostic tests
In total, 101 people had severe grades of appendicitis, equivalent to 42.2% of people having appendiceal perforation. According to the results, patients with a percentage of neutrophils > 85% are two times more likely to have intestinal perforation, while patients with CRP > 15 mg/dL are 14 times more likely to have this complication (Table 2).
Table 2 Tetrachoric table between the paraclinical with histopathology
| Paraclinical test | Acute appendicitis | Diagnostic OR | 95% CI | |
|---|---|---|---|---|
| Perforated (n = 101) | Not perforated (n = 138) | |||
| Leukocyte count > 11,000 | 79 22 | 107 31 | 1.04 | 0.56;1.93 |
| Neutrophil percentage > 85% | 55 46 | 47 91 | 2.17 | 1.28;3.66 |
| Lymphocyte percentage > 10% | 68 33 | 93 45 | 0.99 | 0.57;1.72 |
| NLR > 5.5 | 62 39 | 78 60 | 1.22 | 0.82-1.52 |
| CRP > 15 mg/dL | 88 13 | 44 94 | 14.46 | 7.3;28.6 |
Characteristics of diagnostic tests
Lastly, we found that the tests with the greatest capacity to detect people with appendiceal perforation (sensitivity) were CRP and leukocyte count greater than 11,000/mm3, with 87.13% and 78.22% data, respectively (Table 3).
We could determine that the tests with the best capabilities to detect people with non-perforated appendix (specificity) were CRP and the percentage of neutrophils > 85%, with 68.12% and 65.94% data, respectively (Table 3). Finally, the highest diagnostic accuracy test was CRP, with 76.15% (Table 3).
Table 3 Characteristics of diagnostic tests
| Operating characteristics | Leukocytes | Neutrophils | Lymphocytes | NLR | CRP |
|---|---|---|---|---|---|
| Sensibility | 78.22 % | 54.46 % | 67.33 % | 61.39 % | 87.13 % |
| Specificity | 22.46 % | 65.94 % | 32.61 % | 43.48 % | 68.12 % |
| Positive predictive value | 42.47 % | 53.92 % | 42.24 % | 44.29 % | 66.67 % |
| Negative predictive value | 58.49 % | 66.42 % | 57.69 % | 60.61 % | 87.85 % |
| Diagnostic accuracy | 46.03 % | 61.09 % | 47.28 % | 51.05 % | 76.15 % |
| Likelihood ratio of a positive test | 1009 | 1599 | 0.999 | 1086 | 2733 |
| Likelihood ratio of a negative test | 0.9697 | 0.6907 | 1002 | 0.8881 | 0.189 |
Discussion
In the present study, the population studied represents a relatively young population, with an average of 26.35 years. It allows comparing it with other epidemiological data from other studies, as is the case of Cánovas et al and Escalona et al, who determined that the average age of appendicitis was 21 and 29 years, respectively24,25. Therefore, no significant difference in the results obtained marks a great difference from Jonge et al’s study, with an average of 55 years26.
Moreover, most people diagnosed with AA were women, 53% of the population, consistent with the results shown by other publications, such as Jonge et al’s26, in which the base population was female (51.2%). Even so, in other studies, most patients are male, as is the case of Padierna et al’s, with 50.81%27. However, there are no significant differences in gender regarding AA. It should be mentioned that the female sex presents a greater difficulty for diagnosis during the fertile age or pregnancy28,29. Another important characteristic is that more patients come from urban areas than rural areas.
Numerous studies document that the pathophysiological stages of appendicitis can be divided into three groups according to the time of clinical evolution, as follows: Incipient (0-12 hours), acute (12-24 hours), and perforated (24-48 hours)1,4,10.
This study did not seek a relationship between clinical evolution and perforation; nonetheless, we compared the results of the different stages of the Guzmán-Valdivia classification30. This comparison indicates that the higher the grade, the greater the severity, just like Martínez et al’s research, which obtained the following results: Grade 0: 4; Grade 1A: 26; Grade 1B: 32; Grade 1C: 27; Grade 2: 22; and Grade 3: 11, for a total of 122 patients31.
From these results, we could determine that they were superior in our study at a percentage level, with a percentage difference in Grades 1A (5.88%) and 3 (19.96%). They suggest that the most severe complication, perforation with generalized peritonitis, occurred more frequently compared to the study above. Other studies found that perforation had a prevalence of 10% (Rigual et al)19 and 24% (Beltrán et al)4, but it is still higher in this research, with a prevalence of 42.25% in perforations.
