Introduction
Although echinococcosis has a long history dating back to ancient times, it is still a relevant zoonosis nowadays. It has a considerable socioeconomic impact and affects humans worldwide1. This is a disease caused by parasites, specifically the cestodes of the genus Echinococcus2. Two of the most important forms (which have medical and public health significance) are cystic echinococcosis (hydatidosis), caused by infection by E. granulosus, and alveolar echinococcosis, caused by E. multilocularis2.
Cystic echinococcosis has a worldwide distribution. There are endemic foci in all inhabited continents. The highest prevalence of this disease has been found in temperate zones: Mediterranean countries, southern and central Russia, Central Asia and China, and some regions of Australia and America (especially South America). Some risk factors for getting this disease include low socioeconomic status, scarce health education, living in rural areas, and the relationship with dogs in contact with livestock or animal offal3. Although it does not have high mortality (2.2%), it does have high morbidity and an economic impact of billions of dollars3.
E. granulosus requires two mammalian hosts to complete its life cycle: a definitive host (carnivore, especially the dog), where the adult phase is developed, and an intermediate host (sheep, goats, pigs, cattle, among others), where the larval phase or hydatid cyst is spread. Infection in man occurs after parasite eggs are ingested by accident. The eggs reach the small intestine, where their cover is dissolved. Embryos that cross the intestinal mucosa are released and pass into the venous circulation to reach the different organs. They are often in the liver (67%-89%), followed by the lungs (10%-15%). They can also reach other organs such as the kidney, brain, heart, bones, muscle, among others, although these locations do not exceed 10% of the detected cases (Figure 1)4-6.
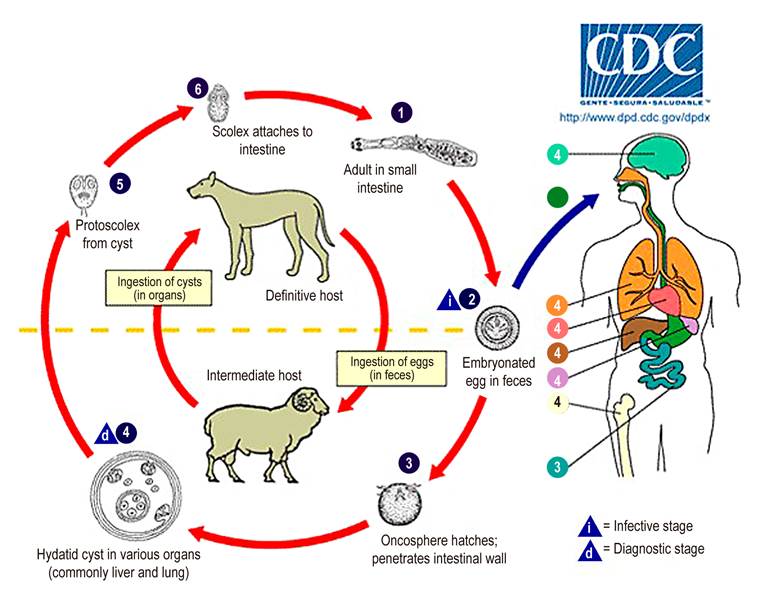
Figure 1 The life cycle of hydatidosis. Source: Courtesy of Centers for Disease Control and Prevention Image Library.
The incubation time in man is several years and can be greater than 40 years. The disease symptoms include cyst expansion, pressure on adjacent structures, infection, rupture, and dissemination of cystic content in neighboring body cavities. When they rupture, spontaneously or secondarily to trauma or surgery, they can cause a seeding that will form multiple cysts (multiple secondary hydatidosis 20%-40%), secondary bacterial infections, anaphylactic reactions, among others4,5.
Presentation of the case
A 21-year-old male patient from a rural area. He reaches the emergency department reporting a 2-year picture of diffuse abdominal pain described as dull, ill-defined, and predominant in the left hypochondrium. The pain is occasionally associated with febrile episodes and nausea, which sometimes reaches emesis of dietary and biliary characteristics. The patient refers to periods of partial remission of the symptoms.
An important event in his history, which is related to the length of time symptoms are present, is a 14-month appendectomy prior to admission with subsequent drainage of the abdominal abscess. It required management by laparotomy.
When admitted to the emergency room, he was hemodynamically stable. On abdominal physical examination, pain on deep palpation in the left epigastrium and hypochondrium was found, with a mass sensation during palpation at this level. Paraclinicals of mild hyperbilirubinemia are taken at the expense of direct, mild leukocytosis and positive C-reactive protein (CRP), hypoalbuminemia, hydroelectrolyte disorder, given by hypopotassemia and hypochloremia, and normal tumor markers (Table 1).
