The online Merriam-Webster dictionary defines dogma as “something held as an established opinion, especially: a definite authoritative tenet.” In other words, it is a concept or doctrine held by religion or other authorities which does not admit replication or doubt and, therefore, is exempt from being subjected to evidence of veracity1. Life, sciences, and medicine are full of these concepts. However, as Paul Valéry said, “That which has been believed by everyone, always and everywhere, has every chance of being false.” The dogma to which we will refer in this article is the one that held for many years that the stomach was a sterile organ due to the action of hydrochloric acid and, consequently, bacteria cannot normally grow inside it. Over the millennia, as knowledge and science have progressed, evidence has shown that “[...] ignorance is less remote from the truth than prejudice.”, as Denis Diderot put it. A prejudice or a belief makes an adequate and correct interpretation of reality impossible; it is like seeing through a colored lens: “[...] everything seems to be that color.” Conversely, ignorance about something will cease once the problem is studied and the necessary knowledge is acquired.
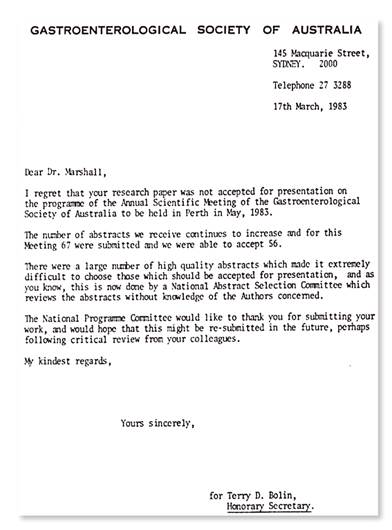
On June 11, 1979, Professor Robin Warren, pathologist at the Royal Perth Hospital in Australia (Figure 1), described his first case of bacteria associated with chronic gastritis2.
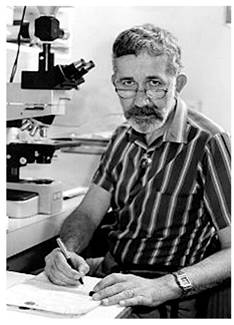
Figure 1 Dr. Robin Warren, Department of Pathology, Royal Perth Hospital Australia. Source: https://www.nobelprize.org/prizes/medicine/2005/warren/biographical/
After examining a gastric biopsy, he concluded that the specimen contained “[...] chronic gastritis with minor erosion and that the quality of the mucosal surface in many areas seemed slightly more inflamed than normal and contained numerous bacteria in close contact with the epithelium, which was Campylobacter-like and appeared to be actively growing and did not appear to be contaminants2.”
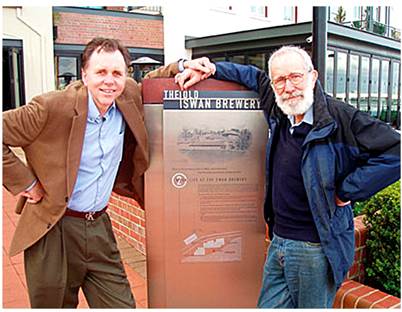
Like every scientist, Dr. Warren was honest in admitting that not everything was clear to him and acknowledged that “[…] I did not know the meaning of these unusual findings but considered that they deserved further research regarding eating habits, gastrointestinal function, and microbiology.” The finding and repeated reporting of such findings prompted two endless questions from attendees of the clinical-pathological meetings: 1) why do you insist it is the primary infection and not those considered secondary to inflammation, and 2) if they are there, why had they not been seen before? At that time, he did not have clear and correct answers to such questions. For the first question, it was necessary to wait for Barry Marshall to demonstrate the effects of antibiotics on these infections eventually. As such alterations were studied, findings progressively showed that there were reports from the previous century describing bacteria in the stomach, too. Still, such findings were considered incorrect and unimportant because the main concept was that “the stomach was sterile2.” Nowadays, many scientific comments and interpretations can be made about these significant findings. Still, an in-depth reflection would also be what Winston Churchill once said: “Men occasionally stumble over the truth, but most of them pick themselves up and hurry off as if nothing had happened.” No one believed Professor Warren’s findings except Win, his wife -a psychiatrist. She encouraged him to continue his research and disregard the disqualification of public opinion. Thus, an obligatory question at this point is, who has not had the world against them, even over the most elementary ideas and concepts? Later, in 1981, Marshall, already an internal medicine resident, would come to his gastroenterology clerkship and be assigned to rotate with Dr. Warren, “a pathologist who was interested in following up on some bacteria that were in the stomach,” although the actual words were “one of our pathologists who is trying to pin gastritis on a bacterial infection” (Figure 2).