Regarding the inflammatory reactants, we found that leukocytosis and neutrophilia were related to the diagnosis of AA. According to the results obtained in this study, a percentage of neutrophils > 85% increases the possibility of an outcome of appendiceal perforation (OR 2.17; 95% CI 1.28-3.66) (Table 2). Similarly, an NLR greater than 5.5 over the reference value was found in patients diagnosed with AA (OR 1.22; 95% CI 0.82; 1.52).
It is noteworthy that patients with AA were found to have a significant positivization of the CRP (mean of 47.46 mg/dL). For this study, the population with a CRP > 15 mg/dL had statistically significant OR (OR 14.46; 95% CI 7.3-28.6), which corroborates the findings in other publications. About the usefulness of this marker as a diagnostic aid, the research by Ishizuka et al analyzed the relationship of NLR with gangrenous and perforated appendicitis in 314 patients. It established a figure of eight as the cut-off point, with a sensitivity and specificity of 73% and 39%, respectively32, results lower than our study’s.
Therefore, we can conclude, according to the results of this study, that the diagnostic tests with better operating performance in the emergency department for a patient in whom AA is suspected are CRP (sensitivity: 87.13%; specificity: 68.12%; diagnostic accuracy 76.15%) and the percentage of neutrophils > 85% (sensitivity: 54.46%, specificity: 65.94%, diagnostic accuracy: 61.09%). These results are similar to previous studies, such as Aguirre et al’s, where there is a similarity regarding the relationship of CRP and eosinophilia with the pathology, as described in this article28. Overall, the results provide us with valuable tools in daily clinical practice; however, we believe that there is a greater need for research in this field to achieve uniformity in information nationwide and obtain tools that enable us to address issues such as AA even earlier.
In the study by Padierna et al, only the CRP and the leukocyte count were compared as predictors of severity. Their results for the CRP showed a sensitivity of 98.3% and a specificity of 88.9%, and for the leukocyte count, a sensitivity of 80% and specificity of 61%27. The CRP results obtained are consistent with such research, but there is a significant difference in the leukocyte count since the sensitivity of 78.22% and specificity of 22.46 % were obtained, with a diagnostic accuracy of 46.03%. Thus, the results are uneven in this study, and this leukocyte count should not be one of the mainstays to determine the prognosis in the emergency department due to its low specificity.
The study by Acharya et al evaluated CRP (sensitivity of 75%; specificity of 50%), the leukocyte count (sensitivity of 79%; specificity of 55%), and other paraclinical tests, such as bilirubin, procalcitonin, IL-6, and urinary serotonin, as other diagnostic and prognostic factors of AA29. In this case, the leukocyte count had a higher value than the CRP, a notable difference based on the results obtained and the rest of the literature reviewed. These results could be explained by the multiple limitations of the study and the potential sources of bias due to the blinding of researchers in the literature.
It is important to highlight that according to the study by Prasetya et al, the NLR had high diagnostic accuracy for AA in children, with percentages of sensitivity of 84.6% and specificity of 56.5%, these being higher than those obtained in our study (61.39% and 43.48%, respectively). This finding is probably due to the difference in the age of the study population (18 years as a maximum) and because this is a retrospective study. This limitation should be considered when interpreting results33.
Conclusions
Currently, AA is a challenge for diagnosis and prognosis in the emergency department, both for the general practitioner and the specialist, because there is still no marker to define how advanced the pathology is and its potential complications. However, this study could determine the operating characteristics of the inflammatory reactants as predictors of severity in AA and thus prevent possible complications. It was found that CRP has the highest specificity and sensitivity and is also the most positive OR predictor compared to the rest of the reactants.
It also revealed that a leukocyte count greater than 11,000/mm3 and a percentage of neutrophils > 85% were related to the diagnosis of AA. According to the results obtained in this study, a percentage of neutrophils > 85% increases the possibility of a complication (OR 2.17), while a CRP greater than 15 mg/dL increases the possibility of a complication (OR 14.46). This characteristic could be definitive to find the probabilities of AA complications in any age group.
In short, this study could determine the cut-off points of paraclinical variables widely used to predict and prevent AA complications, such as perforation, optimizing in-hospital management and ultimately impacting final care costs and recovery times for patients.











 text in
text in