Introduction
Iron-deficiency anemia occurs in 2% to 5% of adult men and postmenopausal women in developed countries and is the presenting complaint in 4% to 13% of patients in the European community. The leading cause of anemia in premenopausal women is menstrual bleeding, while in postmenopausal women and adult men, it is of gastrointestinal origin1. According to the World Health Organization (WHO), anemia is a hemoglobin level below 13 g/dL in men and 12 g/dL in non-pregnant women over 15 years of age. It is regarded as an iron deficiency when ferritin levels are less than 15 µg/L; if an inflammatory disease coexists, a level of less than 50 µg/L2 is considered.
Chronic occult blood loss from the gastrointestinal tract is widely accepted as the main cause of iron deficiency anemia. It can be evaluated by conventional endoscopic methods, such as esophagogastroduodenoscopy and colonoscopy. However, in about 30% of patients with iron-deficiency anemia, its cause is not explained after these studies. In 5% of patients with overt gastrointestinal bleeding, no lesions are identified with these endoscopic diagnostic studies, thus requiring an examination of small bowel lesions with diagnostic methods, such as video capsule endoscopy (VCE)3,4 and single- or double-balloon enteroscopy5. These two studies have similar performance and findings (70.5% vs. 69.6%; p = 0.9), if a complete enteroscopy is achieved6,7. The agreement between VCE and enteroscopy can also vary depending on the type of lesion found, with good agreement for inflammatory lesions Ik = 0.71 (95% CI 0.52-0.91) and moderate agreement for angiectasias, Ik = 0.45 (95% CI 0.25-0.65) and tumors, Ik = 0.40 (95% CI 0.12-0.68)8.
VCE is considered the preferred method by patients and clinicians because it is non-invasive. Enteroscopy is more invasive and has more adverse effects, with complications inherent to the procedure or anesthesia9,10. The main complication of VCE is retention in the small bowel, defined as the permanence of the device in the gastrointestinal tract for more than 15 days11. This paper aims to characterize lesions in the small bowel related to the diagnosis of unexplained iron-deficiency anemia.
Different series have assessed the diagnostic performance of VCE in obscure gastrointestinal bleeding, with 57% according to Juliao et al10 and 58% in the series by García del Risco et al12. In the latter, overt obscure bleeding was present in 68% and occult bleeding in 32%12, without discriminating the VCE findings in these patients with anemia without overt bleeding, who are the subject of this study. However, one barrier is that despite being a non-invasive method and having a low rate of adverse events, it represents a high cost. So, this resource is not available in many low- and middle-income countries.
Materials and methods
Study design
This descriptive, observational, retrospective study included all patients over 18 years of age with an indication for VCE due to iron-deficiency anemia between January 2011 and December 2019. Outpatient and inpatient procedures were added. Patients with overt gastrointestinal bleeding were excluded. All patients had negative ileocolonoscopy, esophagogastroduodenoscopy, and positive fecal occult blood test. In addition to demographic variables and VCE findings, we collected information from paraclinical tests, including hemoglobin, iron, and ferritin levels, comorbidities, and drug history, such as nonsteroidal anti-inflammatory drugs (NSAIDs), antiplatelet drugs, or anticoagulants during the study or within 90 days prior.
VCE procedure
Examinations were performed with the VCE Pillcam SB2 and SB3 (Medtronic). The procedure began by administering the capsule after an 8-hour fast13, previously prepared with two sachets of polyethylene glycol diluted in two liters of water14,15. At four hours, the patient was allowed to have a light meal. After eight hours, or the time required for the VCE to achieve a cecal image, the recorder was turned off, and the images were downloaded using Rapid Reader software. Three gastroenterologists with training and experience in interpreting VCE performed the assessment.
The VCE findings were interpreted according to the degree of clinical relevance for the final diagnosis, according to Saurin’s classification proposal: No potential of bleeding (P0) or absence of lesions; low/uncertain risk of bleeding (P1), including red spots, lymphangiectasia, phlebectasias, erosions, xanthomas, nodular lymphoid hyperplasia; and high bleeding potentials (P2), such as angiectasias, tumors, or ulcers16. VCE retention was established as non-expulsion within 15 days of performing the VCE17.
Statistical analysis
Demographic variables are presented as percentages and frequencies; quantitative variables are means with standard deviations (± SD) in normal distribution and continuous variables and median with interquartile range (IQR) for non-normal distribution variables. We grouped the categorical variables into absolute and relative frequencies, measured in percentages for their description. The Chi2 test or Fisher’s exact test, as necessary, was used to compare the distribution of qualitative variables, such as lesion grades according to capsule type and age range. We considered a p-value < 0.05 statistically significant. Analyses were performed using STATA 15.0 software. (Statistic Software. College Station, TX: Stata Corp LP).
