Introduction
Esophageal intramural pseudodiverticulosis (EIPD) is an extremely rare disease, first described in 1960 by Mendl et al. Since then, around 240 published cases have been collected worldwide until 20141. EIPD primarily affects men in their 60s2.
Its etiology and pathogenesis are not yet fully known. The main hypothesis to explain EIPD results from a hypertrophy of the submucosal glands with cystic dilation of the excretory ducts. During the illness course, inflammation of the submucosal glands can cause fibrosis of the esophageal wall, with consecutive stricture of the lumen. Esophageal stenosis leads to dietary impacts, malnutrition, and dysphagia, which is present in up to 80% of patients2-5.
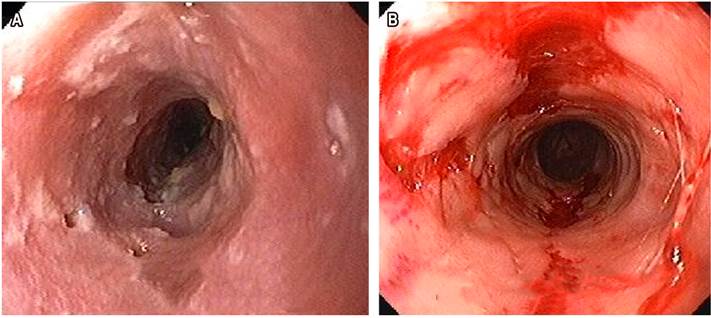
Diagnosis is established by upper gastrointestinal endoscopy (UGE) and a radiological examination of the esophagus with barium contrast (esophagogram). Histological examination is essential to differentiate between benign and malignant stenosis. During UGE, numerous ostia can be visualized, measuring between 2 and 4 mm with whitish collections on the outside of the esophageal wall and stenosis. The esophagogram shows an esophageal stricture and small areas of contrast accumulation, corresponding to the pseudodiverticula2.
Conventional treatment is based on relieving symptoms. Dysphagia is treated by endoscopic dilation with Savary-Gilliard tubes. When there is gastroesophageal reflux and moniliasis, specific medications are used for their treatment. Most EIPD cases have a good evolution with this therapeutic scheme3. Esophagectomy was rarely necessary6.
Materials, methods, and results
Case 1
A 73-year-old female, native and resident of Barretos, SP, Brazil. A smoker who uses 60 packs per year. She suffered from progressive intermittent dysphagia for 17 years. During this period, she made a soft diet. She even had food impact treated by endoscopy. She sought medical attention when she had dysphagia for liquids, but the EIPD diagnosis took 1 year. During this period, she lost 35 kg and underwent a surgical gastrostomy. After diagnosis, she consulted for dilation with Savary-Gilliard tubes. The treatment was initiated with a 5.0 mm tube. After the second session, the 11 mm diameter was reached. At this point, she started eating solids, and the gastrostomy tube was performed. The treatment with dilatations was extended for 6 months, for a total of 5 sessions. She also received fluconazole to treat esophageal moniliasis, present in all performed endoscopies. Omeprazole was also administered for esophagitis due to gastroesophageal reflux disease (GERD), aggravated by a hiatal hernia. The patient had an excellent response to treatment and has remained asymptomatic for 3 years (Table 1 and Figure 1).
Table 1 Clinical picture, endoscopic findings, and therapeutic response of reported cases
| Personal data | Case 1 | Case 2 |
|---|---|---|
| Sex | Female | Male |
| Dysphagia time (years) | Yes (17 years) | Yes (10 years) |
| Impact | Yes | Yes |
| GERD esophagitis | Yes | Yes |
| Moniliasis | Yes | Yes |
| Smoker | Yes | Yes |
| Uses alcoholic beverages | No | Yes |
| Weight loss (kilos) | 35 | No |
| Weight gain after treatment | Yes | Yes |
| Esophageal stenosis | Yes | Yes |
| Treatment with esophageal dilation | Yes (up to 11 mm) | Yes (up to 12.8 mm) |
| Dysphagia return time | Asymptomatic 3 years ago | 6 months |
GERD: esophagitis due to gastroesophageal reflux disease. Source: Table prepared by the author
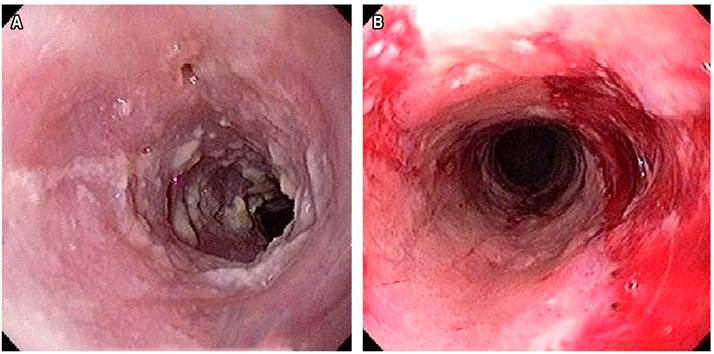
Figure 1 Endoscopic images of patient’s EIDP from Case 1. A. Diagnostic image of EIPD for moniliasis. B. Image after endoscopic dilation. Source: personal file.
