Introduction
Pancreatitis has been defined on multiple occasions over the years. However, in 2013, it was defined as “an acute process of the pancreas, triggered by the inappropriate activation of pancreatic enzymes, with tissue injury, and local inflammatory response with variable involvement of other tissues or distant organ systems.”1 Data in the United States report more than 300,000 admissions per year for this pathology. Mortality does not exceed 1% in mild admissions, and this figure can increase to 30% in severe cases. Mortality in these patients is, to a greater extent, a consequence of multi-organ failure or complications related to the difficult control of the local inflammatory process2.
One of the secondary complications to the inflammatory process of the pancreas to be highlighted is infected pancreatic necrosis, which historically has a mortality that can reach 70% with surgical management (mainly open). However, since the advent of minimally invasive approaches (fine-needle aspiration, percutaneous, endoscopic, or laparoscopic drainage), this figure has decreased to 30%3.
In 2013, a study compared open with laparoscopic management for debridement of infected pancreatic necrosis. A reduction from 63% to 41% in the rate of postoperative complications with laparoscopic management was shown. Postoperative organ failure also reduced their rates from 54% to 22%. The postoperative intensive care unit (ICU) requirement decreased from 54% to 29%, while the incidence of post-operative fistulas was lower than in open management, decreasing from 36% to 10%4. This same study considered an adequate time for surgical management by laparoscopy. An average of 30 days was evaluated with better results in terms of mortality and morbidity after this time4.
What has been described above reflects the high morbimortality rates of this pathology. This is why, in recent years, strategies for the prediction of pancreatitis complications, such as the measurement of serum procalcitonin, have been proposed. Multiple studies have shown its usefulness in assessing patients with suspected local complications like infected pancreatic necrosis, and it could also have a predictive value to consider antibiotic onset and its prognosis5-8.
It has been recently proposed that the safest management with lower rates of postoperative complications should be laparoscopic5. However, there are no epidemiological data in Colombia on the incidence of complications after pancreatitis or the management indicated for infected pancreatic necrosis. However, there are data reported in the literature where the low incidence of complications is exposed, which in some case series reaches up to 8%1,9. In recent years, thanks to greater surgeon training, the laparoscopic management of these pathologies has increased in our institution. This study will describe the experience in the surgical management of infected pancreatic necrosis at the Hospital Universitario Mayor Méderi in Bogotá, Colombia.
Materials and methods
A descriptive observational case series study was conducted. An initial medical history review of patients diagnosed with pancreatitis was performed. Then, in a second step, those patients who underwent surgical drainage of infected pancreatic necrosis between 2014 and 2021 were analyzed. Patients with pancreatitis of a different origin to the biliary one were excluded. Sample size calculation was not performed. All patients meeting the inclusion criteria were considered. Demographic, clinical, surgical, imaging, and paraclinical variables were collected. A descriptive analysis was carried out: qualitative variables were presented in absolute and relative frequencies, and quantitative variables were formulated with dispersion and central tendency measures according to normality.
Diagnosis of complication
Those patients who had torpid progression after the first 96 hours of comprehensive medical management were taken as suspects for a possible local complication of pancreatitis. Then, by performing imaging studies (abdomen tomography and abdominal magnetic resonance imaging), local complications were confirmed. Additionally, those patients who presented signs of systemic inflammatory response, sepsis, and radiological evidence of gas within the collection were considered infected. The diagnosis of infected pancreatic necrosis was then configured.
Results
A total of 1020 medical records of patients diagnosed with acute pancreatitis were analyzed between 2014 and 2021. 33 patients who presented infected pancreatic necrosis as a major complication were identified and taken to surgical drainage by the institution’s General Surgery service. Three patients were excluded, two of them due to traumatic pancreatitis and one because of secondary pancreatitis to hypertriglyceridemia.
A period prevalence of pancreatic necrosis of 2.9% was identified in relation to all pancreatitis analyzed. As for the population with infected pancreatic necrosis, most of them are male (70%; n = 21) with an average age of 56 years (Table 1). 93% of patients were studied preoperatively using an abdominal computed tomography with contrast. Antibiotic management prior to any intervention in all patients was initiated using multiple antibiotic therapies in 53% of them (Table 2). It is important to emphasize that in the ICU, antifungals were initiated prophylactically in 30% of patients, following institutional protocols adjusted to international scales of risk prediction for fungal colonization (isolating in 28% of patients). The entire sample that was subjected to surgical drainage was cultured from the collection. More than one germ was isolated in 33% of the evaluated samples, and in 26% of the cases, it was negative (Table 3).