Results
Between January 2011 and December 2019, 490 VCEs (PillCamSB2 - SB3) were performed at the institution. We analyzed 155 studies, indicating iron-deficiency anemia of unexplained cause in 153 patients. The mean age was about 60 years. The female sex represented two-thirds of the population under study; 90% of the studies were outpatient. The primary comorbidities of our patients were cardiovascular, high blood pressure, and gastrointestinal, while one in seven subjects had no medical history. Drug history was not documented in all medical records. Still, among those that documented it (n = 117), the most common were antiplatelets (acetylsalicylic acid [ASA] or clopidogrel), followed by oral anticoagulants and heparins. The general characteristics of the patients are shown in Table 1.
Table 1 General characteristics of the sample (N = 155). Comorbidities (N = 126) or drug history (N = 117) were not reported in all records
| Age (years) | |
|
|
|
| Women (%) | 106 (68.4 %) |
| Area | |
|
|
|
| Comorbidities (N = 126) | |
|
|
|
| Drugs (N = 117) | |
|
|
|
NSAID: Nonsteroidal anti-inflammatory drug; SD: Standard deviation; IQR: Interquartile range.
The VCEs used were the Pillcam SB3 type in 70 (45.2%) studies. The unobstructed view was achieved in 153 (98.7%), with a mean small bowel transit time of 233 minutes (SD of 117 minutes). Positive findings were identified in 114 (73.6%) procedures. The most frequent lesions were of a vascular etiology, followed by inflammatory and neoplastic causes. Stenosis was found during VCE transit in six cases (3.8%), with retention in four patients (2.6%).
Potential bleeding lesions, characterized as P2 lesions according to the Saurin classification, were found in 53 (34.2%) VCEs. According to the type of VCE, there were statistically significant differences in the positive findings in the Pillcam SB3 VCE (84.2%) compared to the Pillcam SB2. According to the lesion grade of Saurin classification, the P0 was 32 (37.7%) with Pillcam SB2 and only eleven with SB3 (15.7%) (p 0.0024). P1 lesions were found in 26 (30.6%) with Pillcam SB2 and 33 with SB3 (47.1%) (p 0.0346). In the P2 lesions, there were no statistically significant differences (p 0.4823) in the Pillcam SB2; they were found in 27 (31.8%) VCEs, compared to SB3. Lesions were identified in 26 (37.1%) studies, highlighting a poor view in only two (1.3%) of the Pillcam SB2-type VCEs. No lesions were detected in the latter, but it does not interfere with these findings.
In 63 VCEs (40.6%), flat-looking lesions were identified as angiectasias, lymphangiectasias, and macules. Protruding lesions were found in 27 studies (17.3%); nodules were the most frequent, followed by tumors. Excavated lesions were present in 46 (29.7%). The most frequent type was erosions, followed by ulcers. Of the vascular lesions, the most frequent were angiectasias in 33 studies, followed by ulcers and tumors (Figure 1 and Table 2).
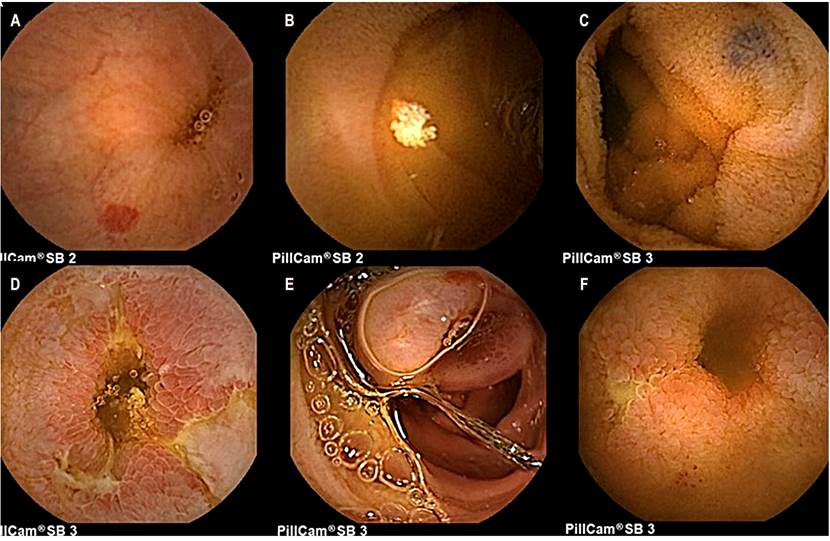
Figure 1 VCE images in patients with unexplained iron-deficiency anemia. A. Angiectasias. B. Lymphangiectasia. C. Phlebectasia. D. Fibrin-covered ulcers. E. Tumor. F. Stenosis. Source: Authors’ images.