Case 2
VJR is a 55 year old male, born in Valparaiso, SP, resident of Tucuruí, PA, Brazil. He suffered from dysphagia for 10 years. He ate only soft and liquid foods in this period. He had food impact 4 times and required endoscopic extraction. When he sought medical help, he drank fluids for 3 months. He reported symptoms such as dysphagia, pyrosis, and moderate gastroesophageal reflux in chronic use of omeprazole. The patient claims to consume alcoholic beverages at least once a month and is a smoker who uses 32 packs per year. EIDP was diagnosed 3 years ago through an upper gastrointestinal endoscopy when esophageal candidiasis was also found.
Initially, 3 sessions were held at 1-week intervals. Dilations began with 7.0 mm tubes. At the end of 3 weeks, they reached 12.8 mm with a complete reversal of dysphagia. Due to the distance between the state of Pará, where the patient resides, and the city of São José do Rio Preto, where he undergoes treatment, dilation sessions have been held every 6 months for the last 3 years. The patient reports remaining asymptomatic for 5 months until the dilation endoscopy presented dysphagia to solids in the last month. He also presents with moniliasis whenever digestive endoscopy is performed. From the beginning of the treatment, the patient gained 11 kilos (Table 1 and Figure 2).
Discussion
Dysphagia was the main symptom in the two cases reported in this study. It was also the main reason the individuals sought medical help. Similarly, more than 72% of patients in the following studies had dysphagia as their main symptom1-3,5-9.
Patients are over 70 years old in both reported cases, very similar to the data provided in most cases in the medical literature1-3,6,7,9-14. Except for patients with human immunodeficiency virus (HIV), who presented the condition at age 35 without evidence of moniliasis8, and at age 45 (Table 2)5.
Table 2 Summary of the main findings of the case reports in the medical literature
| Datos personales | Número de casos | Porcentaje (%) |
|---|---|---|
| Years (average) | 62 years | - |
| Woman | 03 | 27.27 |
| Man | 08 | 72.72 |
| Dysphagia | 08 | 72.72 |
| Impact | 03 | 27.27 |
| GERD esophagitis | 07 | 63.63 |
| Moniliasis | 07 | 63.63 |
| HIV | 02 | 18.18 |
| Smokes cigarettes | 03 | 27.27 |
| Uses alcoholic beverages | 05 | 45.45 |
| Esophageal stenosis | 05 | 45.45 |
| Treatment with esophageal dilation | 07 | 63.63 |
| No improvement after dilation | 01 | 09.09 |
| Dysphagia returned | 00 | 00 |
GERD: gastroesophageal reflux esophagitis; HIV: human immunodeficiency virus. Source: Table prepared by the author.
In the total of the summarized studies in Table 2, a higher incidence of EIPD was demonstrated in men. However, in this report, one case was reported in a man and the other in a woman1,3,5,7-10,13.
Reflux esophagitis and fungal infection may accompany EIPD. In this study, both patients had GERD esophagitis and C. albicans infection. The authors2,6-10,12 reported cases of esophagitis due to GERD1-3,8,9,12,13, where a candid infection was found in the esophageal biopsy (Table 2).
Both patients in this study were treated with endoscopic esophageal dilation, medicines for esophagitis, and GERD moniliasis. Seven studies reported treatment with esophageal dilation and medication for existing pathologies in the literature1-3,5-7,9.
Case studies8,10,12,13 performed conservative treatment only with medication for existing pathologies. Only one of these cases10 showed no improvement in pseudodiverticula during the follow-up period (Table 2).
In this study’s patients, improvement in dysphagia was felt after the first endoscopic dilation session. However, in case 2, there was a recurrence of dysphagia to solids 6 months after the last dilation session. This evolution is explained by the fact that this person lives 2200 km away from the healthcare facility where the treatment is performed, so he cannot carry out all consecutive dilations until a satisfactory esophageal diameter is established. The patient in case 1 received 5 consecutive sessions over 6 months and remains asymptomatic 3 years after the last endoscopic dilation session (Table 2).











 text in
text in