Table 1 Comorbidities
| Comorbidities | N | % |
|---|---|---|
| Denies comorbidities | 13 | 34.2 |
| Diabetes mellitus type 2 | 4 | 10.5 |
| Chronic obstructive pulmonary disease | 3 | 10.5 |
| Chronic kidney disease | 0 | 0 |
| Arterial hypertension | 7 | 18.4 |
| Coronary disease | 1 | 2.6 |
| Immunosuppression | 1 | 2.6 |
| Others (peptic acid disease, hypothyroidism) | 8 | 21.05 |
| More than two comorbidities | 7 | 23.3 |
| Only one comorbidity | 10 | 33.3 |
Table 2 Antibiotic therapy
| Antibiotic | N | % |
|---|---|---|
| Meropenem | 27 | 90 |
| Ampicillin/sulbactam | 3 | 10 |
| Vancomycin | 7 | 23.3 |
| Caspofungin with fluconazole | 9 | 30 |
| Metronidazole | 1 | 3.3 |
| Monotherapy | 14 | 46.6 |
| Multiple therapies | 16 | 53.3 |
Table 3 Isolated microorganisms
| Microorganism | N | % |
|---|---|---|
| E. coli | 6 | 20 |
| P. aeruginosa | 2 | 6.6 |
| K. pneumoniae | 6 | 20 |
| K. oxytoca | 2 | 6.6 |
| E. faecalis | 2 | 6.6 |
| E. faecium | 4 | 13.3 |
| E. casseliflavus | 1 | 3.3 |
| E. gallinarum | 1 | 3.3 |
| A. baumannii | 2 | 6.6 |
| S. anginosus | 1 | 3.3 |
| S. epidermidis | 1 | 3.3 |
| S. haemolyticus | 1 | 3.3 |
| C. freundii | 1 | 3.3 |
| K. ascorbata | 1 | 3.3 |
| Candida albicans | 4 | 13.3 |
| Candida glabrata | 3 | 10 |
| Candida tropicalis | 1 | 3 |
| Polibacterial | 10 | 33.3 |
| Bacterial with fungal | 6 | 20 |
| Monobacterial | 6 | 20 |
| Negative | 8 | 26 |
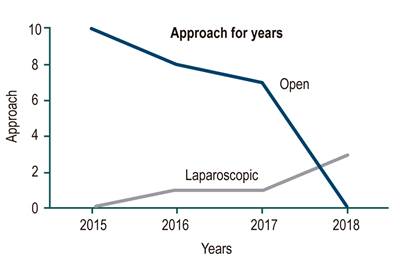
In terms of invasive interventions for managing complications, it was found that, in all cases, patients were assessed by interventional radiology to perform interventions prior to surgical management. The open surgical approach was evidenced in 83% of cases, whereas 16% of cases were managed laparoscopically (Figure 1).
Regarding postoperative complications, 73% of patients (n = 22) did not present any. Out of 27% of patients with complications, the most frequent condition was the pancreatic fistula. Postoperative outcomes such as reinterventions, total hospital stay, postoperative hospital stay in ICU, and mortality in those patients undergoing surgical management by laparoscopy are described in Table 4.
Table 4 Postoperative variables
| Approach | Mortality (n) | Hospital stay in an average of days (n) | Stay in POP intensive care unit in a maximum of days | Reinterventions (n) | Procalcitonin > 1,8 |
|---|---|---|---|---|---|
| Open | 25 (12) | 2-132 | 0-65* | 25 (19) | 25 (8) |
| Laparoscopic | 5 (0) | 9-40 | 2-9 | 5 (0) | 5 (2) |
POP: Postoperative. *Day 0 for mortality.
As part of an additional analysis, the use of procalcitonin was evaluated. We were able to observe that for values < 1.8 ng/dL, mortality was 8.33 (n = 1), compared with values > 1.8 ng/dL where it was 60% (n = 6). Its behavior is described in Table 5. Additionally, as we do not have statistical data on this pathology in Latin America, we evaluated the institution’s prevalence of infected pancreatic necrosis. In the 2014-2021 period, there were 1020 cases of pancreatitis (this data could be biased due to the institution’s ICD-10 diagnostic records). Out of these, 30 patients presented infected pancreatic necrosis as a major complication of pancreatitis, equivalent to 2.9% of period prevalence. This is not far from what is described in the literature (1.2%).
Discussion
The management of acute pancreatitis complications has steadily evolved for about 20 years. Initially, open management was perhaps the only approach. It showed morbidity rates ranging from 43% to 89% and mortality rates as high as 39% in some case series. However, management through minimally invasive techniques has increased recently and showed better results in terms of morbidity and mortality compared to open management, such as in reinterventions (34% vs. 12%), pancreatic fistula (10% vs. 7%), mortality (18% vs. 27%) and hospital stay (40d vs. 49d), respectively, as reported in the literature10-16.
