Introduction
In 2010, the American Society for Gastrointestinal Endoscopy (ASGE) proposed a series of criteria to classify patients with suspected choledocholithiasis according to the probability of having or not having stones in the bile duct; high risk means a probability > 50%, medium risk between 10% and 50%, and low risk < 10%1. Over the years and the publication of several studies that demonstrated that by following these criteria, the rate of non-therapeutic endoscopic retrograde cholangiopancreatography (ERCP) was around 20%-30%2-7, the ASGE decided to update the guidelines and published its new proposal in 20198. The main objective of this modification is to reduce the diagnostic ERCP rate as much as possible, to avoid exposing patients to risks and complications of endoscopic management, such as acute pancreatitis, bleeding, and perforation, among others9. However, the change significantly increased patients with medium probability, which involves imaging them to assess the bile duct before requesting ERCP. Many health institutions in Latin America do not have availability or timely access to this type of study, which could create the need to refer patients and, in turn, increase the days of hospital stay with the consequent increase in complications secondary to delay in the procedure and, probably, the impact on health care costs.
Our objective was to analyze the risk stratification for choledocholithiasis in a hospital in southwestern Colombia and compare the performance of high probability variables according to the ASGE 2010, as updated in 2019, in our patients.
Materials and methods
A retrospective cohort study was carried out on all patients older than 14 with suspected choledocholithiasis taken to ERCP at the San José University Hospital (HUSJ) in Popayán between January 2016 and December 2018. This institution performs around 900 laparoscopic cholecystectomies and 300 ERCPs per year.
We excluded (a) patients undergoing ERCP with a diagnosis of choledocholithiasis by magnetic resonance cholangiopancreatography (MRCP), endoscopic ultrasonography (EUS), contrast-enhanced abdominal tomography (CT) or previous ERCP; (b) failed ERCP (inability to channel the bile duct); (c) other causes of bile duct obstruction (neoplasms, benign strictures, parasites, among others); (d) ERCP for other causes (management of biliary fistulas, replacement of endoscopic prostheses, among others), and (e) incomplete medical records.
On the one hand, a patient is considered to have a high probability, according to the ASGE 2010, when having a very strong predictor (ultrasound bile duct stones, ascending cholangitis, serum bilirubin > 4 mg/dL) or both strong predictors (bile duct dilated, serum bilirubin 1.8-4 mg/dL). On the other hand, according to the ASGE 2010, the medium probability would occur in case of a strong predictor or at least a moderate predictor (altered liver function tests, age older than 55 years, gallstone pancreatitis).
In 2019, by modifying the criteria, patients with bile duct stones on ultrasound or other imaging, symptoms of ascending cholangitis, or bilirubin > 4 mg/dL with dilated bile duct were considered to have a high probability. Medium probability would involve abnormal liver function tests other than bilirubin, age > 55 years, or dilated bile duct on ultrasound or other imaging (acute pancreatitis of biliary origin is dismissed).
We requested the medical record numbers registered in the HUSJ Dynamics system of all patients with a CUPS code for ERCP performed between 2016 and 2018. The information was collected through the electronic form CLINAPSIS®. This study had the ethical endorsement of the HUSJ, Minutes No. 05/2019.
Measures of central tendency and dispersion were obtained for the quantitative variables. The frequencies for the qualitative variables were exposed. With the information obtained, we created univariate analysis tables to summarize the characteristics of the included population. Sensitivity, specificity, positive (PPV), negative (NPV) predictive values, and accuracy were calculated. We employed the statistical software SPSS v. 25 (Statistical Product and Service Solutions) for the analysis.
