Introduction
Retrorectal cystic hamartomas (tailgut cysts) are uncommon, multiloculated congenital tumors derived from embryonic post-anal or tail gut remnants. In the presacral space is the junction of the hindgut and neuroectoderm, and the totipotent cells found there can cause several types of tumors1. Retrorectal tumors are rare and have an incidence of approximately 1:40 0002. Cystic hamartomas are a small proportion of these retrorectal tumors, and most publications include one or a few cases. The largest published report is a series of 53 cases collected over 35 years by Hjermstad and Helwig at the Armed Forces Institute of Pathology. This issue highlighted that only 2 out of 53 cases were accurately diagnosed from the outset3. Cystic hamartomas are located in the retrorectal space or anterior sacral space. The upper limit is the perianal skin fold; the lower limit is the levator ani and, laterally, the ureters and iliac vessels2.
Although found at any age, most cystic hamartomas are more frequent in women between 40 and 60 (3:1 ratio). They are multicystic and frequently asymptomatic (26%-50%), but some patients present with symptoms including rectal prolapse, tenesmus, constipation, urinary symptoms, retrorectal abscess, and low abdominal pain4,5. If not removed early, the most common complications include infection, fistula development, and malignant transformation. Congenital lesions are two-thirds of presacral tumors, including developmental cysts, sacral meningocele, cystic lymphangioma, sacral chordoma, and teratomas1,6.
Surgical excision with negative margins is the definitive treatment. Due to its location, posterior surgery has been the most frequent, but laparoscopic and minimally invasive transanal surgeries have also been reported7,8.
Case presentation
A 21-year-old male patient was evaluated in 2018 for a perineal abscess that drained to the skin and remained with an intermittent outflow of seropurulent material. A perianal fistula was found during the examination. He brought a colonoscopy in which a secondary anal fistula orifice was reported at the right anterolateral level and 3 cm from the anal margin, in addition to two rectal polyps resected with polypectomy loop and the rest colonoscopy up to the distal ileum was normal. The pathology showed that they were juvenile polyps in the rectum. Additionally, he brought a soft tissue ultrasound that showed a fistulous tract at the right lateral level. The patient was referred for surgery, but he was unable to do it at that time. He was assessed 3 months later, and two secondary orifices were found at the right anterolateral and posterolateral levels. When the surgery was performed a month later an abscess was also found which was drained during the procedure.
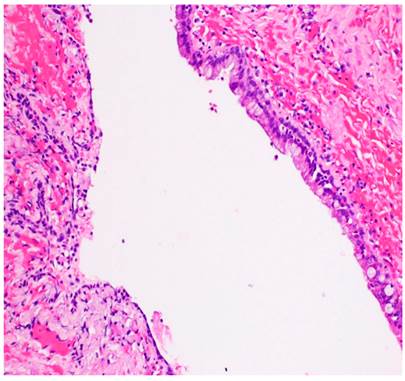
Postoperatively, the surgical wound failed to heal, and a mass was palpated 5 cm from the anal margin. Magnetic resonance of the pelvis showed a retrorectal multilobulated lesion extending to S-4 without involving the sacral bone in contact with the rectum, possibly a cystic hamartoma, and persistence of a fistulous tract at the right posterolateral level (Figure 1). In June 2019, he was taken to surgery, and the lesion was resected posteriorly (Kraske-Mason), and a fistulectomy was performed. Involvement of the rectal mucosa was found, so a colostomy was performed to protect it, which was closed 3 months later. Pathology indicated fragments of fibroconnective stroma with central cavitated lesion with extensive areas lined by epithelium alternating between squamous and columnar. In some areas devoid of epithelium, there was a dense inflammatory infiltrate, predominantly lymphohistiocytic (Figures 2 and 3). Currently, the patient has no evidence of relapse and has good continence.