Additionally, the “step-by-step” management of infected pancreatic necrosis has been proposed. It establishes compliance with certain interventions in order to defer a surgical procedure that could add morbidity and even mortality to the patient3. In some case series, minimally invasive “step-by-step” management has demonstrated efficacy in about 40% of patients, reducing the need for surgical management3. 100% of our population was referred to the interventional radiology or gastroenterology service to assess the relevance of fine-needle aspiration, percutaneous drainage, or endoscopic drainage of the pancreatic lesion (following the “step-by-step” management of the infected pancreatic necrosis)3.
In 20% of cases, patients underwent percutaneous drainage of the lesion first, and 3% underwent fine-needle aspiration. The rest of our population required surgical management due to technical difficulties of the percutaneous/endoscopic procedure. We can evidence that percutaneous management was effective in 23% (n = 7) of our patients and prevented an eventual surgical procedure. This is not far from what was reported in the literature (35%-40%)3.
However, in surgical terms, the laparoscopic approach has had significant advances in recent years mainly because of greater surgeon training (Figure 1). This results in better use of the approach. The evidence in the world literature reports better results, such as postoperative ICU stay, mortality, reinterventions, and complications such as pancreatic and enterocutaneous fistula. In our study, laparoscopic management presented 0% mortality with a mean follow-up of 1 year. Similar results are reported in the literature, which are reported for minimally invasive approaches of 9%1,3,9,10 compared to open management, where we observed a rate of 48% (results comparable to those documented in the literature of 45% -50%)4,9,11.
In terms of postoperative organ failure, laparoscopic management in the population decreased by about 40% from day 1 to day 2 and 20% from day 2 to day 3. These results are not evidenced in any study evaluated in the bibliography. However, in a series of cases, postoperative de novo organ failure was evaluated and decreased by about 25% in patients with minimally invasive approaches3.
Additionally, we observed that procalcitonin (PCT) was used as an infection marker in most of our patients (73%) prior to imaging studies. We established a 1.8 ng/mL cutoff point (taken from previous studies)5,6,8,12 and, given recent advances with PCT as a useful biomarker for antibiotic initiation in pancreatitis, we wanted to observe its behavior compared to the computed tomography severity index (CTSI) and mortality. PCT > 1.8 ng/mL was found to be related to a higher CTSI. In terms of mortality, we found that a PCT < 1.8 ng/mL was associated with lower mortality rates (out of 12 patients with PCT < 1.8 ng/mL, 11 had no mortality). This could reflect a possible relationship between procalcitonin elevation and pancreatic inflammatory status.
In microbiological terms, patients had a polymicrobial behavior with a predisposition to enterobacteriae colonization, which is related to what is reported in the literature7,13,14. Regarding antibiotics, there is a tendency to use carbapenems (more precisely meropenem) as described in international guides and recent studies. These studies indicate that their use, or that of ertapenem, has favorable results to control these infections5,7,8,14-41.
Given the above, as observed in our results, and considering what has been reported in the world literature, the minimally invasive laparoscopic approach shows promising results as it reduces, in considerable terms, the morbidity and mortality of our patients and hospital costs due to a decrease in general hospital stay and ICU. However, these results depend on multiple additional factors, such as the patient’s age, comorbidities, and the surgeon’s training, which is not assessable in the present study due to its observational nature.
The observed behavior of procalcitonin is promising. Recently, studies in the UK, such as PROCAP, sought to establish a relationship between PCT and the initiation of antibiotic therapy in pancreatitis7,17-25,42-45. Although no study adequately reveals a predictive capacity of procalcitonin in this pathology5,7,8,16,26-41, we can evidence a trend of this marker as a predictor of mortality in our study. However, more prospective studies are needed to confirm this hypothesis.
Limitations of the study
The observational and retrospective nature prevents the hypotheses formulation with statistical power. However, based on the observational behavior of the results, it invites to generate hypotheses to be used in prospective studies that confirm what has been evaluated in this series of cases.
Conclusions
Currently, infected pancreatic necrosis is still a difficult pathology to manage surgically and a challenge for the surgeon. Stepwise and minimally invasive management should be of choice, always trying to avoid a surgical procedure that, if necessary, should be addressed laparoscopically since it presents better results in terms of mortality, morbidity, and general hospital and ICU stay. Procalcitonin could be a useful biomarker for predicting complications or mortality in these patients. However, more prospective studies are needed.











 text in
text in