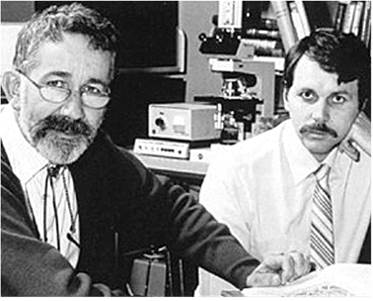
Figure 2 Robin Warren, on the left, Barry Marshall, on the right, July 1984. Source: https://www.nobelprize.org/prizes/medicine/2005/warren/biographical/
Marshall initially doubted the importance of the project. Dr. Warren could not convince him and asked him to read the protocol and forget what the public thought about “gastritis” before continuing to question it. Barry Marshall read the document and finally agreed to start the investigation with 20 patients undergoing additional antral mucosa biopsies, apparently normal to endoscopy. What would a teacher of today think if a second-year resident of internal medicine, based on old prejudices, contradicts without any evidence a protocol that was based on serious observations of an exemplary pathologist like Dr. Warren? That attitude reflects Bertrand Russel’s claim: “The trouble with the world is that the stupid are cocksure and the intelligent full of doubt!”
Once this pair of “quixotes” agreed and decided to undertake the research, arguments appeared from the gastroenterologists who performed the endoscopies, who considered that “the idea of sending gastric biopsies for culture was ridiculous,” “since the goal of gastroenterology and endoscopy was patient care and not esoteric research projects.” Moreover, “no one in many centuries had cultivated stomach bacteria” and, therefore, “it did not make sense for a rational gastroenterologist to take biopsies to look for bacteria.2” Thanks to Marshall’s constant insistence on the microbiology department and the high scientific qualities of the members of that great laboratory -who on multiple occasions modified the culture media and incubation temperatures, at last, the 35th culture was successful and showed bacteria! In fact, the department members had forgotten that culture and mistakenly left it incubating during the Easter festivities, which take five days in Australia. After the holidays, they returned to the laboratory, and on April 14, 1982, they found the typical colonies of Helicobacter pylori (H. pylori)3. Many skeptics and ill-intentioned critics initially considered this achievement as something fortuitous, by chance, and considered it serendipity, or as the jargon has it, “a sheer stroke of luck”. However, if analyzed thoughtfully, the correct conclusion would probably be the one masterfully formulated by Louis Pasteur in his time: “Chance favors the trained mind.”
Despite this interesting discovery, finding “bacteria that could cause chronic active gastritis,” Marshall and Warren -the authors, had not agreed on how they should communicate their findings to the scientific community, nor on the terms in which they should highlight them. They went to Professor Armstrong from the Electron Microscopy Unit of the Royal Perth. This magnificent scientist advised them to write two separate letters to the editor of the Lancet journal4, and so they did5,6. The hardest battle against the world’s disbelief would come from that moment on. In 1983, the Gastroenterological Society of Australia rejected the first work they did in which they demonstrated that H. pylori was more frequently associated with mucosa with chronic gastritis than with normal mucosa (p = 0.001), as well as with duodenal ulcers (p = 0.01), but not statistically significant with gastric ulcers (p = 0.05). Today, we have several explanations for these associations. That work was possible thanks to Dr. Warren’s interest in calculators. However, it was quite an odyssey for him to manage an advanced calculator and interpret the statistical significance of the “p” in that rudimentary “gadget” for our times. Sixty-seven papers were submitted to the Australian congress, and the 56 best papers were selected. Warren and Marshall’s work was in the bottom 11. At the end of the rejection letter were words of courtesy, “appreciating the effort and encouraging them to continue investigating and pursuing better quality research” (Figure 3).