Results
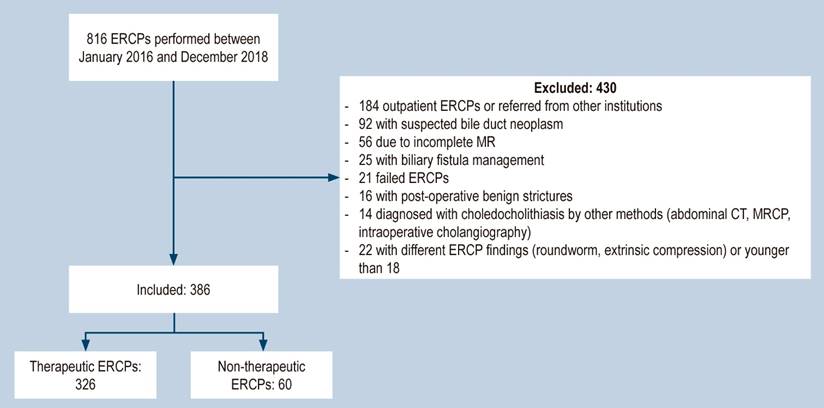
During the 2016-2018 period, 816 ERCPs were performed at the institution, of which 386 met the inclusion criteria (Figure 1). Of the total number of patients, 54.1% were women, the mean age was 59.4 years, and 26.4% (n = 102) had a surgical history of cholecystectomy (Table 1).
Table 1 Characteristics of patients taken directly to ERCP for suspected choledocholithiasis
| n | % | |
|---|---|---|
| Female | 209 | 54.1 |
| Mean age (SD) | 59.4 (20.9) | - |
| Previous cholecystectomy | 102 | 26.4 |
| Clinical and paraclinical assessment | ||
| Acute pancreatitis of biliary origin | 76 | 19.7 |
| Cholangitis, according to Tokyo 2018 | 107 | 27.7 |
| TB < 2 | 61 | 15.8 |
| TB 2-4 | 83 | 21.5 |
| TB > 4 | 242 | 62.7 |
| Altered liver profile other than TB | 373 | 96.6 |
| Abdominal ultrasonography findings | ||
| Acute cholecystitis | 116 | 40.8 |
| Cholelithiasis | 237 | 83.5 |
| Choledocholithiasis | 160 | 41.5 |
| Dilated bile duct | 294 | 76.2 |
| ERCP findings | ||
| Days since admission to ERCP (mean SD) | 2.6 | - |
| Therapeutic ERCP | 326 | 84.5 |
| Choledocholithiasis | 327 | 84.7 |
| Dilated bile duct | 349 | 90.4 |
| Bile duct size (mm) (SD) | 12.8 (5.8) | - |
| Post-ERCP complications | ||
| Pancreatitis | 4 | 1.0 |
| Digestive bleeding | 1 | 0.3 |
| Duodenal perforation | 0 | 0 |
Source: The authors.
Accordingly, 19.7% of the patients presented with acute pancreatitis of biliary origin, and 27.7% were diagnosed with acute cholangitis based on the Tokyo 2018 criteria10. It was found that 62.7% had total bilirubin (TB) > 4 mg/dL, 21.5% had TB between 2 and 4 mg/dL, and 18.8% had values less than 2 mg/dL. Besides, 96.6% of the patients had liver profile abnormalities other than bilirubin (transaminases: aspartate aminotransferase [AST], alanine aminotransferase [ALT], and alkaline phosphatase) (Table 1).
Abdominal ultrasonography findings reported acute cholecystitis in 40.8% of patients, gallbladder lithiasis in 83.5%, and bile duct stones in 41.5%. Patients who presented with biliary sludge in the gallbladder and bile duct were included in the cholelithiasis and choledocholithiasis groups, respectively. Also, 76.2% had a dilated bile duct, considered > 6 mm in patients with gallbladder and > 8 mm with a history of cholecystectomy (Table 1).
The mean time from patient admission to ERCP was 2.6 days (standard deviation [SD] ± 2.6); 90.4% had a dilated bile duct, with a mean size of 12.8 mm (SD ± 5.8), according to the endoscopic report. Choledocholithiasis was detected in 84.7% of the patients undergoing ERCP, and 84.5% of the ERCPs were therapeutic since one of the patients had intrahepatic lithiasis, where endoscopic management was not possible. The total number of complications was 1.3% (n = 5): two severe pancreatitis cases, two mild pancreatitis cases, and one gastrointestinal bleeding without needing blood products or reintervention (Table 1).