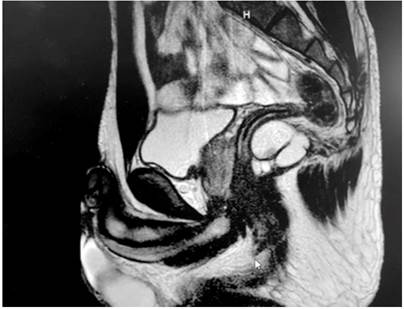
Figure 1 Retrorectal cystic lesion. The midline measures 5.7 cm anteroposterior x 3.6 cm x 4.2 cm, multiloculated with complete partitions and high signal intensity content in T1 sequences.
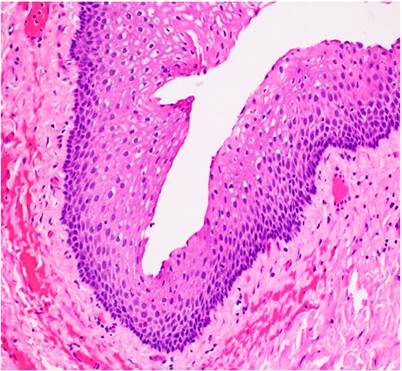
Figure 2 Retrorectal cystic hamartoma. The image shows the cyst wall area covered by stratified squamous epithelium resting on a fibroconnective stroma. Hematoxylin and eosin (H&E) stain. 20X magnification.
Discussion
Although the origin of the retrorectal cystic hamartoma is unknown, the lining cells and its location in the presacral space led to the hypothesis that it originates in the remnant of the tail of the hindgut. Between 28 and 35 days of embryogenesis, the embryo possesses a true tail, and the hindgut extends into this tail, hence the name tailgut for this entity. The intestine is distal to the future anus and normally undergoes involution later in embryogenesis. A remnant of this structure is thought to result in cystic hamartoma9.
The differential diagnosis of cystic hamartoma includes epidermoid cysts, dermoid cysts, duplication cysts, and cystic teratomas. The underlying epithelium in the epidermoid cyst is a stratified squamous epithelium. Skin remnants on the cyst’s wall are found in the dermoid cyst. In rectal duplication, the cysts are covered by the intestinal mucosa, there are crypts and villi, smooth muscle is found in their wall, and they are not multiloculated. Cystic hamartomas are multilocular; the underlying epithelium is cylindrical, transitional, squamous, or a combination thereof, with or without a stratified squamous component. Dispersed bundles of smooth muscle fibers are generally found on the wall of the cysts, but no submucosal or myenteric neural plexus is found3,10,11.
Magnetic resonance imaging is the cornerstone for diagnosis and surgery planning. In magnetic resonance imaging, a cystic hamartoma shows a low-intensity signal in T1 and a high-intensity signal in T2, although this may vary if the content is proteinaceous, hemorrhagic, or mucinous. Magnetic resonance imaging is useful for differentiating retrorectal cystic lesions and predicting malignancy4.
Complete surgical resection of retrorectal cystic hamartomas is recommended to decrease complications such as recurrence, infection, rectal fistula formation, bleeding, and malignant transformation. Malignant degeneration occurs between 2% and 13%, and the most frequently found tumors are adenocarcinomas, squamous carcinomas, neuroendocrine tumors, and sarcomas7,12.
The surgery approach is based on the size of the tumor and the correlation with the pelvic floor (levator ani). The posterior approach is enough for infra-elevator tumors. For supralevator tumors, the above approach is necessary. The posterior approach is enough for cysts with infra- and supralevator extensions if they are small (< 5 cm). The anterior approach is advised when the cysts are between 5 and 10 cm. Cysts larger than 10 cm may be dumbbell-shaped multilocular, so a combined approach13) is recommended. Laparoscopic7 or robotic14) resections have also been attempted, as well as endoscopic transanal microsurgery15. Surgery complications include delayed healing, pelvic floor, and sexual dysfunction. Complications are minor in the posterior approach12.
Conclusion
Retrorectal space tumors are rare and heterogeneous due to the diversity of tissues arising from embryonic remains in this topography. Given the lack of guidelines and paucity of information in the literature, this report aims to emphasize the importance of considering hindgut cyst as a differential diagnosis for presenting symptoms for earlier diagnosis and avoiding progression to carcinoma.











 text in
text in