Then there would be multiple studies with interesting findings, such as the recurrence of duodenal ulcers, more frequently in those who had no cure for H. pylori5, and the bactericidal activity of bismuth for Campylobacter pyloridis7. That initial name given to the microorganism was considered grammatically incorrect since, similarly, we do not say “Escherichia colitis” but “Escherichia coli.” At a world congress, it was renamed as it is currently known8. Faced with the worldwide disbelief that a bacterium produced gastritis, Marshall ingested a supernatant with H. pylori to show that it did produce it and thus convince the world that it was not really “a tall tale9”. Marshall continued to conduct multiple studies related to the diagnosis and treatment of the microorganism10-16. He developed the rapid urease test (RUT) and the urea breath test (UBT)10,16. He demonstrated that eradication in patients with peptic ulcers decreases the probability of recurrence6. Despite the high-quality evidence that H. pylori cure means ulcer cure, the scientific community remained skeptical until research by Dr. Graham, published in the Annals of Internal Medicine, confirmed Marshall and Warren’s findings17. Such an important work, conducted by a scientist of Dr. Graham’s stature, meant “a blessing”. From that time on, the world was convinced about the story. Since then, this microorganism progressively became one of the most transcendental discoveries in gastroenterology, revolutionizing the concept of peptic ulcers and, finally, the etiology of gastric cancer. Thus, providing the possibility of preventing it if the infection is cured. In 2005, the Swedish Academy awarded the Nobel Prize in Physiology and Medicine to Warren and Marshall for discovering the causal relationship of H. pylori with chronic gastritis and peptic ulcers (Figure 4).
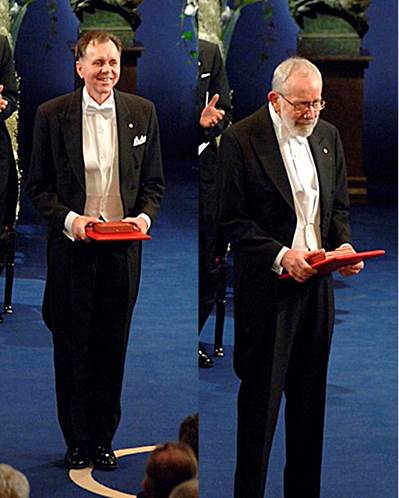
Figure 4 Left: Barry Marshall received the Nobel Prize in Physiology and Medicine in 2005. Right: Robin Warren receiving the Nobel Prize in Physiology and Medicine in 2005. Source: https://www.nobelprize.org/prizes/medicine/2005/marshall/photo-gallery/ y https://www.nobelprize.org/prizes/medicine/2005/warren/photo-gallery/
No one could have imagined that two clinical doctors with no master’s or doctoral degrees or epidemiology studies would be awarded a Nobel Prize for clinical research. This should set an example for all researchers and our undergraduate and graduate students. They should also prompt reflection for many ethics committees in the underdeveloped world that eliminate research protocols and thereby annihilate the ambitions of many young researchers who are taking their first steps in research. This momentous discovery, in my opinion, was the prologue to an overwhelming story whose contemporary reach is absolutely shocking and fascinating.
Many researchers before Marshall and Warren had observed microorganisms in the stomach. They linked them to chronic gastritis, although the causal relationship could not be demonstrated due to the impossibility of culturing them. Dr. Steer was probably the closest to achieving this discovery18-20. However, the culture of his biopsies grew Pseudomonas aeruginosa. Manifold reflections might arise from this amazing story, but this commentary would take too long. I believe that the strongest lessons might include: “absence of proof is not proof of absence” and “he who has faith in himself does not need others to believe in him.” Besides, it is essential to work as a team because, as the letter to the Corinthians states, “the body is not made of one part but of many,” or as Thomas Buxton said, “With ordinary talent and extraordinary perseverance, all things are attainable;” finally, “failures and difficulties should be reasons to keep trying.” For instance, who is not aware of Abraham Lincoln’s many failures, and who became President of the United States after multiple attempts and failures? Moreover, Steve Jobs founded Apple and was expelled from that company. Undoubtedly, “Man discovers himself when he measures himself against the obstacle!” Difficulties are the best stimulus for leaders and the bane of the fainthearted. Regarding leadership, scientific leaders are absolutely persevering and are not concerned about what public opinion thinks, which makes them completely different from politicians. Lastly, teachers are friends with students and can win a Nobel Prize together! (Figures 5 and 6).











 texto en
texto en