The diagnostic yield of tests was calculated for patients with a high probability according to the ASGE 2010 and 2019 criteria. The most sensitive variable was bile duct dilation, with a sensitivity of 81%, followed by TB > 4 mg/dL (64%), and PPVs of 89.9% and 86.4%, respectively. Choledocholithiasis on ultrasound and symptoms of cholangitis were the most specific variables to detect bile duct stones, with specificities of 78.3% and 78.3% and PPVs of 91.9% and 87.9%, respectively. The patients who presented with cholangitis, hyperbilirubinemia greater than 4 mg/dL, and choledocholithiasis on ultrasound had specificities of 96.7% and a PPV of 95%. The sensitivity of bile duct dilation with total bilirubin greater than 4 mg/dL was 51.5% with a specificity of 75%, PPV of 91.8%, and NPV of 22.2% with an accuracy of 47.2 % (Table 2).
Table 2 Diagnostic yield of the tests for high probability according to the 2010 and 2019 criteria
| Variable | n | Sen | Spe | PPV | NPV | Accuracy |
|---|---|---|---|---|---|---|
| Individual | ||||||
| CL on US | 147 | 45.1 | 78.3 | 91.9 | 20.8 | 38.1 |
| Cholangitis | 94 | 28.8 | 78.3 | 87.9 | 16.8 | 24.4 |
| Dilated BD | 264 | 81.0 | 50.0 | 89.8 | 32.6 | 68.4 |
| TB > 4 | 209 | 64.1 | 45.0 | 86.4 | 18.8 | 54.1 |
| TB 2-4 | 70 | 21.5 | 78.3 | 84.3 | 15.5 | 18.1 |
| Aggregate | ||||||
| Cholangitis + CL on US + TB > 4 | 38 | 11.7 | 96.7 | 95.0 | 16.8 | 9.8 |
| CL on US + TB > 4 | 95 | 29.1 | 90.0 | 18.9 | 94.1 | 24.6 |
| Dilated BD + TB > 4 | 168 | 51.5 | 75.0 | 91.8 | 22.2 | 47.4 |
| Dilated BD + TB 2-4 | 55 | 16.9 | 91.7 | 91.7 | 16.9 | 14.2 |
CL: choledocholithiasis; Spe: specificity; Sen: sensitivity; US: ultrasonography; BD: bile duct. Source: The authors.
Patients were divided into high probability (HP) and medium probability (MP) of having choledocholithiasis according to the ASGE 2010 and 2019 guidelines. We calculated the percentage of patients with choledocholithiasis on ERCP and how many met very strong, strong, and moderate criteria according to the 2010 ASGE. Accordingly, we found that, of the 386 patients taken to ERCP, 328 (84.9%) met high probability criteria, of which 283 (86.2%) had choledocholithiasis, 301 met very strong and 27 strong criteria. Fifty-eight (15.1%) patients had medium probability, of which 43 (74.1%) were positive for choledocholithiasis, and 48 met strong and ten moderate criteria. When categorizing the patients according to the ASGE 2019 guidelines, 271 (70.2%) were classified as high probability, of which 242 (89.2%) presented with choledocholithiasis, and all met very strong criteria according to the ASGE 2010 (Table 3).
Table 3 Patients with a high and medium probability, according to the ASGE 2010 and 2019 guidelines
| 2010 | 2019 | ||||
|---|---|---|---|---|---|
| Total n (%) | HP n (%) | MP n (%) | HP n (%) | MP n (%) | |
| Number of patients | 386 | 328 (84.9) | 58 (15.1) | 271 (70.2) | 115 (29.8) |
| LC on ERCP | 326 | 283 (86.2) | 43 (74.1) | 242 (89.2) | 84 (73.1) |
| Very strong criteria* | 301 (77.9) | 301 | NA | 271 | 30 |
| Strong criteria* | 76 (19.6) | 27 | 48 | NA | 76 |
| Moderate criteria* | 10 (2.5) | NA | 10 | NA | 10 |
*According to ASGE 2010 guidelines. CL: choledocholithiasis; ERCP: endoscopic retrograde cholangiopancreatography; NA: not applicable; HP: high probability; MP: medium probability. Source: The authors.