Table 1 Admission laboratory tests
| Paraclinical | Report |
|---|---|
| Complete blood count | Leukocytes 14,4; neutrophils 73.4%; lymphocytes 12.5 %; hemoglobin 13.3; hematocrit 42,6; platelets 290 |
| Hepatic profile | Direct bilirubin 0.57; total bilirubin 1.03; indirect bilirubin 0.46; GOT 16; TGP 16.6; alkaline phosphatase 93 |
| Electrolytes | Ionized calcium 1,1; sodium 141,6; potassium 2,95; chlorine 97,1 |
| Renal function | Ureic nitrogen 7,4; creatinine 0.62 |
| Nutritional Profile | Total proteins 7; albumin 2,7 |
| Tumor Markers | CA 19-9:3 (negative); alpha-fetoprotein 0.5 (negative); carcinoembryonic antigen 0.5 (negative) |
| Others | PCR 28,3 |
A simple and contrasted abdominal and pelvic tomography was performed. Mild hepatosplenomegaly, simple diffuse-distribution intrahepatic and splenic cysts, mesenteric cysts (also in diffuse form), and dilation of intestinal loops with significant distension of the duodenum (Figure 2) were documented. The results were evaluated by the General Surgery surgical board. Due to findings in imaging studies, it was considered that with unclear etiology, residual collections of previous surgical procedures should be discarded. Exploratory laparotomy should be taken, with cysts resection performed and a pathological study to define the etiology and final behavior.
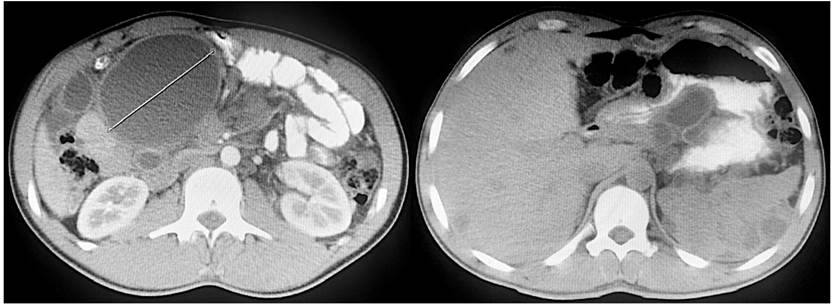
Figure 2 Simple and contrasted abdominal and pelvic tomography. Axial section showing numerous rounded lesions of liquid content, encapsulated and distributed at the root of the mesentery, liver, spleen, and peritoneum.
During the surgical procedure, peritoneal fluid of a moderate amount is appreciated. Multiple peritoneal lesions of cystic appearance: 2 to 3 cm, those of smaller size, and up to 7 cm, the largest. The liquid is located at the root of the mesentery, and it displaces the ascending colon and duodenum, which explains the alimentary emesis episodes (Figure 3).
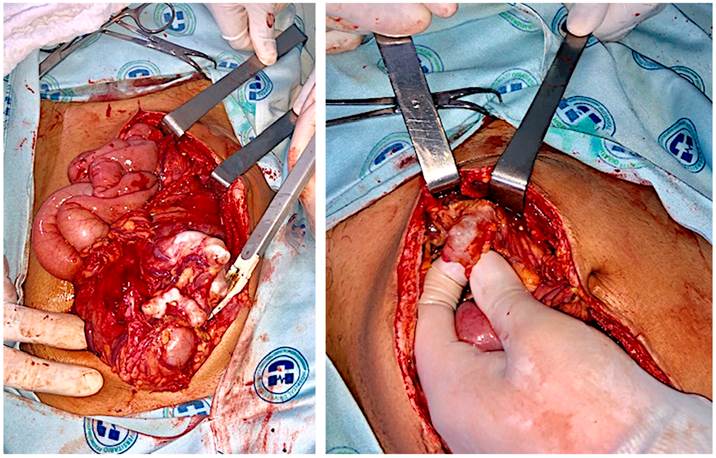
Figure 3 Intraoperative findings. Multiple cystic-like lesions in the peritoneum and root of the mesentery.
FOLLOW-UP AND RESULTS
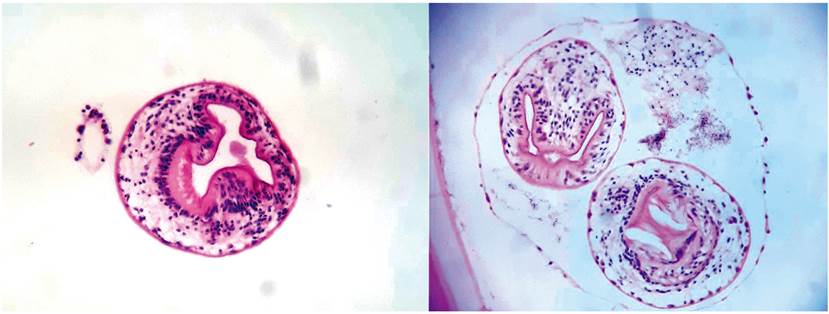
The pathology report of these lesions corresponded to hydatid cystic lesions (echinococcosis), with macroscopic documentation (Figure 4 ) and microscopy study by H&E stain, where numerous scolex are seen inside the cystic cavity (Figure 5 ). The patient presented good clinical evolution after surgery. In-hospital treatment with albendazole 400 mg every 12 hours is initiated for 3-month cycles until 3 cycles are completed with laboratory controls using blood, tomographic and clinical counts every 3 months. The patient is in periodic check-ups with good clinical evolution.