Table 2 General findings on VCE in patients with unexplained iron-deficiency anemia (N = 155)
| Capsule type | |
|
|
|
| View | |
|
|
|
| Small bowel transit | |
|
|
|
| Small bowel lesions | |
|
|
|
| Type of lesion | |
|
|
|
| Lumen | |
|
|
|
| Mucous membrane | |
|
|
|
| Flat lesions | |
|
|
|
| Protruding lesions | |
|
|
|
| Excavated lesions | |
|
|
|
| Grade of lesion (Saurin classification) | |
|
|
|
In elderly patients, angiectasias were identified in 26.5% and tumors in 7.2%; ulcers were more frequent in those under 60 years old. P2 lesions with bleeding potential occurred in 42.2% of patients over 60 years of age, with a statistically significant difference (Table 3). Protruding lesions interpreted as tumors were identified in seven (4.5%) VCEs. Of these studies, four patients underwent institutional enteroscopy and biopsy of the lesions, with histopathological findings in two patients: One with moderately differentiated adenocarcinoma and the other with Hodgkin’s lymphoma. One patient had a lesion that corresponded to lymphangiectasia.
Table 3 Positive findings on VCE according to age group
| < 60 years N = 72 n (%) | ≥ 60 N = 83 n (%) | P-value | |
|---|---|---|---|
| Angiectasias | 11 (15.3) | 22 (26.5) | 0.0885 |
| Ulcers | 7 (9.7) | 6 (7.2) | 0.5764 |
| Tumor | 1 (1.4) | 6 (7.2) | 0.1231 |
| Lesion grade | |||
| 0 | 21 (29.2) | 22 (26.5) | 0.7121 |
| 1 | 33 (45.8) | 26 (31.3) | 0.0635 |
| 2 | 18 (25.0) | 35 (42.2) | 0.0246 |
The hemoglobin value within three months before or after the VCE was reported in 64 medical records, with an average of 9 g/dL. Eight patients had normal hemoglobin, according to the WHO definition. Just over half of these patients (33) presented with moderate anemia, defined by a hemoglobin range between 7.0 and 9.9 g/dL in 33 (21.3%), while six had severe anemia (less than 7 g/dL). In these patients with moderate to severe anemia, P1 and P2 lesions, according to the Saurin classification, were found in 29 (51.7%) VCEs. Ferritin level was documented in 20 patients, with a mean value of 30.2 ng/mL (7.9-89.0), and the iron level in 21 patients, with a mean of 22 µg/dL (15.7-27.0 µg/dL).
Discussion
Obscure gastrointestinal bleeding is classified as overt bleeding if there is evidence of bleeding (hematemesis, melena, or hematochezia) or occult bleeding, defined by iron-deficiency anemia or persistently positive fecal occult blood. Many of these patients pose a diagnostic challenge and require other assessment methods, such as VCE, to identify lesions in the small bowel, which are not within the scope of upper endoscopy or colonoscopy. Unexplained iron-deficiency anemia is a frequent reason for referral to gastroenterology to identify the lesion responsible for bleeding because its recurrence has high morbidity, requires a transfusion, and can lead to mortality.
Due to the complete examination of the entire mucosa of the small bowel in the VCE, the diagnostic assessment has been extended to patients with occult gastrointestinal bleeding, which has allowed identifying the cause in many patients with unexplained iron-deficiency anemia18. The diagnostic yield in various studies has proven superior to other methods in identifying the source of bleeding. In a meta-analysis of 14 prospective studies in 396 patients with occult gastrointestinal bleeding, VCE was found to have a better diagnostic yield than enteroscopy (56% vs. 28%, p < 0.00001) and other radiological studies of the small bowel, such as barium x-ray (67% vs. 8%; p < 0.00001).
Compared to the other tests, the number needed to diagnose (NND) in VCE was three (95% CI 2-4). The most significant use was noted in vascular lesions, 36% in VCE compared to 20% in enteroscopy19. In this study, the most frequent lesions identified were of a vascular etiology in 44 (28.4%) VCEs, specifically in patients with unexplained iron-deficiency anemia without overt bleeding.