In our patient cohort, the sensitivity and specificity of high probability under the 2010 guidelines were 86.8% and 25.0%, respectively, with a PPV of 86.3% and a 77.2% accuracy. High probability, according to the 2019 guidelines, showed lower sensitivity (74%) but higher specificity (51.7%), a PPV of 89.3%, and an accuracy of 70.7% (Table 4).
Table 4 High probability diagnostic yield according to the 2010 and 2019 guidelines
| Variables | 2010 | 2019 | p |
|---|---|---|---|
| Patients with HP (n) (%) | 328 (84.9) | 271 (70.2) | < 0.001 |
| CL in patients with HP (n) (%) | 283 (86.2) | 242 (89.2) | < 0.001 |
| Sensitivity (%) | 86.8 | 74.2 | |
| Specificity (%) | 25.0 | 51.7 | |
| PPV (%) | 86.3 | 89.3 | |
| NPV (%) | 25.9 | 26.9 | |
| Accuracy (%) | 77.2 | 70.7 |
CL: choledocholithiasis; HP: high probability. Source: The authors.
Discussion
The clinical manifestation spectrum in patients with suspected choledocholithiasis is broad and variable, so surgeons rely on guidelines and criteria for decision-making. Due to the high rate of diagnostic ERCP (20%-30%) under the ASGE 20102, we analyzed the therapeutic ERCP rate according to the high probability of the 2010 and 2019 guidelines. When categorizing the patients according to the 2010 guidelines, 328 met the high probability criteria, and the diagnostic ERCP rate in this group was 13.8%; with the 2019 criteria, there were 271 patients, and the non-therapeutic ERCP rate was 10.8%. The 2019 criteria were applied to the 328 who went directly to ERCP to analyze both results due to high probability per the 2010 guidelines. In this scenario, 29 patients (8.8%) would have diagnostic ERCP, which translates into a 41.7% reduction in the non-therapeutic ERCP rate.
When examining the paraclinical and ultrasound variables individually, we found that choledocholithiasis on ultrasound and cholangitis had specificities greater than 78% and PPV > 88%, which are lower than those reported in other studies, such as the one published in China. It analyzed 2724 patients with suspected choledocholithiasis who underwent ERCP, diagnostic imaging, or surgical exploration of the bile duct and reported specificities of 89.6% with a PPV of 91%2. Moreover, a study in the United States retrospectively analyzed 744 patients undergoing ERCP with indications of choledocholithiasis and showed specificities of 97% and a PPV of 93.7%11. Although the diagnostic yield of these variables in the different studies is diverse, they continue to form part of the high probability criteria in the 2010 and 2019 guidelines, under which patients should go directly to ERCP.
One of the significant updates to the 2019 guidelines was removing TB > 4 mg/dL as the only variable and adding bile duct dilation to define ERCP performance. Our study found that bile duct dilation was more sensitive than TB > 4 mg/dL (81% vs. 64%) with similar specificities (50% vs. 45%, respectively). By combining both variables, lower sensitivity and higher specificity were observed with a PPV of 91.8%, and the 2019 guidelines’ objective of being more selective to reduce the rate of diagnostic ERCP was achieved. Our specificity was lower, and the PPVs were similar to the results of other research groups that reported specificities of 94%-96% and PPVs of 69%-85%11,12.
According to ASGE 2010, 86.2% of patients with high probability and 74.1% with medium probability were positive for choledocholithiasis. The 2019 criteria showed that 89.2% of patients with a high probability had bile duct stones compared with 73% of patients with a medium probability. Chandran et al.11 reported similar results (67.7% vs. 82.5%, respectively). While not statistically significant, they considered that they are clinically relevant to reduce the rate of complications of endoscopic management when performing further imaging studies.
During the study period, the institution did not have EUS or MRCP available, which is why 15% of the patients taken to ERCP did not meet high probability criteria according to ASGE 2010 and did not undergo any prior imaging study, as recommended by the guidelines. When analyzing these patients, the probability of having choledocholithiasis was 74.1% according to the 2010 guidelines and 73.1% according to the 2019 guidelines. These data were higher than in the guidelines, which suggest probabilities between 10% and 50%1, maybe because the majority met strong criteria, and only a small percentage met moderate criteria.