Discussion
The diagnosis of E. Granulosus infection is based primarily on clinical findings, serology, and imaging techniques. At least one of the following clinical diagnostic criteria must be met: anaphylactic reaction due to cyst rupture; symptomatic cystic mass, diagnosed by imaging techniques; incidentally diagnosed cyst by imaging techniques in an asymptomatic patient. The established diagnosis is determined by the characteristic lesion diagnosed by imaging techniques, a positive serology, microscopic examination of the fluid or consistent histological sample, and macroscopically compatible surgical findings3.
In the presented clinical case, what was previously described, is verified. The patient met the second clinical judgment, and the diagnosis was verified through images, surgical findings, and macro and microscopic studies. It was considered that the peritoneal dissemination was due to the reoperation of the appendectomy complication (abscess), which ruptured one of the cysts with the manifest consequence in this clinical case.
There are different imaging techniques for the diagnosis. The abdominal ultrasound is the chosen one in abdominal cystic lesions3, using the World Health Organization and International Working Group (WHO/IWG) classification7. This classification evaluates the activity of hydatid cystic lesions according to the activity and number of loculi. In this way, the response to chemotherapeutic treatment can be assessed to compare different types of management and evaluate their response8. The first clinical group corresponds to the types of cysts EC 1 and 2. These cysts indicate that they are active for their fertility, with viable protoskolex. The second group is EC type 3, which are cystic lesions in a transitional stage where the host’s response to treatment has compromised the cyst integrity. The third clinical group comprises CE types 4 and 5, inactive cysts that normally lose their fertility and are the final degenerative status8. Computed tomography and magnetic resonance imaging are techniques of choice in subdiaphragmatic and multiple lesions, in the presence of complicated cysts with fistulas or abscesses, extra-abdominal localization cysts, and as a form of presurgical assessment3,9.
Currently, there is no unification of criteria regarding the best treatment of cystic echinococcosis, not even in relation to the need to treat or not the infection. The treatment is based on three fundamental pillars:
The use of antiparasitics is mandatory in all patients.
Procedures for interventional purposes should be preferred over palliative surgery whenever possible.
Radical surgery is the first option in all susceptible cases to total resection of lesions. This should always be based on the clinical condition and characteristics of the cysts3,7.
Different techniques for the curative treatment of hydatid cysts have been described: percutaneous needle aspiration, hypertonic saline injection, content reaspiration, resection of the protruding dome with aspiration-exeresis of its content, cystoperichistectomy and hepatic resection10. In general, surgeons from non-endemic areas prefer radical techniques, while those from endemic areas use more conservative techniques10. In the case of symptomatic patients or with complicated hydatid cysts (abscess, abdominal cavity rupture, opening to the bile duct, thoracoabdominal transit), the treatment of choice should be surgery, either conventional or laparoscopic. Preoperative chemoprophylaxis with 10 mg/kg/day of albendazole is suggested for at least 15 days. Albendazole can still be used in all cases for 3 cycles in the postoperative period11,12.
The mean postoperative mortality is 2.2%, approximately 6.5% of recurrent cases after an intervention, leading to prolonged recovery periods2. In our case, the diagnosis was made during the intraoperative period. Radical resection of most cysts was carried out, given the complexity of this pathology, due to its multiple dissemination at the level of organs and the peritoneal cavity.
Regardless of the performed treatment, the patients’ follow-up with this pathology is especially important. Revisions are carried out during the first 2 years on a semi-annual basis, with control imaging tests and serological determination. It is recommended to continue follow-up for long periods. Recurrences of the disease are documented up to 10 years after apparently successful treatment has been applied3. The outcome of infection varies depending on the stage of the disease. Approximately 15% of patients are taken to surgery after 10 to 12 years of the initial diagnosis. 75% of these patients may remain asymptomatic.
Conclusion
Disseminated abdominal echinococcosis, although it is a rare pathology in our environment and the world literature, should always be suspected when clinical, imaging, and serological findings suggest it. It is important to identify this pathology to initiate timely medical management and subsequent surgical treatment for total resection of cystic lesions, if technically possible. Finally, the patient must remain in a strict follow-up and control to eradicate the disease adequately by means of medical treatment in prolonged cycles with albendazole.











 texto en
texto en