Introduction
Radiation esophagitis is a frequent complication due to exposure to radiotherapy, which manifests itself in treating certain types of cancer in advanced stages, such as lung and breast cancer1. However, this symptomatic erosive esophagitis requires a clinical, endoscopic, and histological assessment to confirm it because its manifestation is rare, affecting less than 1% of patients receiving radiotherapy2. Its pathogenesis is based on the effect caused by radiation on the basal epithelial layer, which reduces the mucosa and generates progressive denudation of the epithelium2,3. The acute manifestations of radiation esophagitis are dysphagia, odynophagia, and substernal discomfort, starting between two and three weeks after radiotherapy4. This paper aims to present the clinical and endoscopic manifestations of a patient with erosive esophagitis secondary to radiotherapy and to describe how this pathology was diagnosed.
Clinical case
We present the case of a 64-year-old woman with a two-week history of persistent burning chest pain of 10/10 intensity, predominantly in the epigastric region, radiating to the posterior area, and constantly associated with emetic episodes. She had symptoms of dysphagia and odynophagia, intolerance to oral solid and liquid foods, a history of type 2 diabetes mellitus (DM2), and moderately differentiated infiltrating lobular carcinoma. She underwent a right mastectomy in 2017, received tamoxifen therapy, and later in 2020, presented with chronic back pain and did not improve with analgesia. Consequently, she underwent an MRI of the thoracic spine, describing metastatic bone compromise near the sternum manubrium in the vertebral bodies of T11 and T12, the central region of the sacrum, and the sacroiliac joint. Two weeks prior, she received treatment with technical radiotherapy, extracranial radiosurgery near the T10-T12 dorsal column, doses/day of 700-2100 CGY, and chemotherapy with palbociclib, fulvestrant, and zoledronic acid.
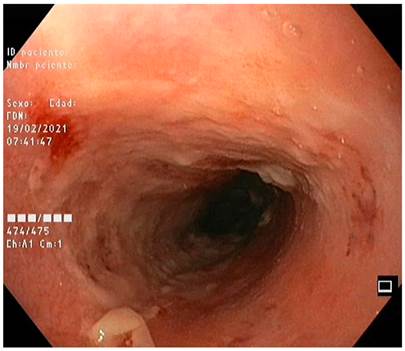
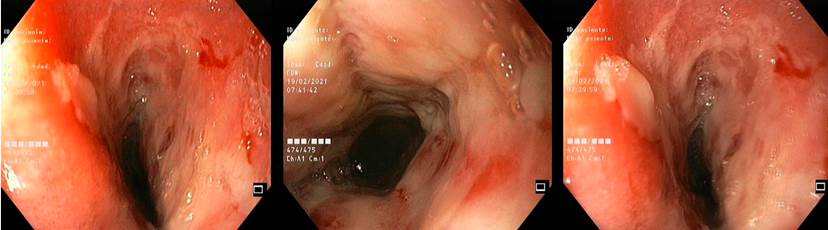
On physical examination, she was found to be tachycardic, hypotensive, with intense pain of the upper abdomen on deep palpation, and no signs of peritoneal irritation (heart rate [HR] 120 beats per minute [bpm], respiratory rate [RR]: 20 breaths per minute [rpm], blood pressure [BP]: 90/50 mm Hg). Complementary studies showed mild anemia, leukopenia, no hypoalbuminemia, renal function within normal limits (hemoglobin [Hb]: 9.8 mg/dL, leukocytes: 1,100, neutrophils: 700, creatinine: 1.9 mg/dL, and albumin: 4g/dL). Coagulation and liver profiles did not show alterations, as did troponin and electrocardiogram (ECG), so the coronary disease was ruled out. Upper gastrointestinal endoscopy reported the following: from 20 cm of the dental arch to the z line, multiple fibrin-covered circumferential ulcerations with easy bleeding on contact, Los Angeles-Savary Miller IV grade D erosive esophagitis, post-radiation esophagitis, and gastropathy chronic antral (Figures 1 and 2).
The patient was managed symptomatically for one week with parenteral proton pump inhibitors (PPIs) (omeprazole), antiemetics, sucralfate, analgesics with opioids, and intravenous fluids. She had a favorable clinical evolution.
Ethical considerations
The completion of the informed consent and its approval by the patient was carried out under Resolution 8430/1993.
Discussion
Erosive esophagitis after radiotherapy produces general damage to the epithelium, which is limited by the number of doses used in the radiotherapy section. Thus, the concomitant use of chemotherapy increases the risk of developing esophagitis, becoming complicated with stenosis six weeks after starting the event5. It is essential to bear in mind the incidence and severity of injuries caused by radiotherapy; the study by Maguire et al frequently described acute or late, but rarely severe, esophageal toxicities with high radiation levels without considering sociodemographic variables as prognostic factors6.
The clinical information on radiation esophagitis described in humans is minimal. The studies carried out by Northway et al on opossums made it possible to see that radiation generated ulcers at the level of the gastric mucosa and dose-response anorexia, which occurred seven to ten days after radiotherapy7. It is vital to consider the chronic complications of radiotherapy, which appear between one and eight months, such as a decrease in primary peristaltic waves, decreased function of the lower esophageal sphincter, and necrosis due to focal coagulation of the mucosa. However, a mouse model produced by Phillips and Ross showed simultaneous areas of epithelial denudation and regeneration one to two weeks after radiotherapy, which would suggest early tissue regeneration8.
In the study by Sasso et al, a case series with 29 participants was described after three weeks of radiotherapy treatment: 37% (n = 11) of the patients presented with esophagitis, which continued even after treatment for bronchial carcinoma9. Mascarenhast et al wanted to describe the incidence and nature of esophagitis in 38 patients who underwent radiation, resulting in endoscopic reports (esophagitis) similar to that described in the present case, considering that the patient received dual therapy for two weeks prior (radiotherapy and subsequent chemotherapy), which substantially increases the risk of developing the complication described in this article10.
The initial management of early complications is conservative, while endoscopic dilators for esophageal strictures are common in chronic cases. The way to prevent these difficulties is based on radioprotectors and inhibitors of the arachidonic acid metabolism pathway. The radiation modification can bring us closer to eliminating complications in normal esophageal tissue and improving the localized response in thoracic tumors5. Multiple pharmacological treatments have been proposed, such as nonsteroidal anti-inflammatory drugs (NSAIDs) and the prophylactic use of corticosteroids, in addition to nutritional support and treatment with PPIs or sucralfate to reduce mucosal exposure to the stimuli produced by radiotherapy, decreasing the risk of mucositis. Topical analgesics such as lidocaine slightly improve dysphagia, and antacids such as sucralfate may slightly improve food intake9,11.
Conclusion
Erosive esophagitis associated with radiotherapy has a very low incidence, and its clinical manifestations are rare. Diagnostic methods are practical, considering the history of cancer with radiotherapy to rule out its etiology virtually since endoscopy of the digestive tract plus biopsy is the first diagnostic tool. Treatment is mainly based on symptom control and the constant use of PPIs, strict diet control, and essential nutritional supplements because these patients have a high risk of malnutrition and a compromised health condition.











 texto en
texto en