Some series have evaluated the diagnostic yield of VCE in overt and occult obscure gastrointestinal bleeding. Chronic anemia was identified in 41% of the patients, as in the series of 100 patients reported by Mosquera et al in a tertiary referral center20, without determining the diagnostic yield in patients with unexplained iron-deficiency anemia, which is the subject matter of this study.
A recent retrospective study on 118 patients evaluated the impact of VCE on iron-deficiency anemia; it was diagnosed in 49%. Small bowel lesions were more frequent in those over 60 years of age (60%) compared to 34%, attributable to the higher frequency of angiectasias and inflammatory causes in those under 60, as described in this study, with evidence of statistically significant P2 lesions in those over 6021. Some studies have described a higher frequency of iron-deficiency anemia in patients older than 50 years (OR 1.6; p = 0.002; 95% CI 1.2-2.2), more comorbidities, and transfusion requirements22.
Angiectasias are among the most common causes of iron deficiency anemia in the elderly with comorbidities, such as kidney disease or chronic liver disease, followed by NSAID-induced inflammation23. The higher performance of VCE has been found in patients older than 75 years compared to a younger population (51.47% vs. 42.76%; p 0.002)24. Another study, which assessed the predictive factors of positive VCE findings in patients with iron-deficiency anemia, found an association between male sex (OR 3.93; 95% CI 1.57-9.86), age (OR 1.03; 95% CI 1.0-1.06), and hemoglobin levels less than 9 g/dL (OR 0.73; 95% CI 0.57-0.94)25.
In their study of 109 patients with unexplained iron-deficiency anemia who underwent VCE, Contaldo et al documented small bowel lesions in 73.4% of patients, with multiple lesions in 17.5%. The consumption of NSAIDs was associated with lesions (OR 1.13; 95% CI 1.02-1.31; p 0.049). The intake of anticoagulants was not statistically significant (OR 3.38; 95% CI 0.73-15.7; p 0.10)26.
This study showed positive VCE findings in 73.5% of cases where lesions were documented, with the potential for anemia in 34.2%. More lesions were found with the type of VCE Pillcam SB3 (84.3% of the studies), with statistically significant differences in identifying P1 and P0 lesions with no potential for bleeding. There were no differences between the type of VCE in P2 lesions or with a potential for anemia.
In the literature, VCE has a diagnostic yield of 38-83% in patients with small bowel lesions, with a positive predictive value of 94-97% and a negative predictive value of 83-100% in assessing gastrointestinal bleeding. Its limitations are low specificity and false negatives in 10-36% of cases5. The main complication of VCE is retention in the small bowel11. Our study showed stenosis during VCE transit in six patients (3.8%), with retention in four (2.6%). The occurrence was somewhat higher than in other studies, which state that it is less than 2%17. In a systematic review of 227 studies (a total of 22,840 procedures) by Liao et al, the detection rate of small bowel lesions was reported as 59.4% (p < 0.0001; 95% CI 56.5-62.2%), lower than in this study. The most frequent lesions were angiectasias in 50%; complications such as retention occurred in 1.4%27.
In a retrospective study conducted by Riccioni et al28 to evaluate the usefulness of VCE in 138 patients with unexplained iron-deficiency anemia, VCE identified at least one causal lesion in two out of three patients evaluated. The main findings were angiectasias, followed by jejunal or ileal microulcerations, tumors, erosive gastritis, and Crohn’s disease. At the end of the follow-up period, improvement in anemia after intervention and treatment (medical, endoscopic, or surgical) was documented, with complete resolution of iron-deficiency anemia in 96% of patients. In our study, VCE identified positive findings in three out of four studies and showed lesions causing anemia in 34%. Given that these patients were admitted only for the procedure, we could not review their complete medical records, preventing the possibility of assessing the subsequent follow-up of the interventions and treatments performed.
The limitations of our study are retrospective, so it was not possible to tell the patient to stop treatment with NSAIDs prior to the VCE.
Conclusions
With the results obtained in this work, we can conclude that VCE is a valuable tool in studying patients with unexplained iron-deficiency anemia, in whom upper and lower digestive tract lesions have been ruled out. Positive findings were identified in the midgut that explain the anemia in 34% of cases. The most frequent significant P2 lesions were vascular. These findings allow interventions and appropriate direct treatment.











 texto en
texto en 