Few studies have compared the performance of patients classified as high-risk according to 2010 versus 2019 guidelines11-13. Hasak et al.12 reported that, when using the 2010 guidelines, the sensitivity, specificity, PPV, NPV, and accuracy were 50.5%, 78.9%, 82.5%, 44.8%, and 60.1%, respectively, while when using the criteria of the 2019 guidelines, the sensitivity, specificity, PPV and NPV, and accuracy were 65.8%, 78.9%, 86.3%, 54.1%, and 70.4%. In conclusion, although the 2019 criteria improve pretest performance, it is still in suboptimal ranges, and further EUS or MRCP-type studies should be considered before taking a patient to ERCP.
Chandran and colleagues11 demonstrated a significant difference in the number of patients classified as high risk: 37% under the 2019 guidelines versus 60% with the 2010 criteria. Sensitivity was 37.8% vs. 61.2%, specificity 77.1% vs. 52.1%, PPV 95.5% vs. 94.9%, and accuracy 40.3% vs. 60.6% when comparing both guidelines. They considered it necessary to carry out a cost-effective analysis when applying the 2019 guidelines due to the significant increase in patients in the medium category. Another group that recently compared both guidelines13 considers that the 2019 criteria reduce the number of diagnostic ERCPs and are a tool that improves risk stratification. Their data showed that the PPV increased by 79% according to the guides of 2010 to 83% according to those of 2019.
Our study obtained similar results when staging patients with the 2019 criteria. A lower number of patients were found in the high-risk category (70.2% vs. 84.9%), translating into much more specific criteria (51.7% vs. 25.0%) but less sensitive (74.2% vs. 86.8%) than those of the 2010 guidelines, considerably increasing the number of patients in the medium category. Accuracy was lower in the 2019 criteria (70.7% vs. 77.2%), a similar pattern to the previously mentioned studies. The PPV was higher in the 2019 guidelines (89.3% vs. 86.3%), with similar NPVs between both guidelines (26.9% vs. 25.9%).
Our ERCP complications were around 1%, well below what is mentioned in the current literature, reporting overall complications of 6%-15%, fatal complications of 1%-2%, and mortality of 0.4%14,15. This result should be taken with caution, as it could be due to underreporting of complications, probably related to not including intra-ERCP bleeding, complications related to sedation, post-ERCP sepsis, complications of the 430 excluded ERCPs, or late complications that could be cared for in another hospital. In addition, most complications, for being minor, could not be correctly noted in the medical record or not identified during data collection. In our institution, there are no trainees; therefore, all procedures were performed by experts with many years of experience, and the literature documents lower complication rates in expert hands16.
Our study has the limitations of being retrospective and single-center, which makes it susceptible to registration bias due to obtaining the data from medical records and restricts the generalization of results. In addition, it does not include all patients suspected of having choledocholithiasis, so an adequate measurement of the prevalence is not possible, especially of patients belonging to the medium probability category who were not taken for ERCP. Among its strengths, it is the first study that discusses the behavior of patients with choledocholithiasis taken to ERCP in the Cauca province, allowing the creation of guidelines that improve patient care at the San José University Hospital and motivate other institutions to conduct similar studies both in Cauca and in the rest of the country, as recommended by the Colombian Society of Gastroenterology.
Conclusions
Our results confirm that the new criteria for risk stratification and treatment of patients with suspected choledocholithiasis are less sensitive but more specific and become stricter when selecting patients who will be taken directly to ERCP so that the rate of non-therapeutic ERCP is decreased. However, the number of patients in the medium probability category increases considerably, which requires previous studies. Therefore, the implementation of the ASGE 2019 guidelines on the indications for ERCP should be considered in light of the resources of hospitals, especially in low- and middle-income countries. The ASGE 2010 guidelines show good sensitivity and accuracy in guiding ERCP performance.











 text in
text in